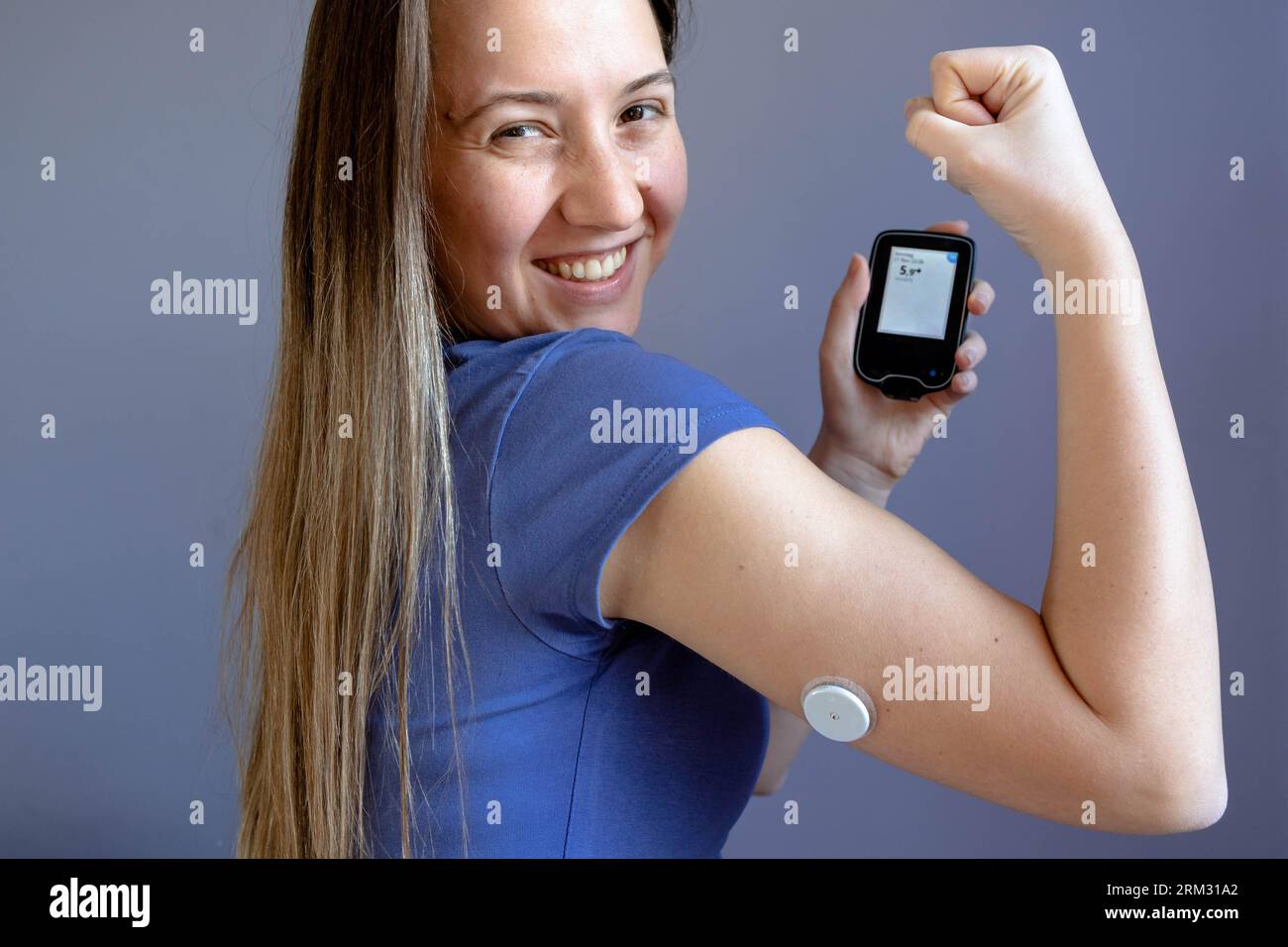
You’re at the grocery store. You see someone with a small, white plastic disc stuck to the back of their tricep. Ten years ago, you might have wondered if it was a nicotine patch or some weird futuristic medical experiment. Today? It’s everywhere. That blood sugar arm monitor—formally known as a Continuous Glucose Monitor or CGM—has moved from the niche world of Type 1 diabetes management into the mainstream fitness and biohacking scene.
