Doctors in Texas are scared. That’s the simplest way to put it. When you hear about a Texas woman died miscarriage complications, it’s usually not because the medicine doesn't exist. It’s because the law and the medicine are crashing into each other in hospital hallways.
The tragedy isn't just one single event. It’s a pattern. Since the overturn of Roe v. Wade and the implementation of Texas’s SB8 and subsequent "trigger" laws, the medical landscape has turned into a legal minefield. We aren't talking about elective procedures here. We are talking about basic emergency room care for a pregnancy that is already ending.
Miscarriage is common. Really common. About one in four pregnancies ends this way. Most of the time, the body handles it. Sometimes, it doesn't. When it doesn't, you need a doctor to step in immediately to prevent sepsis or hemorrhage. But in Texas, "immediately" has become a relative term.
The Reality Behind the Headlines
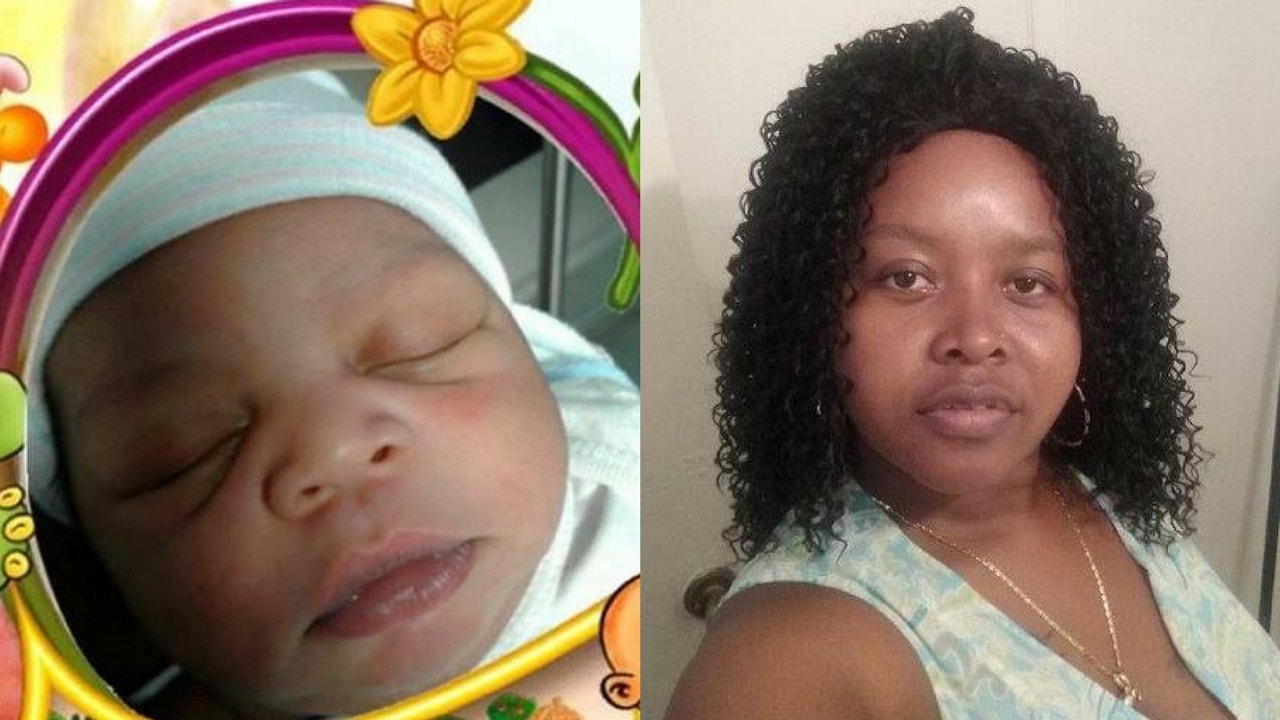
There’s a names people should know, like Josseli Barnica. She was only 28. In 2021, she was 17 weeks pregnant when she started miscarrying. Her husband has been vocal about the fact that they were told the doctors couldn't intervene because the "fetus still had a heartbeat," even though the miscarriage was inevitable and her health was failing. She died of an infection.
It's devastating.
Then there is the case of Nevaeh Crain. She was 18. She went to the emergency room three separate times in one day. Think about that. Three times. She had a fever, she was in pain, and she was clearly septic. But because of the confusion surrounding the legal definition of a "medical emergency," she didn't get the standard of care until it was way too late.
These aren't just "unfortunate incidents." They are systemic failures.
Doctors are essentially being told by hospital legal departments to wait until a woman is "sick enough" to qualify for the life-saving exception. But how sick is "sick enough"? Is it when the blood pressure drops? Is it when the organs start failing? By the time a patient hits those markers, the window to save them is closing fast.
Why the Legal Language is Failing Patients
The Texas law allows for an exception to save the life of the mother. Sounds simple, right? It's not.
The language is vague. It says doctors can act to prevent a "substantial impairment of a major bodily function." Lawyers hate that phrasing. Doctors hate it more. If a doctor gets it wrong, they face life in prison and the loss of their medical license. If you're an OB/GYN who spent a decade in school and hundreds of thousands of dollars on your education, are you going to risk a life sentence on a vague legal definition?
📖 Related: Trump Approval Rating State Map: Why the Red-Blue Divide is Moving
Most won't. They wait for the heartbeat to stop.
