It’s a heavy topic. Literally. When you look at the map of obesity in america, you aren't just looking at a colorful graphic of the United States; you’re looking at a visual representation of a massive, systemic health crisis that has been decades in the making. It’s a mess of economics, biology, and geography.
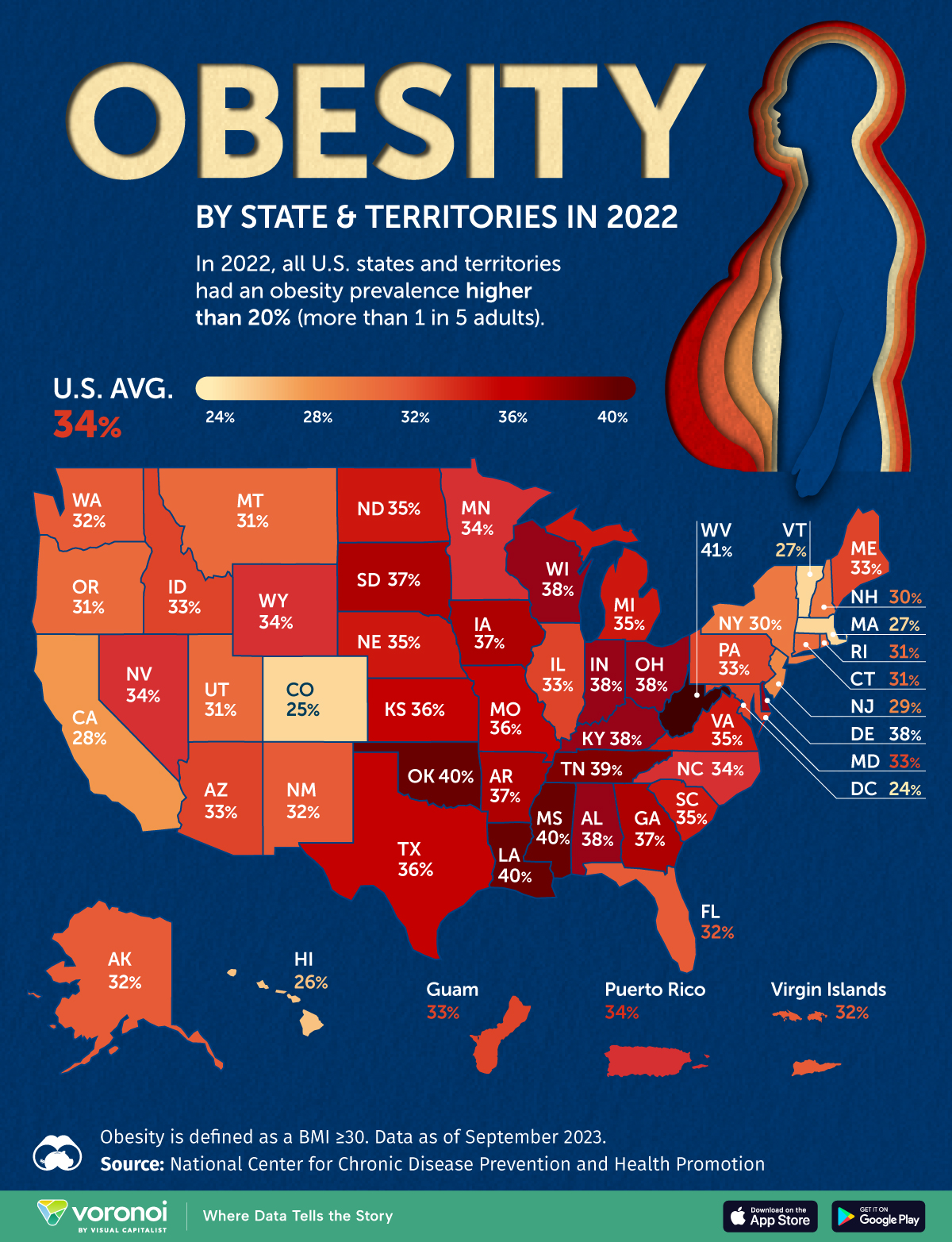
Honestly, it's pretty jarring. If you compare a map from the 1990s to one from the CDC's latest 2024 or 2025 data sets, the shift is wild. We went from a country where no state had an obesity prevalence over 15% in the early 80s to a nation where nearly every single state is well over 30%. In some places, like West Virginia and Louisiana, the numbers are pushing past 40% for adults. That’s nearly one in every two people.
What the Map of Obesity in America is Actually Telling Us
The map isn't just about "willpower" or people liking cheeseburgers too much. That’s a lazy way to look at it. If you overlay a map of poverty or a map of "food deserts" on top of the obesity data, the outlines match up almost perfectly.
Take the "Stroke Belt" in the Southeastern U.S. states like Mississippi, Alabama, and Arkansas consistently show up in the darkest shades of red or purple on these maps. Why? It’s not just the soul food. It’s the lack of walkable infrastructure, the prevalence of low-wage jobs that don't allow for meal prep time, and the "dollar store" effect where fresh produce is a twenty-minute drive away but a bag of chips is on every corner.
The Regional Divide is Real
The Midwest and the South are consistently the heaviest regions. You see states like Oklahoma and Kentucky often topping the lists. Meanwhile, Colorado and Hawaii usually stay on the lighter end of the spectrum, but even their "good" numbers would have been considered a national emergency thirty years ago.
