You're sitting on that crinkly paper in the exam room and the doctor asks, "Do you want the pill, the patch, or the IUD?" It’s treated like picking a flavor of gum. But the reality of how these hormones interface with your biology is way more complex than a three-minute consultation suggests. We need to talk about the effects of birth control because, frankly, the internet is full of either terrifying scaremongering or dismissive medical gaslighting.
It’s personal.
Most people start birth control for one of two reasons: they don't want to get pregnant, or their periods are a total nightmare. It works. The pill, specifically the combined oral contraceptive, has a failure rate of less than 1% when used perfectly. But "perfectly" is a high bar, and the trade-off involves a systemic shift in your endocrine environment. When you introduce synthetic versions of estrogen and progestin, you aren't just "turning off" your ovaries; you're changing the data stream your brain uses to communicate with your entire body.
The Brain-Body Connection and Mood
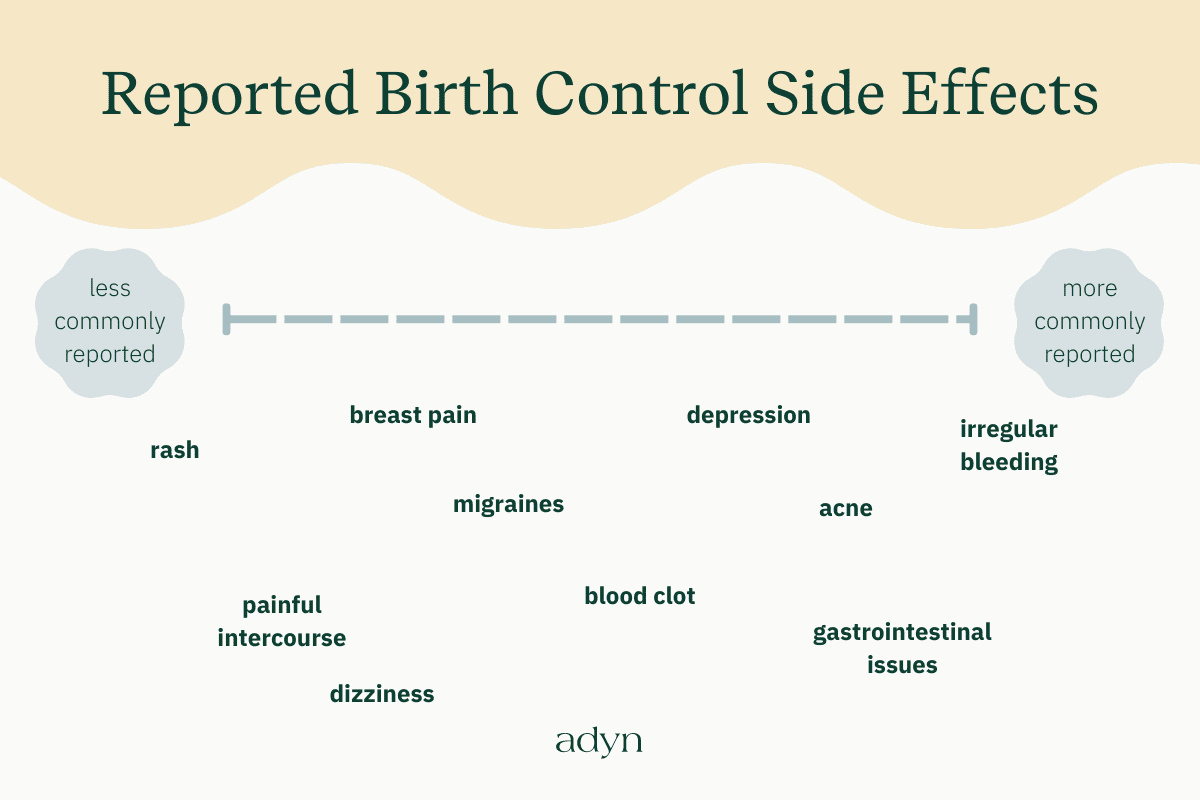
Let's get into the stuff people actually worry about at 2:00 AM. Mood. For years, women told their doctors, "I feel flat," or "I'm crying at car commercials," only to be told it was all in their heads. Then, a massive Danish study—we're talking over a million women—found a clear link between hormonal contraceptive use and a first-time diagnosis of depression.
It’s not just "moodiness."
Synthetic progestins, like levonorgestrel or medroxyprogesterone acetate (found in the Depo-Provera shot), can cross the blood-brain barrier. They mess with GABA receptors, which are basically the "brakes" for your nervous system. If those brakes aren't working right, you feel anxious, irritable, or just... gray. This isn't every user's experience, though. For some people with Premenstrual Dysphoric Disorder (PMDD), birth control is a literal lifesaver because it stops the hormonal roller coaster that causes suicidal ideation every month.
The effects of birth control on the brain are nuanced. It’s about your specific baseline. If you already have a history of depression, certain types of progestins might be a bad match for your chemistry.
✨ Don't miss: Why Do Women Fake Orgasms? The Uncomfortable Truth Most People Ignore
What Happens to Your Skin and Hair?
Everyone talks about the "pill glow." And yeah, it's real for a lot of people. If you have cystic acne caused by high androgens (male-type hormones like testosterone), the pill can be a miracle. It lowers your free testosterone and clears up your skin.
But there’s a catch.
