Look around your local coffee shop. Statistically, someone in that room—maybe the barista, maybe the guy in the corner on his laptop—is struggling with a substance use disorder. It’s not just a "them" problem. It's an "us" problem.
Honestly, we talk about substance abuse awareness like it’s a brochure you find in a doctor’s office. We use these sterile, clinical terms that make it feel like something happening in a lab. But for the 48.7 million Americans aged 12 or older who dealt with a substance use disorder in 2023, it’s not clinical. It’s raw. It’s the Monday morning you can't get out of bed because your brain is screaming for a chemical that makes you feel "normal." It's the quiet panic of a parent realizing the medicine cabinet looks a little too empty.
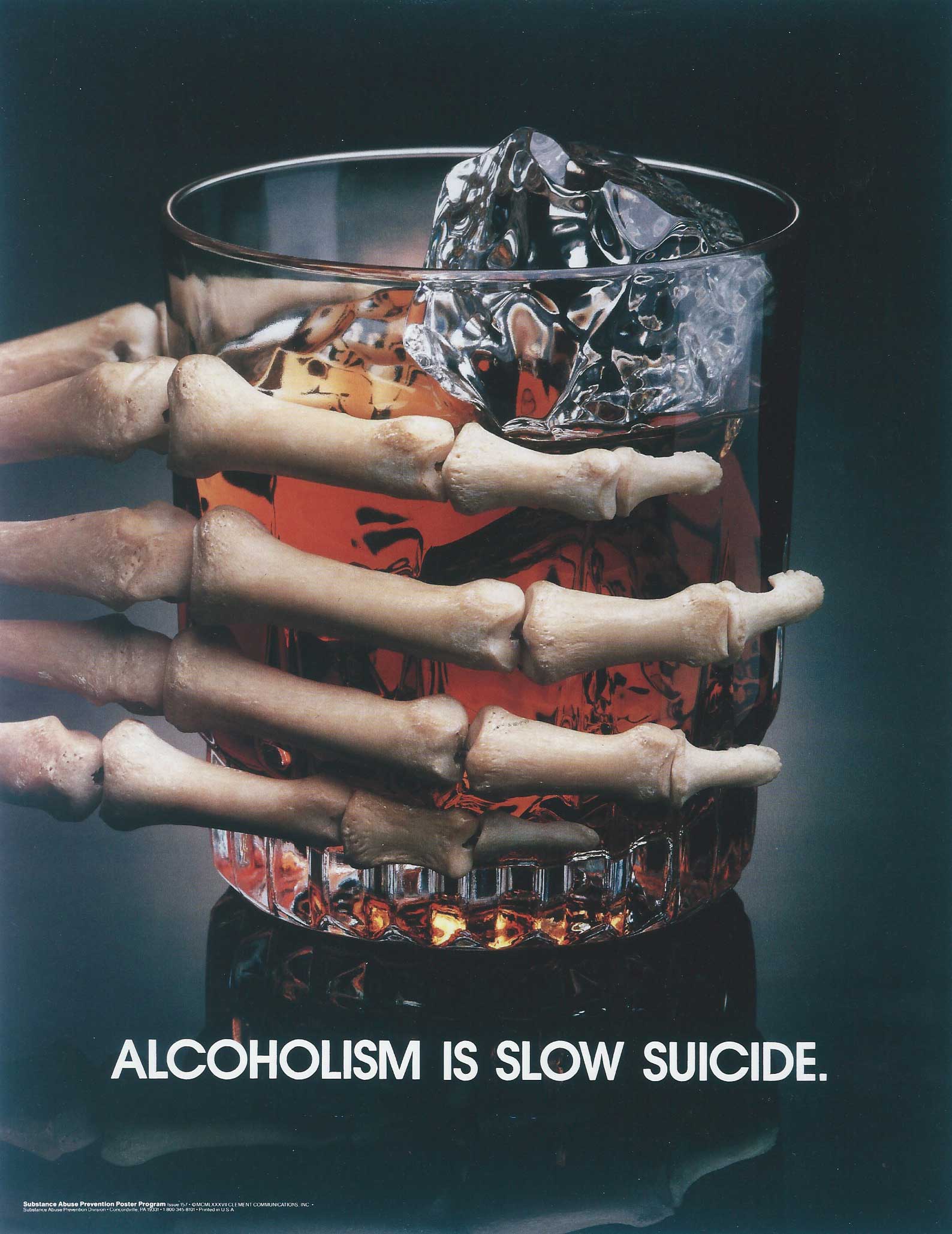
The Substance Abuse and Mental Health Services Administration (SAMHSA) releases data every year, and the numbers are staggering, yet we somehow become numb to them. We see a graph and think, "That's a lot," and then we go back to scrolling. But awareness isn't just knowing a statistic exists; it's understanding the mechanics of how we got here and why the stigma is still killing people faster than the drugs themselves.
The Science We Usually Skip Over
Most people think of addiction as a series of bad choices. That’s a massive oversimplification that actually hinders substance abuse awareness. When someone uses a substance—be it alcohol, opioids, or stimulants—the brain's reward system gets hijacked. Specifically, the basal ganglia, which handles our "pleasure" circuits, gets flooded with dopamine.
Dr. Nora Volkow, the Director of the National Institute on Drug Abuse (NIDA), has spent decades explaining that addiction is a chronic, relapsing brain disease. It’s not a lack of willpower. Think of it like this: if you have a broken leg, you can't just "will" yourself to run a marathon. The neural pathways in the prefrontal cortex—the part of the brain that handles decision-making and impulse control—literally change their physical structure. You're trying to make a logical decision with a tool that is physically compromised.
