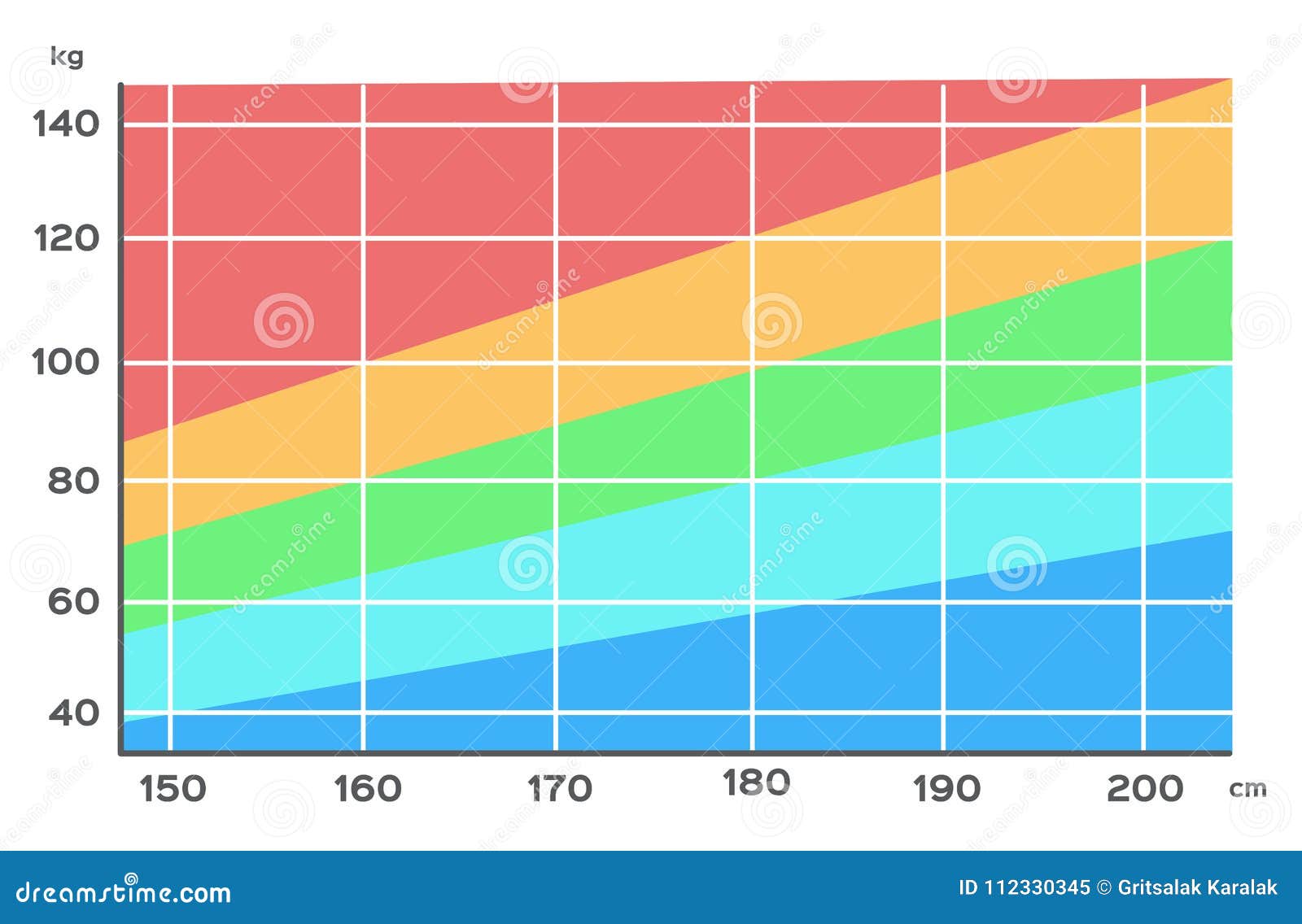
You’ve probably seen it hanging on a dusty wall in a doctor’s office. It’s that grid of colors—usually ranging from a pale yellow to a deep, alarming red—that tells you exactly where you stand based on two simple numbers: your height and your weight. Honestly, the body mass index chart is a bit of a relic. It feels like something from a different era because, well, it is. Invented nearly 200 years ago by a Belgian mathematician named Lambert Adolphe Jacques Quetelet, it wasn't even meant for doctors. Quetelet was a statistician trying to define the "average man" for social research, not a physician trying to diagnose your health.
Fast forward to today and we are still using this same math. It’s wild.
The formula is straightforward. You take your weight in kilograms and divide it by your height in meters squared ($BMI = kg/m^2$). If you’re using pounds and inches, the math gets a little clunkier, but the result is the same. You get a number. That number drops you into a bucket: Underweight, Normal, Overweight, or Obese. But here is the thing. That number doesn't know if you’ve spent the last six months hitting the squat rack or if you’ve been sitting on the couch eating chips. It treats muscle and fat exactly the same.
Understanding the Body Mass Index Chart and Its Limits
When you look at a body mass index chart, the categories seem set in stone. Under 18.5? Underweight. 18.5 to 24.9? Healthy weight. 25 to 29.9? Overweight. 30 or higher? Obese. It’s clean. It’s easy for insurance companies to track. But it is fundamentally flawed for individuals.
