It sounds like a horror movie prop. You’re looking at a medical image or reading a pathology report, and there it is: a mass containing fully formed molars, long strands of hair, and maybe even bits of bone or cartilage. This is a teratoma with teeth and hair, and honestly, it’s one of the most misunderstood phenomena in modern medicine. People often freak out. They assume they’ve absorbed a twin in the womb or that something "sentient" is growing inside them.
The reality is actually more fascinating—and a lot more biological—than those urban legends suggest.
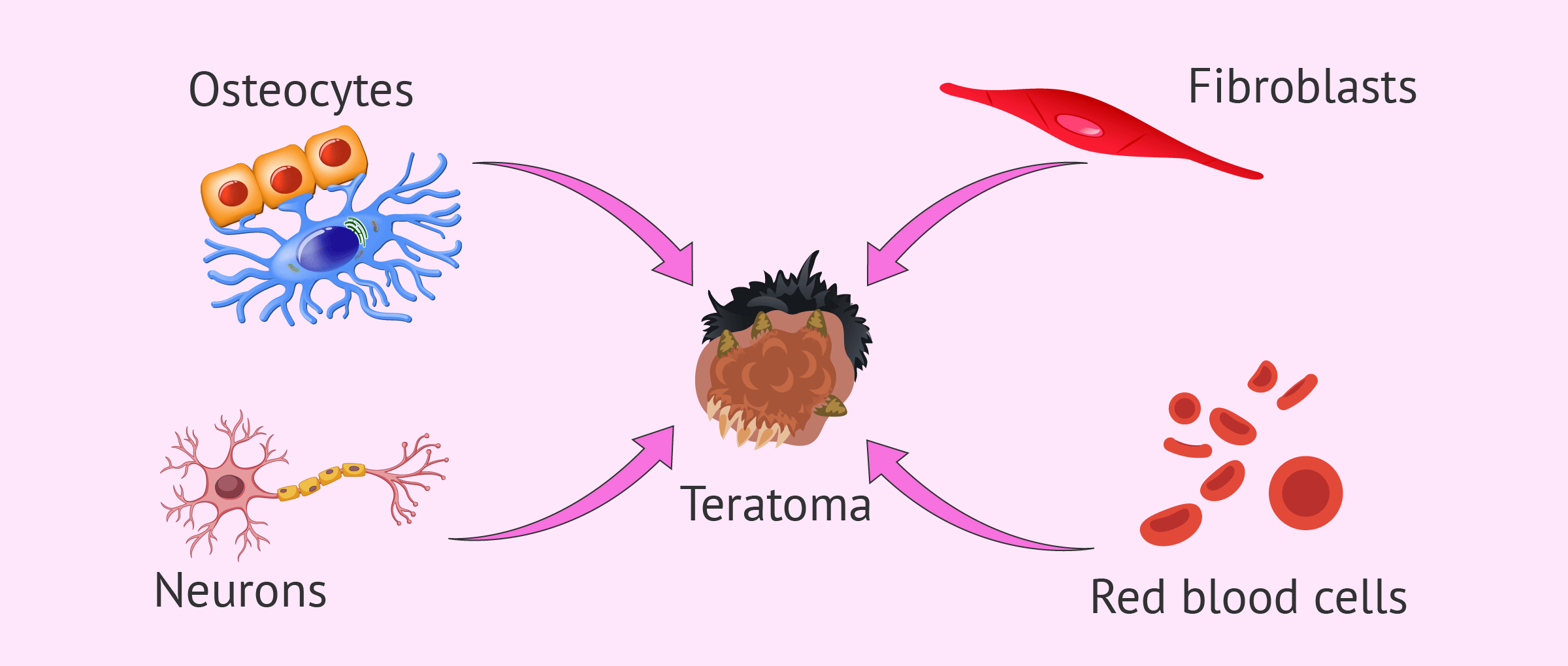
These aren't "babies." They aren't even "people" in any sense of the word. They are essentially a biological glitch. A teratoma is a type of germ cell tumor. To understand it, you have to think about how a human body is built from scratch. Usually, a cell has a specific job. A skin cell makes skin; a heart cell makes heart tissue. But germ cells are the "master cells." They are pluripotent, which is just a fancy way of saying they have the potential to become absolutely anything. When these cells go rogue and start dividing haphazardly, they don't just make a lump of uniform tissue. They start following their internal blueprints to create complex structures.
Why Teeth and Hair Show Up in a Teratoma
Most tumors are just a mass of the same kind of cell. If you have a lipoma, it's just fat. If you have a fibroid, it's muscle. A teratoma is different because it contains tissues from all three "germ layers": the endoderm, mesoderm, and ectoderm.
Think about the ectoderm for a second. In a developing embryo, the ectoderm is responsible for creating your skin, your hair, and your tooth enamel. Because these tumors often arise from germ cells that are heavily skewed toward ectodermal development, they frequently produce very high-quality hair and teeth. It’s not uncommon for a surgeon to open a dermoid cyst (a common type of mature teratoma) and find a "nest" of hair soaked in sebum—the oily stuff your skin produces—along with multiple teeth embedded in a piece of bone that looks suspiciously like a jaw.
It’s weird. It’s definitely jarring. But it’s a result of your body’s own building blocks getting their signals crossed.
The "Vanished Twin" Myth
We need to address the elephant in the room. You’ve probably seen a viral social media post or a tabloid headline claiming a woman "gave birth" to her own twin via a tumor.
