Let’s be honest. Most guys don't spend a lot of time thinking about their bathroom habits. You go, you flush, you move on with your day. But that's exactly how the early symptoms of colon cancer men often fly under the radar for months or even years. It starts with a little bit of fatigue that you blame on a long week at work, or maybe a weird cramp you figure was just that sketchy taco truck lunch.
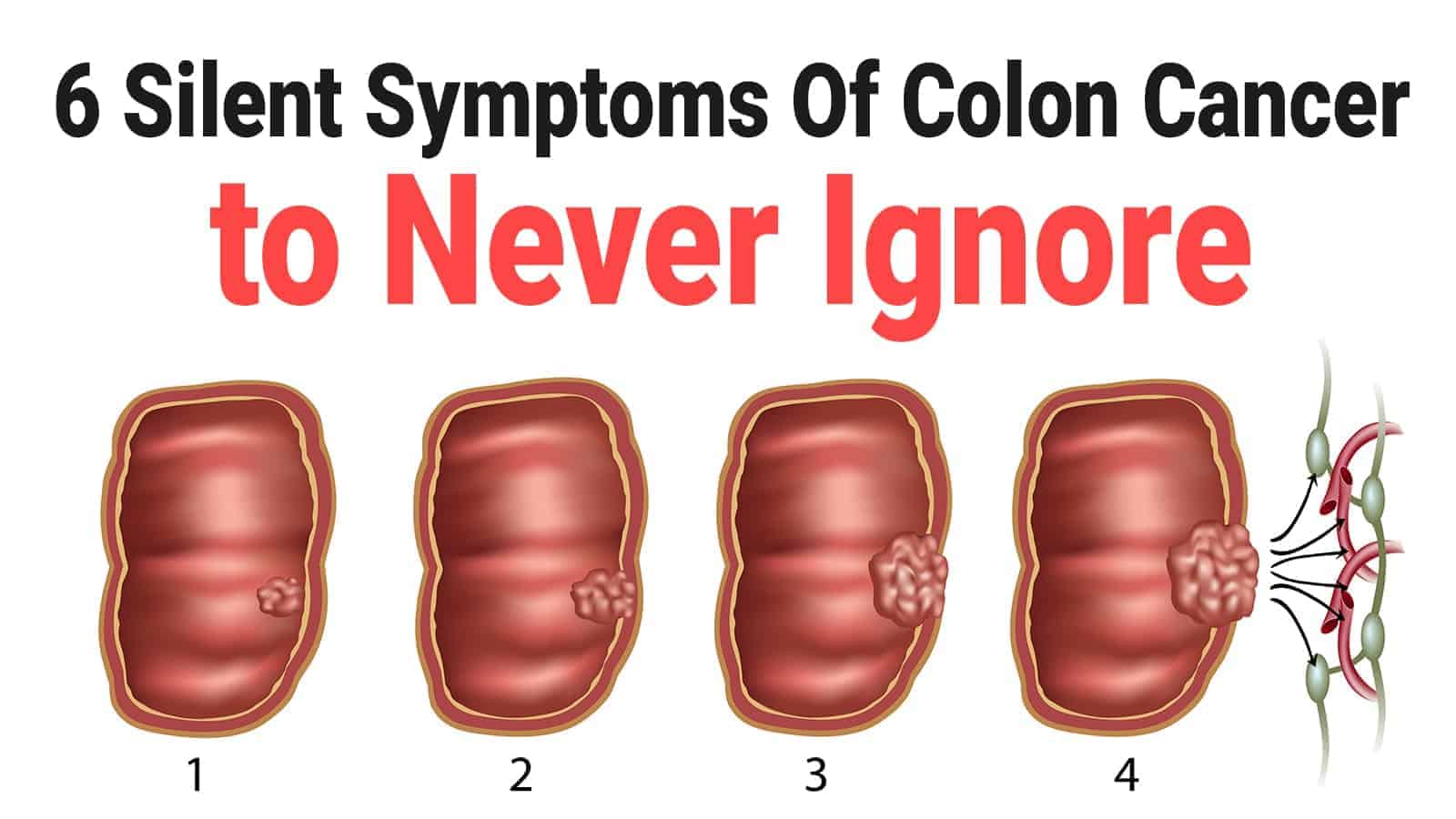
But colon cancer—medically known as colorectal cancer—is currently the second leading cause of cancer deaths in the United States. That's a heavy statistic. What's even more frustrating for doctors is that it is incredibly treatable if you catch it while it's still just a tiny polyp. The problem? Men are statistically more likely to delay screenings or shrug off "minor" stomach issues compared to women.
We need to talk about what’s actually happening in your gut.
The Red Flags: Symptoms of Colon Cancer Men Need to Watch
Blood is the big one. If you see bright red streaks on the toilet paper, your brain probably goes straight to "hemorrhoids." And honestly? You’re usually right. Hemorrhoids are common. But here's the kicker: you can have hemorrhoids and a tumor at the same time. Never assume one explains away the other.
The color of the blood matters a lot. Bright red usually means the bleeding is happening near the exit, like the rectum. If the blood is dark, tarry, or makes your stool look like coffee grounds, that’s "old" blood coming from higher up in the colon. That is a massive warning sign.
