Walk into any airport, grocery store, or high school football game in the United States, and you’ll see it. It’s not just a "feeling" anymore. It’s the data. Honestly, looking at the percentage of americans who are overweight or obese feels a bit like watching a slow-motion train wreck where everyone is also trying to sell you a snack.
According to the latest data from the Centers for Disease Control and Prevention (CDC) and the National Health and Nutrition Examination Survey (NHANES), the numbers are staggering. We aren't just talking about a few people carrying a little extra holiday weight. We are looking at a collective shift in human biology across an entire continent.
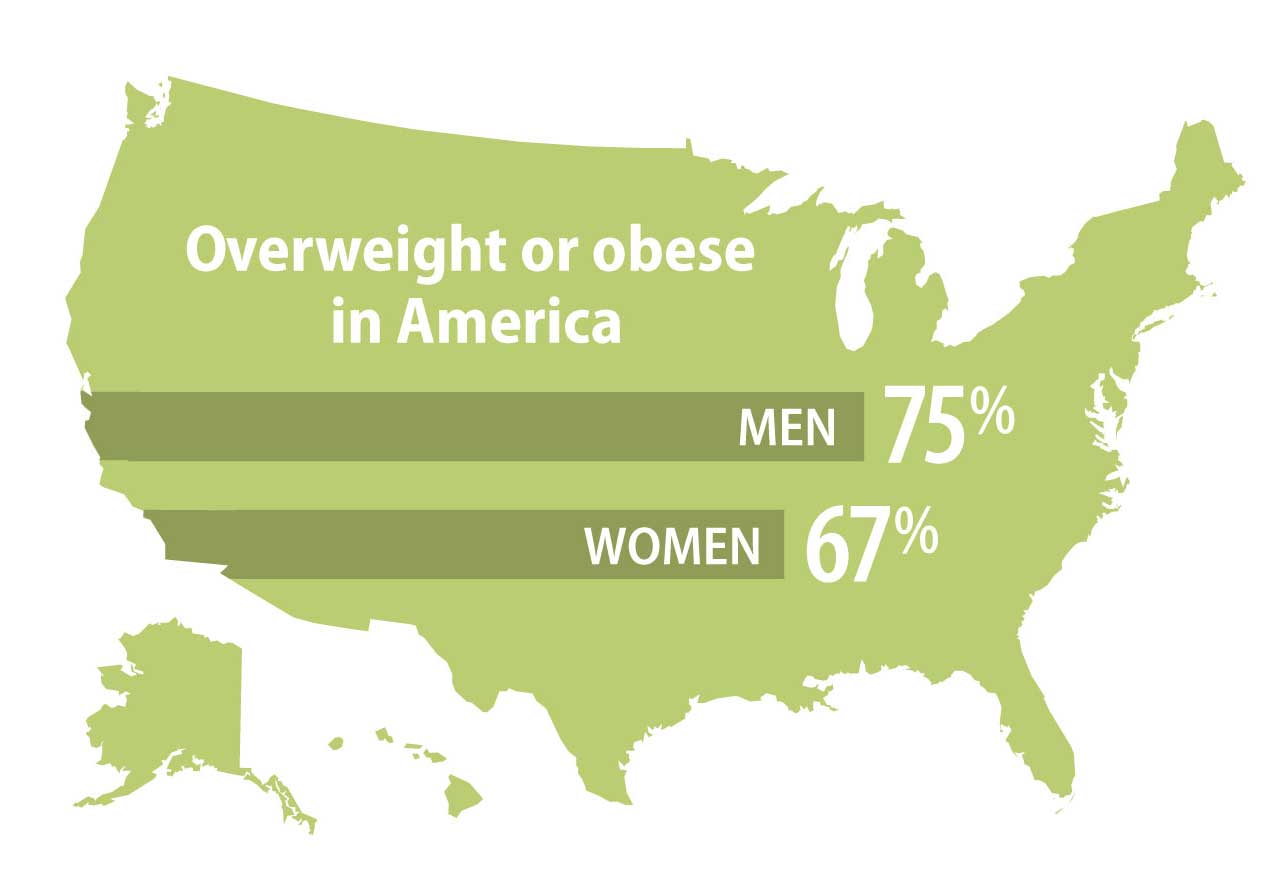
The reality? About 73.6% of adults over the age of 20 are considered either overweight or obese.
Think about that for a second. If you’re standing in a room with four people, three of them are likely struggling with their weight relative to clinical standards. It’s basically the new normal. But "normal" doesn't mean "healthy," and the nuance between being overweight and being obese matters a lot for how we talk about public health and personal longevity.
Breaking Down the Percentage of Americans Who Are Overweight or Obese
When we talk about this, we have to use Body Mass Index (BMI). Is it perfect? No. It’s a 200-year-old math equation that doesn't know the difference between a bodybuilder’s bicep and a sedentary person's midsection. But for large populations, it's the yardstick we have.
The CDC defines "overweight" as a BMI between 25 and 29.9. "Obese" is a BMI of 30 or higher.
When you peel back the layers of that 73.6% figure, the "obese" category alone accounts for roughly 41.9% of the population. That’s a massive jump from where we were in the late 1990s when the obesity rate was closer to 30%. We’ve added ten percentage points to the obesity tally in just over two decades. It’s fast. Too fast.
The Regional Divide: Where the Numbers Spike
It’s not the same everywhere. If you live in Colorado, you might feel like everyone is out hiking and eating kale. Colorado consistently reports the lowest obesity rates in the country, often hovering around 25%. Compare that to states like West Virginia, Mississippi, or Alabama, where the obesity rate frequently clears 40%.