It’s a massive shift.
Honestly, the tech is cool. Instead of stabbing your finger five times a day and squeezing a drop of blood onto a strip that looks like a tiny piece of cardboard, you just wave your phone over your arm. Or, better yet, you just look at your smartwatch. The data is just there. But there is a lot of noise out there about what these things actually do, who needs them, and why your doctor might be annoyed that you’re wearing one if you aren't diabetic.
The Reality of the Sensor Under Your Skin
Most people think the blood sugar arm monitor is measuring their actual blood. It isn’t. Not exactly. When you apply a sensor like the Abbott Freestyle Libre or the Dexcom G7, a tiny, flexible filament—thinner than a hair—is inserted just under the skin.
It sits in the interstitial fluid.
That’s the fluid surrounding your cells. It’s not the same as the "capillary blood" you get from a finger stick. Because of this, there is a "lag time." If you eat a massive bowl of pasta, your blood sugar spikes in your veins first. The glucose then seeps into the interstitial fluid. This process takes about 5 to 15 minutes. If you feel shaky and think your sugar is crashing, your arm monitor might still show you’re fine because it’s "living in the past" by ten minutes. It’s a nuance that matters.
People get obsessed with the numbers. They see a 110 mg/dL and panic because they wanted a 95. But here’s the kicker: even the best monitors have a margin of error. The industry standard is called MARD (Mean Absolute Relative Difference). Most top-tier monitors have a MARD under 10%. This means if your actual blood sugar is 100, the monitor is legally and medically "accurate" if it reads anywhere between 90 and 110.
Context is everything.
👉 See also: Why the Dead Bug Exercise Ball Routine is the Best Core Workout You Aren't Doing Right
Why the "Arm" Location Won the Popularity Contest
You can technically wear these sensors in other places. Some people put them on their abdomen or the upper curve of their buttocks (mostly for kids). But the back of the upper arm became the gold standard for a few practical reasons.
First, there’s less "compression low" risk. If you sleep on your sensor, the pressure can push the fluid away from the filament, making the device think your sugar is tanking. You wake up to a screaming alarm at 3:00 AM thinking you’re dying, but you were just lying on your arm. The back of the arm tends to be flatter and more protected than the belly, where waistbands and seatbelts constanty rub.
Also, let’s be real. It’s a status symbol now.
Seeing a blood sugar arm monitor on a celebrity or an athlete sends a message: "I care about my metabolic health." It’s the new Oura ring. Whether that’s a good thing for the healthcare system is a different debate entirely, especially when supply chain issues hit and people with life-threatening diabetes can't find their sensors.
What the Data Actually Tells You (And What It Doesn't)
If you’re a non-diabetic using a monitor to "optimize" your life, you’re looking for glucose variability. This is the "spikiness" of your blood sugar.
Imagine a roller coaster. You want the kid-friendly hills, not the 90-degree drops.
When your sugar spikes high after a meal, your pancreas pumps out insulin to bring it back down. If the spike is too high, the insulin response can be too aggressive, leading to a "crash" that leaves you foggy, irritable, and craving a donut. This is the "afternoon slump" most office workers feel.
✨ Don't miss: Why Raw Milk Is Bad: What Enthusiasts Often Ignore About The Science
But here’s where it gets complicated. A spike isn't always bad.