The "Chilling Effect" is Real
This isn't some theoretical debate in a courtroom. It’s happening in triage rooms in Houston, Dallas, and Austin. ProPublica has done extensive reporting on this, highlighting how even when the law technically allows for care, the fear of prosecution creates a paralysis.
- Medical boards haven't given clear guidance.
- Hospital systems are prioritizing liability over clinical judgment.
- Doctors are literally Googling the law while patients bleed.
Texas has one of the highest maternal mortality rates in the developed world. Adding a layer of legal terror for physicians hasn't helped. When a Texas woman died miscarriage related issues come up in the news, the immediate reaction from state officials is often that the law is clear and the doctors are just confused.
But if every doctor is confused, the law is the problem, not the doctors.
What "Standard of Care" Actually Means
In a normal world—or at least, the world before 2022—if a woman came in with PPROM (Preterm Premature Rupture of Membranes) at 17 weeks, the doctor would explain that the baby cannot survive. They would offer to induce labor or perform a D&E (dilation and evacuation) to prevent infection.
That is the standard of care.
Now? The standard of care is "watchful waiting." It’s a polite term for watching a woman get closer to death until her vitals are so bad that the legal risk of doing nothing outweighs the legal risk of doing something.
It's a gamble. And women are losing.
The Case of Amanda Zurawski
You might remember Amanda Zurawski. She didn't die, but she almost did. She was told she was miscarrying, but because there was still a heartbeat, she was sent home. She waited until she went into septic shock. She survived, but the infection was so severe one of her fallopian tubes was permanently closed.
👉 See also: Ukraine War Map May 2025: Why the Frontlines Aren't Moving Like You Think
She sued the state. The Texas Supreme Court eventually ruled against the women in that case, basically saying the law’s exceptions were enough. The court's perspective is that doctors should know what to do. The doctors' perspective is that the court isn't the one facing a life sentence if a prosecutor decides to make an example of them.
The Complexity of Medical Definitions
Health isn't a binary. You aren't "fine" one second and "dead" the next. There is a long, agonizing slide in between.
Medical emergencies are often a series of cascading events. A minor infection becomes a systemic one. A small bleed becomes a hemorrhage. In the context of a miscarriage, things can turn south in minutes. If a physician has to call a legal team before they can pick up a scalpel, the patient is already at a disadvantage.
Some argue that the Texas Medical Board should just issue a list of conditions that qualify. But medicine doesn't work that way. Every body is different. Every pregnancy is different. You can't list every possible scenario in a legislative bill.
Misconceptions About Miscarriage Care
A lot of people think "abortion" and "miscarriage care" are two different things. Medically, they often use the exact same procedures and the exact same medications (like misoprostol).
When a law bans "abortion," it inadvertently sweeps up miscarriage management. A D&E is the surgical procedure used for both. If a pharmacy is scared to dispense misoprostol because it could be used for an elective abortion, a woman having a natural miscarriage can't get the medicine she needs to pass the tissue safely at home.
This overlap is where the danger lives.
What Needs to Change
Honestly, the blame game doesn't save lives. Politicians blame doctors for not being brave enough. Doctors blame politicians for writing bad laws. Hospital boards blame everyone to protect their bottom line.
But the data is hard to ignore.
✨ Don't miss: Percentage of Women That Voted for Trump: What Really Happened
The Texas Maternal Mortality and Morbidity Review Committee has noted that a huge percentage of pregnancy-related deaths are preventable. If we want to stop hearing about how a Texas woman died miscarriage complications, we need a "safe harbor" for physicians.
This means:
- Clear, statutory protection for doctors who act in "good faith" to treat a miscarriage.
- Removing the threat of life imprisonment for medical decisions.
- Requiring hospitals to prioritize the stabilization of the mother over the presence of a fetal heartbeat when a miscarriage is medically inevitable.
It’s not about politics. It’s about not letting people die from 19th-century complications in 21st-century hospitals.
Actionable Steps for Pregnant Women in Texas
If you are pregnant or planning to be in Texas, the reality is that the healthcare system is currently unstable. You have to be your own strongest advocate.
Know the warning signs of a failing pregnancy. If you experience heavy bleeding (soaking through a pad an hour), extreme abdominal pain, or a high fever, you need an ER immediately.
Ask the hard questions now. If you are seeing an OB/GYN, ask them directly: "What is your hospital's policy if I have a miscarriage and my life is at risk but there is still a fetal heartbeat?" If they can't give you a straight answer, find a different provider or a different hospital system.
Bring an advocate. Never go to the ER alone. You need someone there who can demand answers and document what the doctors are saying. If they refuse treatment, ask them to document the refusal and the specific medical reason for it in your chart.
Keep records. Get copies of your ultrasounds and lab results. If you have to move to a different state for care—which many Texas women are now doing—having your records ready can save precious hours.
Understand your legal rights. While the law is restrictive, Federal law (EMTALA) still requires hospitals to stabilize patients in emergency situations. This is currently a major point of contention between the federal government and Texas, but it remains a tool for advocacy.
The situation in Texas is a stark reminder that when policy ignores clinical reality, the consequences are measured in human lives. Staying informed and proactive is the only way to navigate a system that is currently failing its most vulnerable patients.
Resources for Support
- Postpartum Support International (PSI): Offers resources for miscarriage and loss.
- REACH Fund of Texas: Provides information on navigating reproductive healthcare in the state.
- Maternal Health Hotlines: Many non-profits now offer 24/7 lines for women in medical crises to understand their options.
The goal is to ensure that no more families have to experience the preventable loss of a loved one due to legal confusion and medical hesitation.