You’ve seen it. Everyone has. You look down at your wrist and see those thin, branching pathways of blue or greenish-teal snaking under your skin. Because of those visual cues, a massive chunk of the population grew up believing a specific "fact" taught on playgrounds and even in some questionable classrooms: that blood is blue until it hits the oxygen in the air.
It sounds scientific enough. It explains why veins look the way they do. But honestly? It’s completely wrong.
The color of human blood inside the body is always red. Always. Whether it’s surging through your heart or trickling through a tiny capillary in your pinky toe, it never turns blue. Not for a second. Even when it’s "deoxygenated" and heading back to your lungs for a refill, it stays firmly in the red family.
But why do we see blue? Why does a bruise change colors? And if it's always red, why does the shade change so drastically between an artery and a vein? To understand the real story, we have to look at the chemistry of your insides and the weird way light plays tricks on your eyes.
The Chemistry of Red: Hemoglobin and the Iron Connection
Blood is a complex soup of plasma, platelets, and white blood cells, but the "redness" comes from one specific player: hemoglobin. This protein is the workhorse of your circulatory system. Its only job is to grab oxygen and carry it where it needs to go.
Inside every hemoglobin molecule are four iron atoms. When these iron atoms bind with oxygen, they undergo a chemical change that alters how they absorb and reflect light. This is a process called oxidation. Think about rust. When iron is exposed to oxygen and moisture, it turns a bright, reddish-orange. A similar principle is at play in your veins, though much faster and more sophisticated.
When your blood is saturated with oxygen—fresh from the lungs—it is a bright, vivid scarlet. This is the blood found in your arteries. It’s high-pressure, high-energy, and ready to fuel your muscles.
However, once that blood delivers its oxygen cargo to your tissues, the hemoglobin changes shape slightly. It loses that "bright" reflectiveness. The color of human blood inside the body then shifts to a deep, dark, dusky maroon. If you’ve ever donated blood and noticed the bag looks almost like black cherry juice, that’s why. It’s deoxygenated blood, but it is still undeniably red.