If you go for a sprint, your liver dumps glucose into your bloodstream to fuel your muscles. Your blood sugar arm monitor might show a scary-looking spike. Does that mean exercise is bad? Of course not. It means your body is doing exactly what it was evolved to do. Contextless data is dangerous. I’ve seen people stop eating fruit because their CGM showed a spike after an apple, ignoring the fiber, vitamins, and polyphenols that make fruit objectively healthy.
Real-World Examples of Glucose Triggers
- Stress: You’re in a tense meeting. You haven't eaten in four hours. Suddenly, your glucose jumps 20 points. That’s cortisol telling your liver to prep for a fight.
- Poor Sleep: One night of four-hour sleep can make you look pre-diabetic on a monitor the next morning. Your insulin sensitivity drops through the floor.
- The Order of Food: If you eat a steak and broccoli before the breadbasket, your glucose curve will be much flatter than if you ate the bread first. Protein and fiber slow down gastric emptying.
The Big Players: Dexcom vs. Libre vs. The Newcomers
Right now, the market is basically a duopoly with some hungry startups biting at the heels.
The Abbott FreeStyle Libre 3 is the size of two stacked pennies. It’s tiny. It’s also relatively affordable if your insurance doesn’t cover it (around $75-$150 for a month's supply). It sends data via Bluetooth to your phone every minute.
Then you have the Dexcom G7. It’s the powerhouse. It’s widely considered the most accurate and is often the one integrated with insulin pumps for people with Type 1. It’s a bit more expensive, but the app interface is slicker for most users.
Then there are the "software layers" like Levels, Nutrisense, or Signos. These companies don't make the hardware. They buy the Libre or Dexcom sensors, ship them to you, and provide a much better app that helps you log food and score your metabolic health. They’re basically translators for the raw data. They make the blood sugar arm monitor feel less like a medical device and more like a fitness tracker.
Is It Worth the Itch?
The "ick" factor is real. These things use medical-grade adhesive. If you have sensitive skin, you might end up with a red, itchy square on your arm that lasts for a week after you rip the sensor off.
🔗 Read more: Why Poetry About Bipolar Disorder Hits Different
There’s also the mental health aspect.
"Data obsession" is a real thing. If you find yourself checking your phone 50 times a day and feeling guilty because you ate a piece of birthday cake that caused a spike, the monitor might be doing more harm than good. For a diabetic, this data is a lifesaver. For a healthy 25-year-old, it can sometimes cross the line into orthorexia—an unhealthy obsession with healthy eating.
Actionable Steps for Using a Blood Sugar Arm Monitor
If you’ve decided to slap one of these on, don’t just watch the numbers go up and down. That’s boring and useless. Do some experiments.
1. The "N of 1" Food Test
Eat a plain white bagel on day one. Watch what happens. On day two, eat the same bagel but go for a 15-minute brisk walk immediately after. You will likely see a massive difference in how high your sugar peaks. Movement is a glucose vacuum.
2. Check Your Fasting Baseline
Look at your numbers between 2:00 AM and 5:00 AM. This is your true baseline. If it’s consistently high (over 100 mg/dL), it might be worth talking to a doctor about insulin resistance, even if your A1c (the three-month average) looks "normal."
3. Don't Calibrate Constantly
If your monitor allows calibration (like Dexcom), don't do it while your sugar is moving fast (like right after a meal). Only calibrate when the trend line is flat, or you'll confuse the sensor and end up with wonky readings for the rest of its 10-to-14-day life.
4. Protect the Sensor
If you’re active, buy an "overpatch." It’s basically a big waterproof sticker that goes over the monitor. One doorway bump or a sweaty gym session can rip a $70 sensor right off your arm.
The blood sugar arm monitor is a window into a previously invisible part of our biology. It turns "I feel tired" into "I can see exactly why I’m tired." As the tech gets cheaper and even less invasive—there are rumors of non-invasive laser-based sensors on the horizon—we’re going to see these become as common as heart rate monitors. Just remember that the sensor is a tool, not a boss. Use the data to make better choices, but don't let it ruin your dinner.