🔗 Read more: Finding Your Way Around the Kaiser Permanente Mosswood Building Without Getting Lost
Take a professional rugby player or a bodybuilder. These athletes are often packed with lean muscle. Muscle is much denser than fat. Because the BMI formula only cares about total mass, these elite athletes often land squarely in the "obese" category on a standard body mass index chart. Does that mean they are at risk for Type 2 diabetes or heart disease? Likely not. Conversely, you have people who fall into the "normal" range but have very little muscle and high levels of visceral fat—the dangerous kind that wraps around your organs. In medical circles, this is often called "skinny fat" or metabolically obese normal weight (MONW). The chart says they’re fine. Their bloodwork might say something else entirely.
We have to acknowledge the racial and gender biases baked into these old charts too. Quetelet’s original data was based almost exclusively on European men. Research, including studies published in The Lancet Diabetes & Endocrinology, suggests that the "healthy" BMI threshold might actually be lower for people of Asian descent due to a higher risk of metabolic issues at lower weights. Similarly, women naturally carry more body fat than men, yet the chart often applies the same broad strokes to everyone. It’s a blunt instrument used for a delicate job.
Why We Still Use It Anyway
If it's so flawed, why haven't we tossed it?
Efficiency.
Doctors need a quick screening tool. It’s a starting point. If a patient’s BMI is 35, it’s a red flag that prompts further investigation, like checking blood pressure, cholesterol, and blood sugar levels. It’s a "first look" tool, not a final diagnosis. According to the CDC, BMI is a reasonable indicator of body fatness for most people, even if it misses the mark for the extremes of the population. It’s also incredibly cheap. Measuring a waist circumference or doing a DEXA scan takes time and money. Stepping on a scale takes five seconds.
But don't let the chart's simplicity fool you into thinking it's the only metric that matters. Your "health" is a massive puzzle. BMI is just one tiny, slightly warped piece of that puzzle.
Better Ways to Measure Progress
If you’re trying to get a real sense of your health, stop obsessing over the grid. There are better metrics that actually tell you what’s happening inside your body.
- Waist-to-Hip Ratio (WHR): This is often a better predictor of cardiovascular risk than BMI. You just measure the smallest part of your waist and the widest part of your hips. Divide the waist by the hip. For men, a ratio above 0.90 suggests increased risk. For women, it's above 0.85.
- Body Fat Percentage: This is the big one. Whether through skinfold calipers, bioelectrical impedance scales (the ones you stand on at home), or the "gold standard" DEXA scan, knowing how much of you is fat versus bone and muscle is far more useful than a total weight number.
- Visceral Fat Levels: Some high-end scales now estimate visceral fat. This is the "hidden" fat deep in the belly. High levels here are a massive warning sign, regardless of what the body mass index chart says about your total weight.
- Functional Fitness: Can you walk up three flights of stairs without gasping for air? Can you carry your groceries? How is your grip strength? These "real world" metrics often correlate more closely with longevity than a height-to-weight ratio.
The Psychology of the Number
We need to talk about the mental toll these charts take. I've seen people get completely derailed because a chart told them they were "overweight" when they felt the best they’d ever felt. They were eating whole foods, sleeping well, and lifting weights. But the scale didn't move "down" because they were gaining muscle.
The body mass index chart can be a trigger. It simplifies the complex human experience into a single digit. If that digit doesn't align with your goals, it feels like failure. But you have to remember: the chart doesn't see your habits. It doesn't see your energy levels. It doesn't see your blood pressure improving.
Real-World Evidence: The Obesity Paradox
There is a fascinating, albeit controversial, concept in medicine called the "obesity paradox." Some studies have shown that in certain populations—like elderly patients or those with chronic heart failure—having a slightly higher BMI (falling into the "overweight" category) might actually be protective. It provides a metabolic reserve. This doesn't mean obesity is "healthy," but it underscores that the relationship between weight and mortality isn't a simple straight line. It's a curve.
🔗 Read more: The Real Vibe at Mighty Yoga Ithaca NY and Why It Actually Works
Actionable Steps for a Healthier View
Instead of staring at a body mass index chart and feeling discouraged, try a more nuanced approach to your health.
- Get a full panel. Go to your doctor and ask for more than just a weigh-in. Get your A1C (blood sugar), lipid panel (cholesterol), and blood pressure checked. These numbers don't lie.
- Measure your waist. Keep an eye on your waist circumference. If it’s creeping up, that’s a signal to adjust your nutrition or activity, even if your total weight stays the same.
- Focus on performance. Set goals that have nothing to do with the scale. Try to run a mile faster, do five more pushups, or hold a plank for an extra thirty seconds.
- Audit your body composition. If you can afford it, get a DEXA scan once a year. It’s the most accurate way to see where you are actually storing fat and how much muscle you’re carrying.
- Ignore the "categories." Treat your BMI as a data point, not a label. If you are a 27 (overweight) but your metabolic markers are perfect and you're active, you're likely doing just fine.
The body mass index chart is a tool from the 1800s. Use it as a reference if you must, but don't let it be the boss of you. Your health is way too complex for a two-century-old math equation to summarize. Focus on how you feel, how you move, and what your bloodwork says. Those are the metrics that actually define your future.
Next Steps for You: Grab a flexible measuring tape and check your waist-to-hip ratio today. It takes two minutes and provides a much clearer picture of your metabolic health than a standard weight scale. If your ratio is high, prioritize increasing your daily step count and reducing processed sugar intake to target visceral fat reduction.