You’ve heard it since you were a kid. 120 over 80. It’s the metric we’ve been told is the holy grail of cardiovascular health, the "perfect" score that means your heart is ticking along like a Swiss watch. But honestly, it’s not that simple anymore. Medicine changes. We learn. And what we’ve learned recently is that the best blood pressure number depends heavily on who you are, how old you are, and what other health baggage you’re carrying around.
If you walk into a clinic today and clock in at 118/78, your nurse might give you a thumbs up. But for a 75-year-old with a history of fainting spells, that same number might actually be dangerous. It’s weird, right? We want one single answer, a "pass/fail" grade for our arteries, but the human body doesn’t really work in binary.
The 120/80 Myth and the New Reality
For decades, the "normal" ceiling was 140/90. Then, the goalposts shifted. In 2017, the American Heart Association (AHA) and the American College of Cardiology (ACC) dropped the hammer. They redefined "hypertension" to start at 130/80. Suddenly, millions of people who thought they were fine woke up with a medical condition.
Why the change? It wasn't just to sell more pills. It was the SPRINT trial (Systolic Blood Pressure Intervention Trial). This was a massive study involving over 9,000 adults. Researchers found that aiming for a systolic number (the top one) of less than 120—rather than the old standard of 140—cut the risk of cardiovascular events by 25% and the risk of death by 27%. That’s huge. It’s the difference between a long retirement and a sudden stroke.
But here’s the kicker: the best blood pressure number for a marathon runner in her 30s is vastly different from a grandfather managing type 2 diabetes.
High blood pressure is often called the "silent killer" because it doesn't have a distinct feel. You don't get a headache every time your pressure spikes. You just feel... normal. Until you don't. Your arteries are like garden hoses; if the pressure is too high for too long, they start to stiffen, scar, and eventually, they might just burst or clog up entirely.
💡 You might also like: How to Treat Uneven Skin Tone Without Wasting a Fortune on TikTok Trends
Breaking Down the Numbers
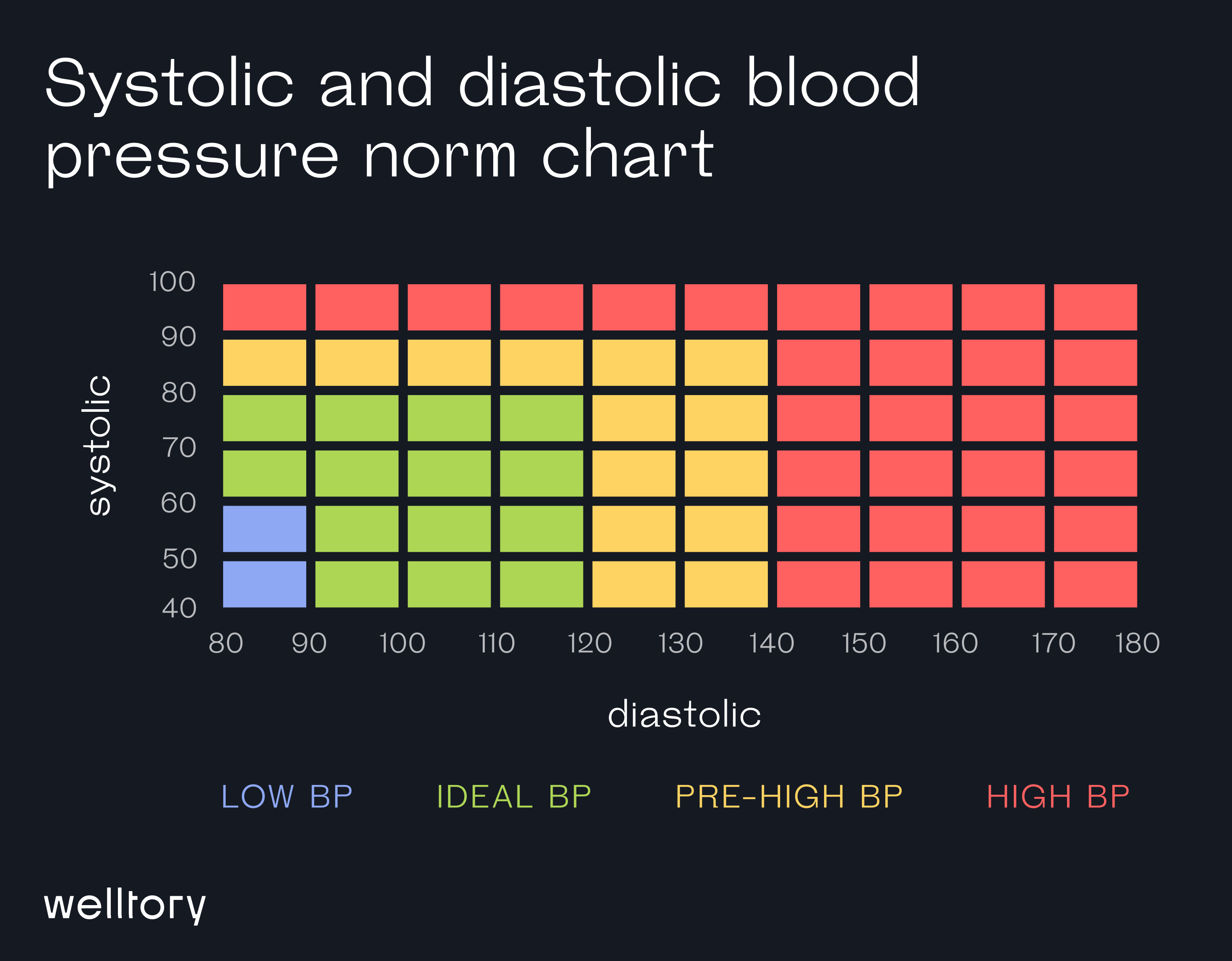
Let's look at the systolic and diastolic divide. The top number, systolic, measures the pressure in your arteries when your heart beats. The bottom number, diastolic, measures the pressure when your heart rests between beats.