What happens when you stop? Post-pill acne is a documented phenomenon where your oil glands, which have been suppressed for years, suddenly go into overdrive. It’s like a dam breaking. Then there's melasma—those dark, symmetrical patches on the face often called the "mask of pregnancy." Because birth control mimics certain hormonal states of pregnancy, your skin can become hypersensitive to the sun. You might end up with permanent pigment changes just from walking to your car.
Nutrients You’re Losing
This is the part that drives me crazy because it’s so easy to fix, yet rarely discussed. Hormonal contraceptives are "nutrient robbers."
- B Vitamins: Specifically B6, B12, and Folate. These are crucial for energy and mood.
- Magnesium: If you're getting leg cramps or migraines on the pill, check your magnesium levels.
- Zinc and Selenium: These are the heavy hitters for thyroid health and immune function.
If you’re on the pill, you basically need to be more aggressive about your nutrition than someone who isn't. You can't just "eat clean" and hope for the best; your body is burning through these cofactors faster because of the metabolic load of processing synthetic hormones through the liver.
The Big Fear: Blood Clots and Cardiovascular Health
We have to address the elephant in the room. The risk of venous thromboembolism (VTE).
🔗 Read more: That Weird Feeling in Knee No Pain: What Your Body Is Actually Trying to Tell You
It sounds scary because it is. Synthetic estrogens increase the production of clotting factors in the liver. For a healthy 20-year-old, the absolute risk is still very low—about 3 to 9 cases per 10,000 women compared to about 1 to 5 for those not on the pill. But those odds change fast if you smoke, have a BMI over 30, or have an underlying condition like Factor V Leiden.
If you see a doctor who doesn't check your blood pressure before handing over a script, run. High blood pressure is one of the most common cardiovascular effects of birth control, and it often goes unnoticed because we assume young people are "fine."
Weight Gain: Myth or Reality?
"Will this make me fat?"
It’s the number one question. The science is actually kind of annoying here because it says "no," but everyone's experience says "maybe." Large-scale reviews generally show no significant weight gain for most people on the combined pill. However, the Depo-Provera shot is a different story; it is consistently linked to weight gain in clinical studies.
For the pill or the IUD, what people usually experience isn't "fat gain" so much as insulin resistance or water retention. Synthetic progestins can make you more hungry. If you're hungrier, you eat more. If you eat more, you gain weight. It’s not the pill itself creating fat cells out of thin air, but it is changing the appetite signals in your hypothalamus.
The Long-Term View on Fertility and Cancer
One of the biggest misconceptions is that birth control "uses up" your eggs or makes you infertile. That’s just wrong. Your eggs are dying off every month anyway, whether you ovulate them or not. In fact, birth control can actually protect your fertility by reducing the risk of endometriosis and ovarian cysts, which can cause permanent scarring.
💡 You might also like: Does Birth Control Pill Expire? What You Need to Know Before Taking an Old Pack
As for cancer, it's a mixed bag.
The effects of birth control include a significantly lower risk of ovarian, endometrial, and colorectal cancers. We're talking a 30% to 50% reduction that lasts for decades after you stop taking it. On the flip side, there is a slightly increased risk of breast and cervical cancer while you're actively using it. Once you stop, that risk eventually returns to the baseline of someone who never used it.
It’s a game of trade-offs.
Why the "Period" on the Pill is Fake
You know that bleeding you get every month on the sugar pills? It’s not a period. It’s a "withdrawal bleed."
A real period is the result of ovulation. On birth control, you don't ovulate. The lining of your uterus doesn't thicken the same way. The bleed you experience is just your body reacting to the sudden drop in synthetic hormones. This is why many people choose to skip the placebo week entirely and just not bleed. Medically, there is no reason you need to have that withdrawal bleed, but the inventors of the pill added it in the 1960s to make the process feel more "natural" to users and the Catholic Church.
Navigating the Choices
If you’re feeling overwhelmed, that’s normal. You aren't just choosing a contraceptive; you’re choosing a hormonal profile.
If you want to avoid systemic effects, the copper IUD (ParaGard) is the gold standard because it’s non-hormonal. But, it can make your periods heavier and crampier. It’s a "pick your poison" situation. If you struggle with heavy bleeding, a hormonal IUD like Mirena keeps the hormones localized in the uterus, so much less of it hits your bloodstream compared to the pill.
Actionable Steps for Your Health
If you are currently using or considering birth control, don't just "set it and forget it."
- Track Everything: Use an app or a paper journal to track your mood, skin, and energy levels for at least three months. You won't notice subtle changes day-to-day, but you will notice the trend line.
- Supplement Smarter: Talk to a healthcare provider about a high-quality B-complex, magnesium glycinate, and zinc. This helps mitigate the "nutrient robbing" effect.
- Monitor Blood Pressure: Buy a cheap home cuff. Check it once a month. If it starts creeping up, that’s a signal your body isn't vibing with that specific formulation.
- Demand a Full Panel: Before starting, ask for a blood test to check your baseline lipids and glucose. Some people have a genetic predisposition that makes them more likely to develop insulin resistance on certain pills.
- Listen to Your Gut: If you feel "off," you are probably right. There are dozens of different progestin types. Sometimes switching from a "third-generation" pill to a "second-generation" one makes all the difference in the world.
The effects of birth control are neither all good nor all bad. They are a tool. And like any tool, the more you understand how it works, the less likely you are to get hurt by it. You deserve a healthcare experience that treats your hormones as the complex, vital messengers they are, not just a switch to be flipped.