👉 See also: Nuts Are Keto Friendly (Usually), But These 3 Mistakes Will Kick You Out Of Ketosis
That’s basically never what’s happening.
There is a very rare condition called fetus in fetu, where a malformed fetus is found inside the body of its twin. But that is distinct from a teratoma with teeth and hair. In fetus in fetu, there is a visible spinal column and a high degree of organization. In a teratoma, it’s total chaos. You might find a tooth next to a piece of brain tissue, which is right next to a patch of intestinal lining. There is no umbilical cord. There is no placenta. It’s just a disorganized library of human parts.
Where They Hide: Ovaries, Testes, and Tailbones
Where do these things actually grow? Most often, we see them in the ovaries. These are called "mature cystic teratomas" or dermoid cysts. About 20% of all ovarian tumors are dermoids. They’re usually benign. You might go in for a routine ultrasound because of some bloating or pelvic pain, and the technician sees a "highly echogenic" mass. That’s the medical way of saying the mass is so dense—because of the teeth and bone—that it’s bouncing the sound waves right back.
But they aren't exclusive to women.
Men can get them in the testes, though in adults, these tend to be more aggressive (malignant) than the ovarian versions. You also see them in newborns, specifically at the base of the tailbone. This is called a sacrococcygeal teratoma. It happens because that area is a "hub" for germ cells during embryonic development. Sometimes, a few of those cells get left behind, lose the script, and start building teeth where a tailbone should be.
The Brain Connection: Anti-NMDA Receptor Encephalitis
Here is the part that sounds like actual science fiction. Sometimes, a teratoma with teeth and hair—specifically one that contains brain tissue—can cause someone to lose their mind.
✨ Don't miss: That Time a Doctor With Measles Treating Kids Sparked a Massive Health Crisis
It’s a condition called Anti-NMDA Receptor Encephalitis.
Because the tumor contains neural tissue, the body’s immune system recognizes that tissue as "foreign" and starts attacking it. But because the tumor’s brain tissue looks just like the person’s actual brain tissue, the antibodies start attacking the patient's real brain, too. This leads to hallucinations, seizures, and personality changes. Dr. Souhel Najjar famously diagnosed this in journalist Susannah Cahalan (the author of Brain on Fire). Once the teratoma is surgically removed, the "madness" often disappears. It’s a perfect example of how a physical mass can manifest as a psychiatric crisis.
How Doctors Deal With It
If you have one of these, you can’t just "wait and see." They don’t dissolve on their own.
- Imaging: Usually, a CT scan or an MRI is the gold standard. Teeth and bone show up very clearly on a CT, making the diagnosis relatively straightforward.
- Surgical Removal: This is the only real fix. For ovarian teratomas, surgeons often perform a cystectomy, where they shell the tumor out and leave as much of the healthy ovary as possible.
- Pathology: Once it’s out, a pathologist slices it up and looks at it under a microscope. They’re looking for "immature" cells. If the cells are all mature (like fully formed skin or adult-looking teeth), it’s benign. If there are embryonic-like, immature cells, it’s considered malignant and might require further treatment like chemo.
Most people recover perfectly. Once the "host" tissue is gone, the body stops reacting to it.
Common Misconceptions
People think these things are "eating" them. They aren't. A teratoma is a parasite only in the sense that it uses your blood supply to grow. It’s not trying to form a person. It has no consciousness. It’s just a biological accident.
Another big one: "Did I grow this because of something I did?" No. These are congenital or arise from spontaneous cellular mutations. There’s no diet, lifestyle choice, or environmental toxin that’s been definitively linked to causing a teratoma with teeth and hair. It’s mostly just bad luck in the cellular lottery.
🔗 Read more: Dr. Sharon Vila Wright: What You Should Know About the Houston OB-GYN
What You Should Actually Do
If you’ve been diagnosed with one, don’t spiral down a Reddit rabbit hole.
First, get the specifics from your doctor about whether it's "mature" or "immature." This is the most important distinction for your prognosis. Mature teratomas are common and almost always cured by surgery.
Second, pay attention to symptoms that seem unrelated. Are you having weird memory gaps? Heart palpitations? Dermoids can sometimes produce hormones or trigger those aforementioned autoimmune responses.
Third, if you’re planning on having kids later, talk to your surgeon about "ovarian-sparing" techniques. Modern robotic surgery is incredibly precise. They can often remove a large teratoma while keeping the rest of the ovary functional.
Finally, stop calling it a twin. It’s weird enough as it is without adding a ghostly sibling into the mix. It’s a tumor. It’s a collection of misplaced instructions. It’s a medical marvel, sure, but it’s one that we know how to treat.
Actionable Next Steps
- Confirm the Pathology: Ensure your doctor has sent the tissue for a full microscopic review to rule out any immature (malignant) components.
- Monitor the Other Side: If you had an ovarian teratoma, there is about a 10-15% chance one could develop on the other ovary later in life. Keep up with your annual pelvic exams.
- Check Your Blood: In some cases, doctors check tumor markers like AFP (Alpha-fetoprotein) or hCG to ensure the tumor isn't producing specific proteins associated with more aggressive growths.
- Review Your Symptoms: If you’ve felt "off" mentally or emotionally leading up to the discovery, mention this to your neurologist or GP; the link between these tumors and the immune system is significant.