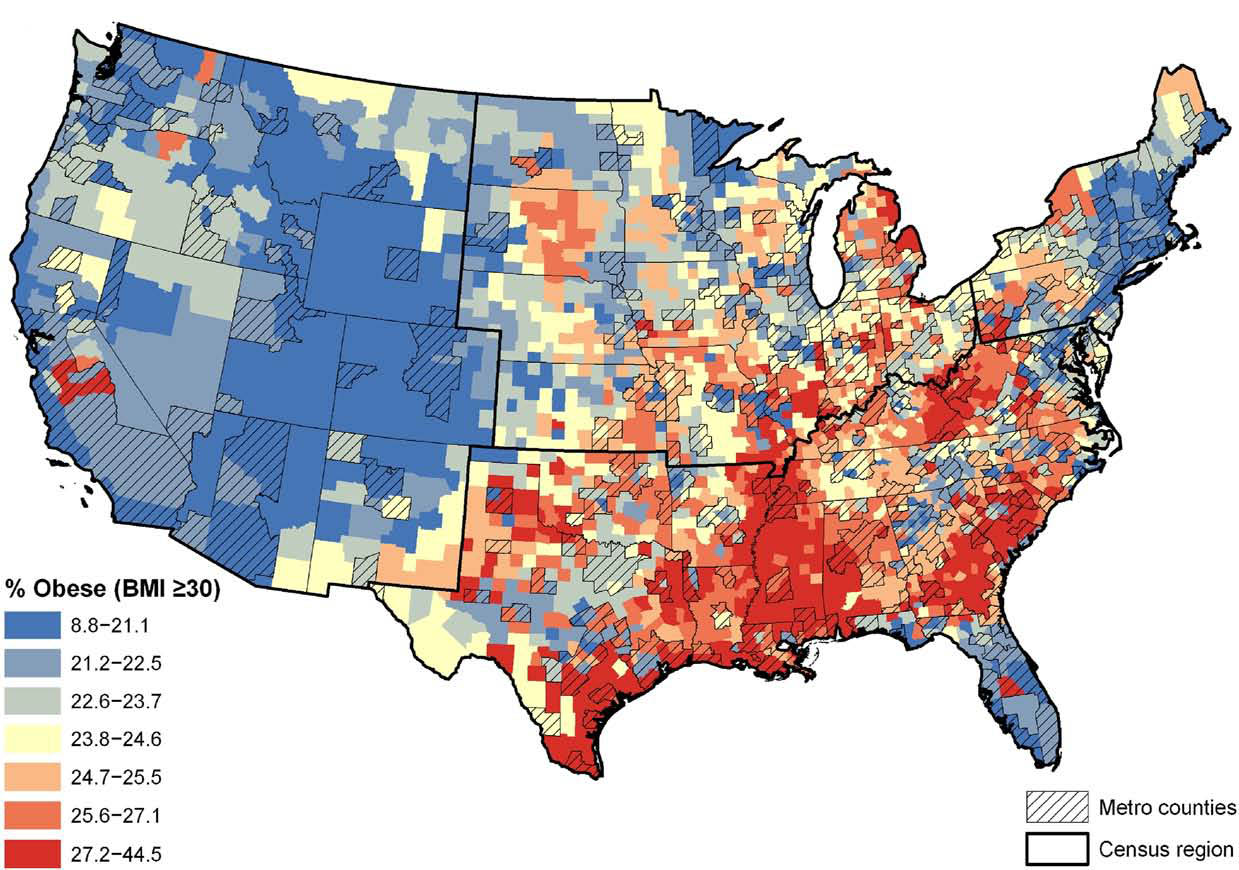
Look at the latest data and it’s pretty jarring. If you pull up the most recent obesity map of the us from the CDC, you aren't just looking at a colorful graphic; you’re looking at a socioeconomic blueprint of the country. It’s a sea of deep reds and dark oranges.
We’re past the point of "eating a few more salads."
According to the CDC’s 2023-2024 Behavioral Risk Factor Surveillance System (BRFSS) data, over 20 states now have an adult obesity prevalence at or above 35%. Think about that. In more than a third of the country, more than one in three adults is living with obesity. It wasn’t like this twenty years ago. Back in 2000, no state had a prevalence over 25%. Now? We’re seeing states like Louisiana, Mississippi, West Virginia, and Oklahoma consistently hitting the highest tiers.
It’s a crisis. But it’s a lopsided one.
What the Obesity Map of the US Actually Tells Us
If you squint at the map, you’ll notice patterns that have nothing to do with willpower. The "Stroke Belt" across the Southeast almost perfectly overlays with the highest rates on the obesity map. This isn't a coincidence. It's a result of systemic factors, historical poverty, and what experts call "food deserts."
Dr. Fatima Cody Stanford, an obesity medicine scientist at Massachusetts General Hospital, has been vocal about how we misinterpret this data. She argues that we often treat obesity as a moral failing rather than a complex brain disease influenced by genetics and environment. When you look at the map, you’re seeing where the environment is the most "obesogenic."
Check out the West Coast and the Northeast. Colorado usually sits at the bottom of the list. Why? It's not just the mountains. It's the infrastructure. It’s the fact that cities like Boulder are designed for walking, while cities in the Deep South are often designed exclusively for cars. If you can't walk to a grocery store that sells fresh produce, you’re stuck with whatever is at the gas station.
Honestly, the obesity map of the us is a map of inequality.
The Race and Ethnicity Gap
The data gets even more granular and, frankly, more upsetting when you break it down by demographics. The CDC reports that non-Hispanic Black adults have the highest age-adjusted prevalence of obesity at nearly 50%. Hispanic adults follow at around 45%. Compare that to non-Hispanic White adults at roughly 41% and Asian adults at 16%.