It’s not just about the high
People use because they want to stop feeling bad. This is the "self-medication" hypothesis. Maybe it’s untreated trauma. Maybe it’s a high-stress job in a culture that celebrates "hustle" at the cost of sanity. According to the Journal of the American Medical Association (JAMA), roughly half of people with a severe mental disorder also struggle with substance use. If we don't talk about mental health, we aren't actually talking about awareness. We're just looking at the tip of the iceberg and wondering why the ship is sinking.
Why the Current Narrative is Failing
We’ve spent decades on "Just Say No" campaigns. They didn't work. In fact, they might have made things worse by shaming people into silence.
Real substance abuse awareness requires us to look at the social determinants of health. If you live in a zip code with high unemployment, limited access to green spaces, and a "food desert" where the only affordable calories are at a gas station, your risk profile is different. Dr. Gabor Maté, a renowned expert on addiction, often asks not "Why the addiction?" but "Why the pain?" We are a society in pain. We have an isolation epidemic. U.S. Surgeon General Vivek Murthy has pointed out that loneliness can be as damaging to health as smoking 15 cigarettes a day. When people lack connection, they find it in a bottle or a pill.
- Stigma prevents 90% of people with a substance use disorder from seeking treatment.
- Language matters: "Addict" is a label; "Person with a substance use disorder" is a human being.
- Harm reduction saves lives, even if it feels "controversial" to some.
The Fentanyl Shift: Why This Isn't Your Parents' Crisis
The game changed. If you haven't looked at the toxicology reports lately, you should. Fentanyl is a synthetic opioid that is 50 to 100 times more potent than morphine. It’s everywhere. It’s being pressed into fake Xanax pills and mixed into cocaine. This is why substance abuse awareness in 2026 has to be about more than "don't do drugs." It has to be about Narcan (Naloxone).
If you don't have a Narcan kit in your bag or your car, why not? You don't need to be a drug user to carry it. You just need to be someone who cares about their neighbors. It’s a nasal spray. It’s easier to use than a fire extinguisher. And yet, there's still this weird pushback—this idea that having Narcan "enables" users. That’s like saying having a life jacket enables people to fall off boats. It doesn't. It just keeps them from drowning.
The Myth of the "Rock Bottom"
We need to stop waiting for people to hit rock bottom. Rock bottom is often a morgue.
The "tough love" approach—kicking someone out, cutting them off completely—is sometimes necessary for the family's safety, but as a universal treatment philosophy? It's outdated. Research from the Partnership to End Addiction shows that early intervention is significantly more effective. If you see someone struggling, you talk to them now. You don't wait for them to lose their job or their home.
What Recovery Actually Looks Like (Hint: It's Not a Straight Line)
Recovery isn't a 28-day stint in a fancy Malibu rehab center with organic kale smoothies. For most, it's a lifelong process of managing a chronic condition. It involves Medication-Assisted Treatment (MAT), like Buprenorphine or Methadone, which are evidence-based tools that help stabilize brain chemistry.
🔗 Read more: Does Apple Cider Vinegar Give You Gas? What the Science Really Says
There's a lot of "recovery elitism" out there. Some people think that if you're on MAT, you aren't "really" sober. That’s dangerous nonsense. If a person is holding down a job, reconnecting with their kids, and not overdosing in a bathroom stall because they're using a prescribed medication to manage their cravings, that is a massive victory. We need to celebrate all pathways to recovery, whether it's 12-step programs, SMART Recovery, or purely clinical intervention.
Actionable Steps for Genuine Awareness
It’s easy to read an article and feel bad. It’s harder to do something. If you actually want to move the needle on substance abuse awareness, you have to get your hands a little dirty.
1. Audit your medicine cabinet tonight.
Most people who misuse prescription opioids get them from a friend or relative. Don't "save" those leftover Percocets from your wisdom tooth surgery. Find a drug take-back location. Many pharmacies have anonymous drop boxes. Use them.
2. Change your vocabulary.
Next time you're tempted to call someone a "junkie" or "crackhead," stop. Even in private. The language we use shapes the empathy we feel. Refer to it as a "substance use disorder" or "struggling with use." It sounds clunky at first. Do it anyway. It reduces the barrier for someone to ask for help.
3. Get Narcan and learn how to use it.
You can get it over the counter at most pharmacies now. Many community health centers give it away for free. Watch a two-minute YouTube video on how to administer it. You might never use it. But if you do, you'll be the reason someone gets a second chance at life.
4. Push for workplace changes.
If you're in a leadership position, look at your company's insurance policy. Does it cover mental health and addiction services at the same level as physical health? Does your culture encourage people to take "mental health days" without being judged? Substance abuse thrives in high-pressure, low-support environments.
5. Support Harm Reduction.
This means needle exchanges, supervised injection sites, and fentanyl test strips. These things are often politically unpopular, but the data is clear: they reduce the spread of HIV and Hepatitis C, and they decrease overdose deaths. They also provide a touchpoint where social workers can connect with users and offer treatment options when they're ready.
👉 See also: People Getting Struck by Lightning: What the Movies Always Get Wrong
Real awareness isn't a ribbon you wear for a month. It’s a fundamental shift in how we view human struggle. It’s acknowledging that the line between "us" and "them" is incredibly thin, often just a single traumatic event or a bad prescription away. We have to stop looking for someone to blame and start looking for ways to heal.