🔗 Read more: How to Eat Chia Seeds Water: What Most People Get Wrong
The "Thin Stool" Mystery
Have you noticed your poop looks different lately? I’m not talking about the occasional bout of diarrhea. I mean a permanent change. Doctors often look for "pencil stools." If a tumor is growing inside the colon, it narrows the passage. As the waste passes through that narrowed "pipe," it gets squeezed into a thin, ribbon-like shape. If your stool used to be robust and now it’s consistently thin for more than a couple of weeks, that’s not your diet. That’s an obstruction.
That Weird Feeling You Aren't Quite Done
There is a medical term called tenesmus. It’s that nagging, frustrating sensation that you need to have a bowel movement even though your bowels are already empty. You sit there, you strain, and nothing happens. This happens because a tumor in the rectal area can trick your nerves into thinking there is still stool present. It’s an incredibly annoying symptom that men often mistake for simple constipation or a need for more fiber.
Why Is This Happening to Younger Guys?
For decades, we thought of this as an "old man's disease." Not anymore. The American Cancer Society has been sounding the alarm because the rates of colorectal cancer in people under 50 have been climbing steadily since the mid-1990s.
We don't fully know why. Some researchers point to the "Western Diet"—lots of red meat, processed sugars, and not enough leafy greens. Others look at environmental factors or changes in gut bacteria. Whatever the cause, the "wait until you're 50" rule is dead. The new official recommendation for a first colonoscopy is age 45. If you have a family history, like a dad or brother who had it, you might need to go even earlier.
💡 You might also like: Why the 45 degree angle bench is the missing link for your upper chest
The Silent Symptoms: It Isn't Always About the Bathroom
Sometimes the most dangerous symptoms of colon cancer men experience have nothing to do with the toilet.
- Unexplained Weight Loss: If you’re dropping pounds without hitting the gym harder or cutting calories, your body is burning energy to fight something. Cancer cells consume a lot of the body's energy supply.
- Anemia and Iron Deficiency: Tumors often bleed microscopically. You won't see this blood in the bowl. However, over months, that slow leak leads to iron-deficiency anemia. If your doctor tells you your iron is low, ask why. Men shouldn't be anemic without a clear reason like internal bleeding.
- Shortness of Breath: This ties back to the anemia. Less iron means less oxygen in your blood. You might find yourself huffing and puffing while walking up a flight of stairs that used to be easy.
"A lot of men come in complaining of fatigue. They think it's just stress or getting older. But when we run the blood work and see the low hemoglobin, that's when the bells start ringing," says Dr. Mark Pochapin, a leading gastroenterologist at NYU Langone.
Abdominal Pain vs. Normal Bloating
Gas happens. We all get bloated after a heavy meal. But the pain associated with colon cancer feels different. It’s often a dull, persistent ache or a cramp that doesn't go away after you use the bathroom. It might feel like a "full" sensation in your abdomen that persists for days. If you’re reaching for the Tums or Pepto-Bismol every single day for a month, you’re masking a symptom that needs an actual diagnosis.
The Role of Genetics and Ethnicity
It's not a level playing field. Black men have the highest incidence and mortality rates of colorectal cancer in the United States. The reasons are a complex mix of genetics and systemic healthcare disparities, but the takeaway is clear: if you are a Black man, being proactive about these symptoms is literally a matter of life and death.
📖 Related: The Truth Behind RFK Autism Destroys Families Claims and the Science of Neurodiversity
Also, look at your family tree. If a first-degree relative had colon cancer or even "precancerous polyps," your risk doubles. You can't change your DNA, but you can change how closely you monitor your health.
What Happens During a Screening?
The word "colonoscopy" makes most men want to run for the hills. Let's demystify it. You aren't awake for it. You get some of the best sleep of your life thanks to a sedative like Propofol. The "prep"—the day before when you have to drink the liquid that clears you out—is honestly the worst part.
The procedure itself takes about 20 minutes. The doctor uses a tiny camera to look for polyps. Polyps are small growths that aren't cancer yet, but they could become cancer in 5 to 10 years. If the doctor finds one, they snip it out right then and there.
You just prevented cancer. There are also at-home tests like Cologuard. You poop in a box and mail it to a lab. They look for DNA changes. It’s better than nothing, but if it comes back positive, you still have to get the colonoscopy. It’s also not as good at finding those "pre-cancer" polyps as a visual exam.
Actionable Steps for Men Right Now
- Audit your bathroom habits. For the next week, actually look before you flush. Note changes in color, consistency, or frequency.
- Check your family history. Call your parents or siblings. Find out exactly who had what and at what age.
- Schedule the "Baseline." If you are 45 or older, call a GI doctor today. Don't wait for a symptom to appear.
- Eat more fiber. Aim for 30-38 grams a day. It acts like a broom for your colon, scrubbing the walls and keeping things moving. Think beans, broccoli, and whole grains.
- Limit the red stuff. You don't have to go vegan, but cutting back on processed meats like bacon, deli meats, and hot dogs significantly lowers your risk.
The bottom line is that you know your body better than anyone else. If something feels "off" in your gut, don't let embarrassment keep you out of the doctor's office. A 20-minute uncomfortable conversation can add 20 years to your life. Take the symptoms seriously, get the screen, and keep moving. No excuses.