Most doctors now care way more about the top number. As we age, our arteries stiffen. This makes the systolic pressure climb while the diastolic might actually stay the same or even drop. If you’re over 50, that top number is your primary predictor of stroke and heart attack.
Why One Size Doesn't Fit All
If you have chronic kidney disease or diabetes, your doctor is going to be aggressive. They want you as close to 120/80 as possible because your "pipes" are already under stress from blood sugar or filtration issues.
However, if you are 85 years old, a blood pressure of 120/80 might make you dizzy when you stand up. This is called orthostatic hypotension. If you get dizzy, you fall. If you fall at 85, you break a hip. In that specific case, the best blood pressure number might actually be 135/85. Doctors call this "clinical judgement," which is basically a fancy way of saying they are weighing the risk of a stroke against the risk of a broken bone.
It’s also worth mentioning "White Coat Hypertension." My dad gets it every single time. He sits in that waiting room, smells the antiseptic, sees the blood pressure cuff, and his heart starts racing. His reading will be 155/95. The doctor thinks he's in a crisis. Then he goes home, uses his own monitor while sitting on his recliner, and he’s 122/78.
📖 Related: My eye keeps twitching for days: When to ignore it and when to actually worry
This is why a single reading at the doctor's office is almost useless. To find your actual best blood pressure number, you need a week of data. You need to measure it in the morning, before coffee, and in the evening, after the stress of the day has settled.
The Role of Lifestyle (Beyond Just Cutting Salt)
Everyone talks about salt. "Don't eat the fries!" "Watch the sodium!" Yeah, salt matters, but for some people, it’s not the main driver. Potassium is actually the unsung hero here.
Think of potassium as the "anti-salt." It helps your body flush out sodium and eases the tension in your blood vessel walls. If you’re hunting for your best blood pressure number, you might find it by eating more bananas, avocados, and spinach rather than just obsessing over the salt shaker.
Then there’s sleep. If you have undiagnosed sleep apnea, your blood pressure will be high no matter how many salads you eat. When you stop breathing at night, your body panics. It releases a surge of adrenaline. Your blood pressure spikes. If this happens 30 times an hour, your heart never gets the rest it needs. You can take three different blood pressure medications and still have high numbers if your sleep is a wreck.
What Most People Get Wrong About Medication
There's this weird stigma about taking "the pill." People feel like they failed. "If I just tried harder with my diet, I wouldn't need this."
👉 See also: Ingestion of hydrogen peroxide: Why a common household hack is actually dangerous
Listen. Genetics are real. Some people do everything right—they run 5ks, they eat kale, they meditate—and their blood pressure is still 150/100 because their parents gave them "stiff" genes. In these cases, medication isn't a failure; it’s a tool.
Modern meds like ACE inhibitors or calcium channel blockers aren't just about forcing a number down. They actually protect your organs. They take the "pressure" off the kidneys and the heart muscle. If your best blood pressure number requires a low-dose medication to be reached, that’s a win, not a loss.
Actionable Steps to Finding Your Target
Don't just take a reading and panic. If you want to master your cardiovascular health, follow this protocol:
- Buy a validated home monitor. Check the Stride BP list to make sure your device is actually accurate. Most wrist cuffs are trash; get one that goes around the upper arm.
- The "Rule of Threes." Take your blood pressure three times in a row, with a minute of rest between each. Your first reading is almost always the highest because you’re nervous. Throw it out. Average the second and third.
- The 5-Minute Sit. You cannot walk into the house, drop your keys, and take your pressure. You have to sit still, feet flat on the floor, back supported, for five minutes. No talking. No scrolling on your phone. Just breathe.
- Track the Trends. A single 145/90 isn't a diagnosis. A week of 145/90 is a conversation with your doctor.
- Check the "Dips." Normally, your blood pressure should drop by 10-20% at night. If it doesn't, you're a "non-dipper," which carries a higher risk. This is something only a 24-hour ambulatory monitor can catch, but it’s worth asking your doctor about if your daytime numbers are stubborn.
The best blood pressure number for most healthy adults is now considered to be under 120/80 mmHg. But remember, that's a target, not a law. The real goal is a number that keeps your arteries flexible and your brain sharp without making you feel like a zombie.
Talk to your doctor specifically about your "cardiovascular risk score." They use a tool called the ASCVD Risk Estimator. It takes your blood pressure, your cholesterol, your age, and your smoking status to predict your risk of a heart attack over the next 10 years. If your risk is low, they might be okay with a slightly higher blood pressure. If your risk is high, they’ll want you lower.
Knowledge is power here. Stop chasing a generic number and start chasing the number that's right for your specific biology.
Check your numbers. Log them. Be honest about your stress. That’s how you actually protect your heart.