🔗 Read more: Why Having Sex in Bed Naked Might Be the Best Health Hack You Aren't Using
- The South: High rates of adult obesity, often linked to systemic poverty and cultural dietary traditions that haven't adapted to more sedentary lifestyles.
- The West: Generally lower rates, particularly in mountain states like Utah or Colorado where outdoor recreation is baked into the culture and the climate allows for year-round activity.
- The Northeast: A mixed bag. Cities like New York have high walkability, which helps, but rural parts of Pennsylvania or upstate New York mirror the struggles of the Midwest.
Why the Data Keeps Shifting
The CDC uses the Behavioral Risk Factor Surveillance System (BRFSS) to build these maps. It’s based on self-reported height and weight to calculate BMI. Now, we know BMI (Body Mass Index) isn't perfect. It doesn't distinguish between muscle and fat. A bodybuilder might technically be "obese" according to the chart. But on a population level? It’s a very reliable indicator of where the healthcare system is going to feel the most pressure.
We’re seeing a massive uptick in "severe obesity" too. This isn't just being twenty pounds overweight; this is having a BMI of 40 or higher. This specific demographic has grown significantly, and it’s where we see the highest correlations with Type 2 diabetes, hypertension, and certain types of cancer.
It’s a Socioeconomic Map
If you’re wealthy, you can buy health. You can pay for a trainer, organic kale, and the time to cook it. If you’re working two jobs in a rural county in Ohio, your dinner is whatever is fast and cheap. The map of obesity in america is, in many ways, a map of the American class divide.
Dr. Fatima Cody Stanford, an obesity medicine scientist at Massachusetts General Hospital, has often pointed out that the brain regulates weight more than we give it credit for. It’s not just about calories in versus calories out. It’s about stress, sleep deprivation, and the quality of the food. When you’re stressed about rent, your cortisol levels spike, and your body wants to hold onto fat. The map reflects this biological reality of living in high-stress, low-resource environments.
💡 You might also like: Why PMS Food Cravings Are So Intense and What You Can Actually Do About Them
The Racial and Ethnic Disparities
The data gets even more complex when you break it down by demographics. Non-Hispanic Black adults and Hispanic adults have statistically higher rates of obesity compared to White or Asian adults. This isn't a genetic inevitability; it’s a result of decades of redlining and unequal access to healthcare and grocery stores.
In many majority-Black neighborhoods, the ratio of fast-food joints to grocery stores is staggering. When the only "grocery store" within three miles is a gas station, the map is going to look a certain way. You can't out-run a bad environment.
What about the kids?
The map for childhood obesity is arguably more concerning. We’re seeing "adult-onset" diabetes appearing in teenagers at rates that would have been unthinkable in the 1970s. These habits and physiological changes are getting locked in early, making the adult map of the future look even more daunting unless there’s a radical shift in how we handle school lunches and physical education.
Is Technology Helping or Hurting?
You’d think with all the fitness trackers and calorie-counting apps, we’d be getting thinner. Nope. The map keeps getting darker. Screen time has replaced "outside time" for almost every demographic. We’ve built a world where you don't have to move to survive. You can order groceries, work, and socialize without ever leaving your couch.
📖 Related: 100 percent power of will: Why Most People Fail to Find It
But there is a silver lining. New medications like GLP-1 agonists (think Ozempic or Wegovy) are starting to have a measurable impact on the data. For the first time in years, some clinicians are hopeful that the 2026 and 2027 maps might show a plateau or even a slight dip in certain regions. But these drugs are expensive. If only the wealthy can afford them, the map will just show an even wider gap between the "haves" and "have-nots" of metabolic health.
Addressing the Map: Actionable Steps
We can’t just look at the map and sigh. It requires actual changes at both the personal and policy levels.
- Advocate for Walkability: If your town doesn't have sidewalks or bike lanes, talk to your local government. Physical activity shouldn't require a gym membership; it should be part of getting to the store or the library.
- Support Local Food Systems: Farmer’s markets that accept SNAP (food stamps) are one of the most effective ways to change the "food desert" narrative.
- Prioritize Sleep and Stress Management: It sounds "woo-woo," but chronic stress is a primary driver of metabolic dysfunction. If you're constantly in "fight or flight" mode, your body will stay in "store fat" mode.
- Re-evaluate "Ultra-Processed" Foods: It’s not just about calories. The emulsifiers and stabilizers in highly processed foods mess with your gut microbiome, which controls how you process energy. Try to eat things that don't have a shelf life of three years.
- Focus on "Health at Every Size" Principles: Shaming people doesn't make them lose weight. It actually does the opposite by increasing cortisol. Focus on movement that feels good and nourishment that provides energy rather than just hitting a number on a scale.
The map of obesity in america is a wake-up call that has been ringing for a long time. It’s a signal that our environment is mismatched with our biology. Solving it isn't about a new fad diet; it's about restructuring our communities to make the healthy choice the easy choice.
If you’re looking at your own state on that map and feeling discouraged, remember that these are macro-trends. They don't dictate your individual health journey, but they do highlight the uphill battle many of us are fighting against an environment designed to keep us sedentary and overfed. Change starts with recognizing that the map is a systemic issue, not just a personal failing.