Honestly, when most of us think about heart attacks or cardiovascular failure, we picture the Hollywood version. You know the one. A man in his fifties suddenly clutches his chest, gasps for air, and collapses onto the floor in a dramatic heap. It’s terrifying. But it’s also kinda misleading because that’s not how it usually goes down in real life.
Heart disease is sneaky.
It doesn't always scream; often, it whispers for years before it finally breaks something. Symptoms of heart disease can be as subtle as feeling a bit more winded than usual when you're carrying groceries or having a weird ache in your jaw that you’ve been blaming on a toothache for three weeks. If you’re waiting for the "elephant on the chest" feeling to tell you something is wrong, you might be waiting too long.
According to the American Heart Association (AHA), cardiovascular disease remains the leading cause of death globally, but the way it manifests is vastly different between a 40-year-old woman and a 70-year-old man. We need to talk about the nuance. We need to talk about why your "indigestion" might actually be your arteries struggling to move blood.
The weird truth about chest pain and "discomfort"
We’ve been conditioned to look for "pain." Doctors, however, prefer the word "discomfort." This is a huge distinction. People who end up in the ER often describe the feeling not as a sharp stabbing, but as a heaviness, a tightness, or even just a "fullness" in the center of the chest. It’s the sensation of a balloon being inflated where it shouldn't be.
Sometimes it lasts a few minutes, goes away, and then comes back. This is often Angina. Basically, your heart muscle isn't getting enough oxygen-rich blood because a coronary artery is narrowed.
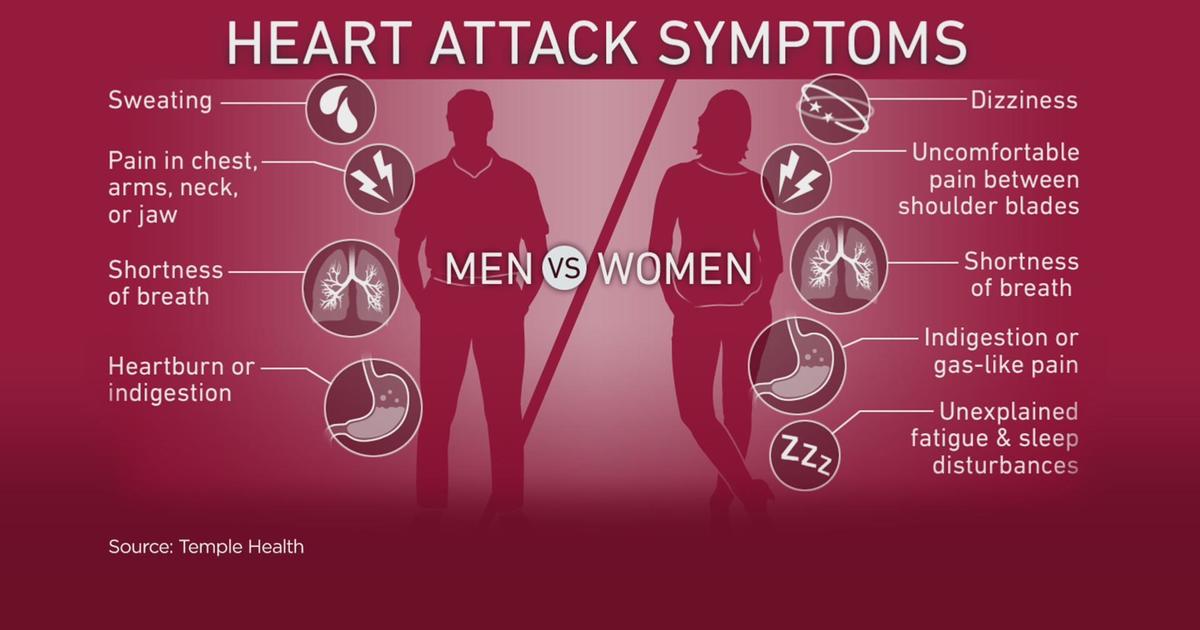
But here is the kicker: some people feel absolutely nothing in their chest. Women, in particular, are notorious for having "atypical" presentations. Instead of chest pressure, a woman might experience profound fatigue—the kind where you feel like you’ve run a marathon when you’ve only walked to the mailbox. Or she might feel a burning sensation in her upper abdomen that feels exactly like acid reflux.
Dr. Nanette Wenger, a pioneer in geriatric cardiology at Emory University, has spent decades pointing out that clinical trials historically ignored these differences. If you’re a woman, your symptoms of heart disease might involve nausea, lightheadedness, or pain in the shoulder blades. Don't let a doctor tell you it’s just anxiety without a full workup.
✨ Don't miss: Why Sometimes You Just Need a Hug: The Real Science of Physical Touch
When your "fitness" hides the problem
There’s this phenomenon with athletes or very active people where they rationalize symptoms away. You’re a runner, so when you feel a little short of breath, you assume it’s just a bad training day or the humidity. You’re "too fit" for heart issues, right?
Wrong.
Hypertrophic cardiomyopathy or even standard plaque buildup doesn't care about your VO2 max. If you notice a sudden, unexplained drop in your exercise tolerance—like a hill that used to be easy now feels impossible—that is a massive red flag. It’s not just "getting older." It’s a physiological shift.