👉 See also: What Really Happened When a Mom Gives Son Viagra: The Real Story and Medical Risks
Why the massive delta?
It’s not biology in a vacuum. It’s "redlining" legacies. It’s the stress of living in under-resourced neighborhoods. It’s the targeted marketing of ultra-processed foods to specific communities. When we look at the map, we have to acknowledge that health outcomes are baked into the soil of these regions long before an individual ever picks up a fork.
Why the Map Shifted So Fast
We didn't just wake up one day and decide to stop exercising.
The shift in the obesity map of the us over the last three decades tracks perfectly with the rise of ultra-processed foods. These are "industrial formulations" typically containing five or more ingredients—things like high-fructose corn syrup, hydrogenated oils, and flavor enhancers. They are engineered to be hyper-palatable. They bypass our "I'm full" signals.
Kevin Hall, a senior investigator at the NIH, conducted a landmark study showing that people eat about 500 more calories a day when given ultra-processed food compared to unprocessed food, even when the nutrients are matched.
The Economics of the Map
Calories are cheap. Nutrition is expensive.
In West Virginia, a state that often leads the obesity map, the poverty rate is significantly higher than the national average. When you’re trying to feed a family of four on a tight budget, a $2 bag of chips provides more caloric density than a $6 head of cauliflower. The map reflects this economic reality.
We also have to talk about the "built environment."
In states like Texas or Georgia, suburban sprawl is the default. You spend two hours a day in a car. That’s two hours of sedentary behavior baked into your existence. Contrast that with New York City, where even the least active person probably hits 5,000 steps just by commuting. This is why the obesity map of the us shows such stark regional divides. It's about how our towns are built.
✨ Don't miss: Understanding BD Veritor Covid Test Results: What the Lines Actually Mean
Misconceptions We Need to Kill
There’s this idea that people in "red" states just don't care about their health.
That’s nonsense.
The reality is that people in high-prevalence states often have less access to healthcare providers who specialize in obesity. Most primary care doctors receive less than a dozen hours of nutrition training in medical school. They tell patients to "eat less and move more," which we now know is about as effective as telling a person with clinical depression to "just cheer up."
It’s about biology.
When you lose weight, your body fights back. Your levels of ghrelin (the hunger hormone) spike, and leptin (the fullness hormone) plummets. Your metabolism slows down to protect its "set point." This is why regional interventions—like better school lunches and walkable parks—are more effective than individual shaming.
The GLP-1 Factor: Will the Map Change?
We are currently in the middle of a massive shift in how we treat obesity, thanks to medications like semaglutide (Wegovy) and tirzepatide (Zepbound). These drugs mimic hormones that tell the brain you’re full.
Will these drugs change the obesity map of the us?
Maybe. But only if people can afford them.
Right now, there’s a massive "access gap." If you live in a wealthy zip code in California, your insurance might cover these $1,000-a-month medications, or you can pay out of pocket. If you’re in a rural part of Arkansas, you might not have a specialist within 50 miles who can prescribe them, let alone the insurance coverage to pay for them. We risk creating a new kind of "health divide" where the map stays red in poor areas and turns green in wealthy ones.
The Surprising Truth About "Health" vs. "Weight"
It’s possible to be metabolically healthy at a higher weight, and it’s possible to be "skinny fat" with high visceral fat. However, the obesity map of the us is a reliable proxy for other health crises.
🔗 Read more: Thinking of a bleaching kit for anus? What you actually need to know before buying
Where obesity rates are high, Type 2 diabetes rates are high.
Where obesity rates are high, hypertension is rampant.
These aren't just statistics; they are drivers of healthcare costs. We spend billions treating the complications of obesity rather than the root causes. We’re treating the smoke instead of the fire.
Moving Beyond the Map: Real Actionable Steps
Looking at the map can feel hopeless. It’s easy to feel like a tiny speck against a massive national trend. But understanding the map allows you to navigate your own environment more effectively.
First, acknowledge your environment. If you live in a "car-dependent" area, you have to be intentional about "NEAT" (Non-Exercise Activity Thermogenesis). This is the energy we burn doing everything that isn't sleeping, eating, or sports-like exercise. Take the stairs. Park at the back of the lot. It sounds cliché, but it’s a direct counter-attack against an environment designed to keep you still.
Second, audit your "food environment."
The obesity map of the us is fueled by ultra-processed foods. You don't have to be perfect, but try the "80/20" rule. Aim for 80% whole foods—things that don't have a label or only have one ingredient. If it comes in a crinkly plastic bag, it’s likely designed to make you overeat.
Third, push for local policy.
This is the big one. Change happens at the local level. Support initiatives for bike lanes, community gardens, and better school food programs. The map only changes when the infrastructure changes.
Finally, talk to a specialist.
If you’re struggling, stop relying on "influencer" advice. Seek out an American Board of Obesity Medicine (ABOM) certified physician. They understand the science behind the map and can provide treatments—from behavioral therapy to medication—that actually work.
The obesity map of the us is a call to action. It shows us where we are failing as a society, but it also gives us the data we need to start fixing it. It's time to stop blaming the individual and start fixing the map.
Summary of Actionable Insights:
- Identify your local risks: Recognize if you live in a "food desert" or a car-dependent city and prioritize daily movement.
- Prioritize fiber over calories: High-fiber, unprocessed foods naturally regulate hunger hormones better than calorie-counting alone.
- Consult an ABOM specialist: Move past "dieting" and look into medical management if lifestyle changes aren't enough.
- Advocate for infrastructure: Support local walkability and school nutrition standards to change the environment from the ground up.