🔗 Read more: Ingestion of hydrogen peroxide: Why a common household hack is actually dangerous
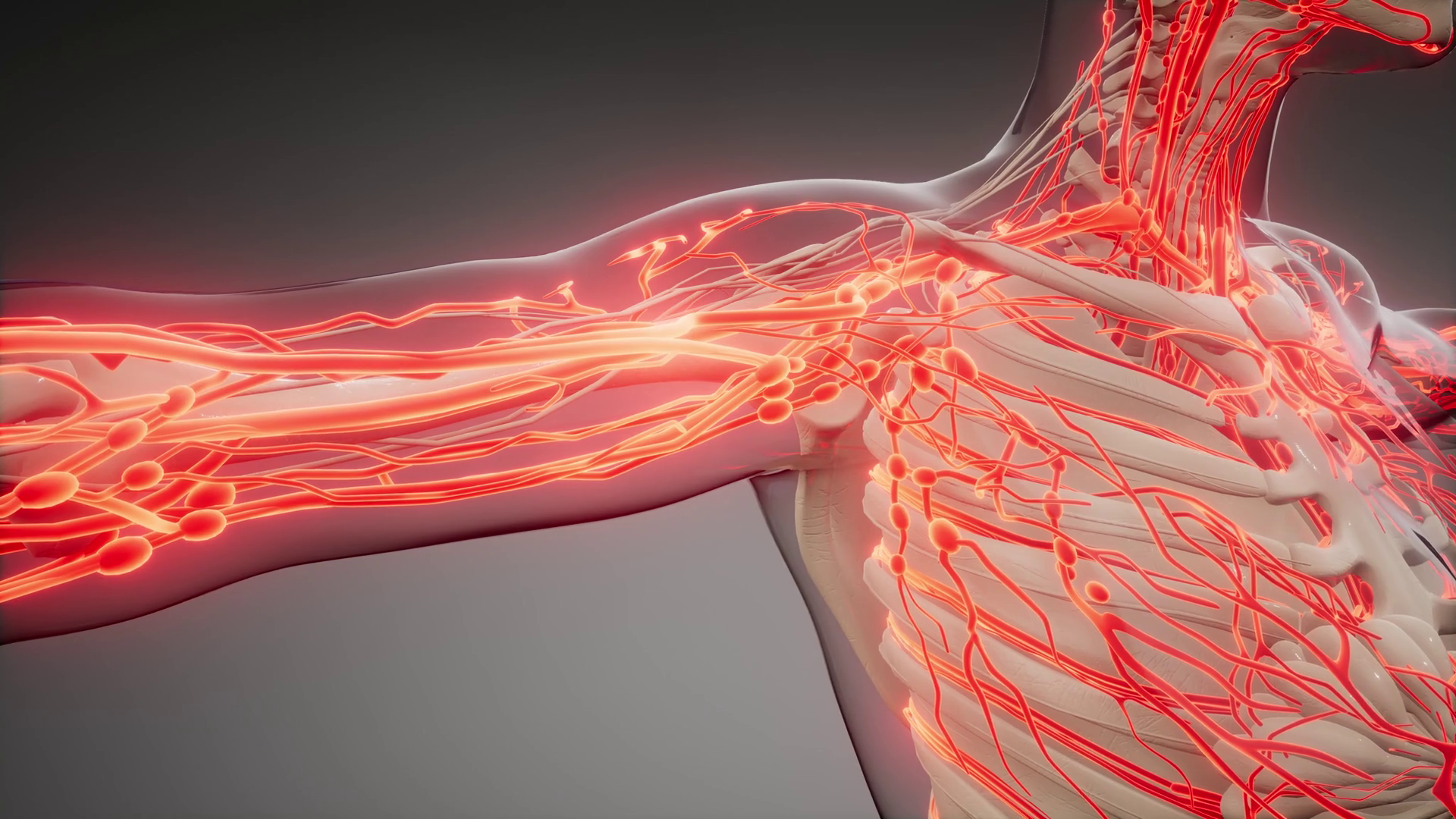
The Light Trick: Why Your Veins Look Blue
If the blood is dark red, why does your wrist look like a map of the Caribbean Sea? This is where physics messes with your head. It’s an optical illusion caused by how different wavelengths of light penetrate your skin.
Light isn't just one thing; it's a spectrum. Red light has long wavelengths. Blue light has short wavelengths.
When white light (like sunlight or a lamp) hits your arm, the red wavelengths are actually pretty good at penetrating deep into your tissue. They get absorbed by the dark, deoxygenated blood in your veins. The blue wavelengths, however, don't make it very far. They bounce off the surface of the skin and the vessel walls, reflecting back into your eyes.
Basically, your skin acts as a filter. You aren't seeing the color of the fluid; you're seeing the light that didn't get absorbed. Scientists like Dr. Alwin Kienle have published extensive papers on this phenomenon, using "transport theory" to model exactly how photons navigate through human tissue. The conclusion is always the same: the "blue" is a ghost.
The Horseshoe Crab Exception
To be fair to the "blue blood" theorists, blue blood does exist in nature. Just not in humans.
If you were a horseshoe crab, your blood would be a startling, bright baby blue. This is because they don't use hemoglobin. Instead, they use a protein called hemocyanin, which relies on copper rather than iron. When copper gets oxidized, it turns blue-green (think of the Statue of Liberty).
Some octopuses and spiders share this trait. But humans are strictly iron-based. We are "red-blooded" in every sense of the phrase. Even in medical emergencies where someone is suffering from severe cyanosis—a condition where the skin or lips turn blue due to lack of oxygen—the blood inside is still dark red. The "blue" tint on the skin is just the visual manifestation of that dark, oxygen-starved blood being filtered through the surface layers of the body.