The legs tell a story
We often forget that the heart is just the pump for a massive, body-wide plumbing system. If the pump is struggling, the pipes in your legs will show it. This is called Peripheral Artery Disease (PAD).
- You get cramps in your calves when you walk.
- The hair on your legs stops growing.
- Your feet feel cold even when the room is warm.
- Sores on your toes that won't heal.
If your legs hurt when you move but feel better when you sit, your arteries are likely clogged. This is a systemic issue. If the pipes in your legs are blocked, the pipes in your heart are probably under pressure too.
The "silent" symptoms you’re ignoring right now
Let’s talk about sleep. If you’ve started snoring loudly or waking up gasping for air, you might have sleep apnea. While that’s a respiratory issue, it puts an insane amount of stress on the heart. Every time you stop breathing, your oxygen levels plummet and your heart has to kick into overdrive to keep you alive. Over time, this leads to atrial fibrillation (Afib) or heart failure.
Then there’s the swelling. Edema.
🔗 Read more: Can I overdose on vitamin d? The reality of supplement toxicity
If you notice that your socks are leaving deep, lasting indentations in your ankles by 5:00 PM, or your rings are suddenly too tight, it’s not just "water weight." When the heart can't pump efficiently, blood backs up in the veins. This forces fluid into the body tissues. Your kidneys also start to struggle with salt and water excretion. It’s a snowball effect.
Is it just a "flu" or something else?
Many people who suffer a "silent" heart attack—which accounts for nearly 45% of all heart attacks according to some studies—mistake the event for a bad bout of the flu. They feel achy. They have a cold sweat. They feel "off."
A study published in Circulation highlighted that these silent events are just as dangerous as the "big ones" because they leave behind scar tissue. That scar tissue interferes with the heart's electrical system, setting the stage for future arrhythmias. If you have "the flu" but no fever and no cough, and you just feel an impending sense of doom? Get an EKG.
Understanding the "referred pain" map
Your brain is actually pretty bad at pinpointing where internal pain is coming from. The nerves from your heart and the nerves from your arm or jaw travel the same pathways to the brain. This is why symptoms of heart disease often show up in places that seem totally unrelated to the chest.
- The Left Arm: This is the classic one, but it can also happen in the right arm.
- The Jaw: Specifically the lower jaw. It’s often mistaken for a dental issue or TMJ.
- The Neck: A feeling of choking or a tight throat.
- The Upper Back: Pain between the shoulder blades that doesn't feel like a pulled muscle.
If these pains appear when you're physically exerting yourself and vanish when you rest, that is a textbook sign of cardiac issues. It’s called "exertional" pain.
Why the "widowmaker" is a terrifying misnomer
We need to stop using the term "widowmaker" as if heart disease only happens to men. While the Left Anterior Descending (LAD) artery blockage is what that term refers to, it's just as deadly for women. The problem is that women are often diagnosed later because their symptoms don't fit the 1950s medical textbook definition.
In 2026, we know better. High blood pressure during pregnancy (preeclampsia) is now recognized as a massive risk factor for heart disease later in life. If you had issues during pregnancy twenty years ago, you are at a higher risk today. This is the kind of nuance that saves lives.
💡 You might also like: What Does DM Mean in a Cough Syrup: The Truth About Dextromethorphan
What you should actually do today
If you’ve been reading this and thinking, "Wait, I actually do get that weird jaw pain," don't panic. Panic makes your heart rate spike, which doesn't help anyone. Instead, take a structured approach to your health.
Start tracking the triggers. Does the discomfort happen after a big meal? (Could be gallbladder, could be heart). Does it happen when you’re stressed? Does it happen when you walk up stairs? Write down the date, what you were doing, and how long it lasted.
Get a blood panel that actually matters. Most people just get "total cholesterol." That’s outdated. You want to look at your ApoB levels. Apolipoprotein B is a much more accurate predictor of cardiovascular risk than just LDL alone. It measures the number of potentially "bad" particles in your blood. Ask your doctor for a Lipoprotein(a) test too—it’s a genetic marker that most doctors don't test for unless you ask, and it can explain why "healthy" people have sudden heart attacks.
Check your own pulse. Literally. Put two fingers on your wrist. Is it steady like a metronome? Or does it skip a beat, then race, then slow down? An irregular pulse could be Atrial Fibrillation, which increases your stroke risk by five times.
Next steps for immediate action:
- Schedule a Calcium Score (CAC) test: This is a quick CT scan that looks for actual calcified plaque in your heart arteries. It’s often more useful than a standard stress test for early detection.
- Invest in a blood pressure cuff: Checking it at the doctor’s office once a year is useless because of "white coat syndrome." Check it at home, at rest, and keep a log.
- Audit your sleep: If your partner says you stop breathing, get a sleep study. Do not wait.
- Recognize the "Sense of Doom": It sounds unscientific, but many heart attack survivors report a sudden, overwhelming feeling that something is horribly wrong right before physical symptoms escalate. Trust your gut.
The reality is that symptoms of heart disease are manageable if you catch them before the "big event." The technology we have now—from wearable EKG monitors to advanced lipid testing—means nobody should be surprised by a heart attack. Be the person who "overreacts" to a weird symptom. It’s much better to be told it’s just heartburn than to ignore a warning sign your body is desperate for you to notice.