✨ Don't miss: 2025 Radioactive Shrimp Recall: What Really Happened With Your Frozen Seafood
Why the gap?
- Economic factors: It is often cheaper to buy a 2,000-calorie bag of processed snacks than a fresh salad.
- Infrastructure: Some cities are built for cars, not people. If you can't walk to the store, you won't.
- Culture: Food is love in many parts of the country, and that love is often fried.
Why the Trend Lines Keep Moving Up
We like to blame willpower. We love to tell people to just "eat less and move more." But if it were that simple, would the percentage of americans who are overweight or obese be climbing every single year? Probably not.
Our environment is basically "obesogenic." That’s a fancy word researchers like Dr. Kevin Hall at the NIH use to describe a world designed to make us gain weight. We have ultra-processed foods that are engineered to bypass our "I'm full" signals. These foods—think boxed cereals, frozen pizzas, and sugary sodas—make up about 60% of the calories Americans consume.
They are hyper-palatable. They are cheap. They are everywhere.
Then there’s the activity side of things. Most of us sit at desks. We commute in cars. We relax by looking at screens. Even if you hit the gym for 45 minutes, it’s hard to outrun 23 hours of relative stillness.
The Medical Complexity
Obesity isn't just "carrying extra weight." It's a chronic disease. The American Medical Association (AMA) officially recognized it as such in 2013, which was a huge turning point.
When body fat reaches a certain level, it stops being passive storage and starts acting like an organ. It sends out inflammatory signals. It messes with insulin. It stresses the heart. This is why we see a direct correlation between the rising weight of the country and the prevalence of Type 2 diabetes and hypertension.
🔗 Read more: Barras de proteina sin azucar: Lo que las etiquetas no te dicen y cómo elegirlas de verdad
The Economic Gut Punch
This isn't just a health issue; it's a massive drain on the economy. Recent estimates suggest that the annual medical cost of obesity in the U.S. is nearly $173 billion. People with obesity generally have medical costs that are over $1,800 higher than those at a healthy weight.
Who pays for that? Everyone. It shows up in higher insurance premiums, taxpayer-funded programs like Medicare, and lost productivity at work.
Misconceptions We Need to Address
There is a lot of noise in this space. One of the biggest myths is that you can't be "fat but fit." While it’s true that some people with a high BMI have great cardiovascular health, the long-term data suggests that weight eventually catches up with the joints and the metabolic system.
Another big one? The idea that it's all about genetics. Yes, genetics load the gun. But our environment pulls the trigger. Your genes haven't changed in the last 40 years, but the percentage of americans who are overweight or obese has skyrocketed. That means it's the world around us—the food, the stress, the sleep deprivation—that's doing the heavy lifting.
The GLP-1 Factor: A New Era?
We have to talk about the "Ozempic effect." Medications like semaglutide and tirzepatide are changing the conversation in real-time. For the first time, we have drugs that actually mimic the hormones that tell our brains we’re full.
Some experts believe these medications might finally bend the curve of the national obesity rate. Others worry about the long-term side effects and the fact that we’re medicalizing a problem that started with our food system. It’s a messy, complicated, and very expensive debate.
What Can We Actually Do?
Looking at these statistics can feel pretty hopeless. If three-quarters of the country is struggling, what chance does one person have?
💡 You might also like: Cleveland clinic abu dhabi photos: Why This Hospital Looks More Like a Museum
It’s about small, sustainable shifts rather than radical overhauls that fail by February.
Prioritize Whole Foods Over "Health" Foods
Don't buy the "low fat" cookies. Buy the apple. The less a food has been messed with in a factory, the better your body knows how to process it. Ultra-processed foods are the primary driver of caloric overconsumption because they don't trigger satiety the way fiber and protein do.
Focus on "NEAT"
Non-Exercise Activity Thermogenesis. It’s a mouthful, but it basically means moving when you aren't "working out." Pacing while on the phone, taking the stairs, or standing up every hour. These little movements add up to more burned calories over a week than a single intense gym session.
Sleep is a Weight Loss Tool
Lack of sleep spikes ghrelin (the hunger hormone) and tanks leptin (the fullness hormone). If you’re tired, you’re going to eat more. Period. Getting seven to eight hours of sleep is arguably as important as what you put on your plate.
Advocate for Systemic Change
On a broader level, we need better urban planning and food policies. Making fresh produce more affordable and creating walkable neighborhoods shouldn't be a luxury. It’s a public health necessity.
The percentage of americans who are overweight or obese is a reflection of a society that has prioritized convenience and profit over metabolic health. Changing that won't happen overnight, but understanding the scale of the problem is the first step toward fixing it.
Practical Next Steps
- Audit your pantry: Identify three "ultra-processed" staples you buy every week and replace them with single-ingredient alternatives (e.g., swapping sugary cereal for plain oats with fruit).
- Track your movement, not just your calories: Use a basic pedometer or phone app to see your baseline "NEAT" levels. Aim to increase your daily step count by just 1,000 steps this week.
- Schedule a metabolic panel: If you haven't had blood work recently, ask your doctor for an A1c and lipid profile. Knowing your internal numbers is more important than the number on the scale.
- Prioritize protein: Aim for 25–30 grams of protein at breakfast to stabilize blood sugar and prevent the mid-afternoon "snack attack" that often leads to overeating.