💡 You might also like: Why the EMS 20/20 Podcast is the Best Training You’re Not Getting in School
The Myth of the "Blue to Red" Transition
We’ve all heard the story: "Blood is blue inside, but it turns red the moment it hits the air."
This is a classic case of correlation not being causation. When you cut yourself, the blood is bright red because it's instantly hitting a high-oxygen environment. But if you were to look at blood inside a vacuum-sealed tube, or through the glass of a syringe during a blood draw, it would still be red.
The medical community has spent decades trying to debunk this, yet it persists. Maybe it’s because it feels like it should be true. Our diagrams in textbooks almost always show arteries in red and veins in blue. This is a helpful shorthand for doctors and students to distinguish which way the blood is flowing, but it was never meant to be a literal color guide.
Imagine how confusing a medical chart would be if everything was just slightly different shades of maroon. The "blue vein" convention is a map, not a photograph.
Does Blood Ever Change Color?
While it stays red, the shade tells a story. Doctors use this as a diagnostic tool.
If a surgeon nicks a vessel and the blood is "pulsatile" and bright red, they know they’ve hit an artery. If it’s a slow, dark ooze, it’s a vein. But there are rare conditions that can actually change blood color.
- Sulfhemoglobinemia: This is a super rare condition where a sulfur atom integrates into the hemoglobin molecule. This can happen due to certain medications like sulfonamides. The result? Blood that actually looks greenish or blackish.
- Methemoglobinemia: This turns the blood a brownish, chocolatey color. It happens when the iron in the blood is in a specific state ($Fe^{3+}$ instead of $Fe^{2+}$) that can't carry oxygen effectively.
These are medical anomalies, though. For 99.9% of the population, the color of human blood inside the body is a spectrum of red.
📖 Related: High Protein in a Blood Test: What Most People Get Wrong
Why This Matters for Your Health
Knowing the reality of blood color helps you understand how your body uses oxygen. Every time you breathe, you are performing a massive chemical color-shift inside your chest.
When you track your "oxygen saturation" (SpO2) with a pulse oximeter—that little clip they put on your finger at the doctor—the device is actually using the color of your blood to give you a score. It shines a red light and an infrared light through your finger. By measuring how much of each light is absorbed, the sensor calculates how "red" your blood is.
If your blood is absorbing more infrared light, it means it's highly oxygenated (bright red). If it’s absorbing more red light, it’s deoxygenated (dark maroon). The device is literally "reading" the shade of red to see if you’re breathing well enough.
Take Action: What to Watch For
While your blood is always red, the appearance of your veins and the color of your skin can tell you a lot about your circulation. Don't worry about the "blue" color of the veins themselves, but do pay attention to changes in the surrounding area.
- Check for "Staining": If the skin around your ankles starts to turn a permanent reddish-brown (hemosiderin staining), it can mean blood is leaking out of tiny vessels because of poor circulation.
- Monitor Bruises: A bruise is just blood trapped under the skin. It starts red/purple (fresh blood), turns blue/black (oxygen loss), and then green/yellow as the body breaks down the iron (biliverdin and bilirubin). This "rainbow" is a sign your body is cleaning up the mess.
- The Press Test: Press your fingernail until it turns white, then let go. It should turn back to a healthy pink (red blood returning) in under two seconds. This is called "capillary refill time."
Next time someone tells you that your blood is blue until you take a breath, you can confidently tell them they’re seeing a physics trick. It's a dark, deep red, working hard to keep you moving. If you’re curious about your own circulation, the best next step is to check your capillary refill or track how quickly a bruise heals—it's the easiest way to see your blood's chemistry in action without needing a needle.
Expert Insight Summary:
The color of human blood inside the body is determined by the oxidation state of heme iron. Arterial blood is bright scarlet ($HbO_2$), while venous blood is dark maroon ($Hb$). The blue appearance of veins is a result of selective light scattering (the Tyndall effect) and the way human skin reflects short-wavelength light. Unless you are a horseshoe crab or suffering from a rare sulfur-based blood disorder, your blood never leaves the red spectrum.