You're sitting there. Waiting. Straining. Nothing happens. Or maybe, weirdly, there’s a bit of watery diarrhea leaking out, which makes zero sense because you feel like you’re carrying a literal brick in your lower gut. That’s the hallmark of fecal impaction. It’s not just "being a little backed up." It’s a physical blockade. When you need to know what to do impacted stool becomes a priority that overrides everything else in your day. It’s uncomfortable. It’s embarrassing to talk about. Honestly, it can even be dangerous if you handle it wrong or wait too long.
Most people think they just need more fiber. Stop right there. If you are truly impacted—meaning the stool is a dry, hard mass wedged in the rectum that won't budge—dumping a bunch of Metamucil on top of it is like adding more cars to a massive traffic jam. It doesn’t clear the wreck; it just makes the line longer. We need to talk about how this actually happens and the specific, step-by-step ways to resolve it without ending up in the emergency room, though sometimes, that’s exactly where you need to be.
Why things get stuck in the first place
It’s usually a slow-motion disaster. Constipation is the precursor. Your colon’s main job is to soak up water. When waste sits there too long, the colon keeps sipping away at the moisture until that waste turns into something resembling concrete. According to the Cleveland Clinic, common culprits range from chronic opioid use—which slows the gut to a crawl—to simply ignoring the "urge to go" because you’re too busy at work.
Sometimes it’s a mechanical issue. If your pelvic floor muscles aren't firing in the right order, you're basically pushing against a closed door. This is called dyssynergic defecation. It's frustratingly common. You might also be dealing with low motility due to conditions like Parkinson's or diabetes, where the nerves in the gut just don't signal correctly anymore.
What to do impacted stool: The immediate home strategy
If you're at home and realizing that gravity and normal straining aren't doing the trick, you have to change tactics. You aren't trying to "stimulate" a bowel movement anymore; you're trying to soften or break up a physical mass.
Hydrate from the bottom up
Drinking water is great for preventing future issues, but for an active impaction, you need local intervention. This is where glycerin suppositories come in. They’re small, waxy bullets you insert. They work by drawing water into the stool and providing a slick coating. It’s a gentle first step. If that fails after about 30 minutes, people often turn to a saline enema (like a Fleet enema). These are more aggressive. They flood the rectum with fluid to create pressure and soften the mass.
👉 See also: How Much Sugar Are in Apples: What Most People Get Wrong
But be careful.
Overusing enemas can mess with your electrolytes. Also, if you have certain kidney issues or heart conditions, the sodium in those enemas can be a genuine problem. Honestly, if the first enema doesn't produce results, don't just keep doing them. That's a sign the impaction might be higher up or too dense for a simple liquid flush.
The Mineral Oil trick
Mineral oil is a "lubricant laxative." Taking it orally can help, but it takes hours. Some doctors suggest a mineral oil enema. It doesn’t force the bowel to contract like saline does; it just greases the wheels. It’s messy. It’s "kinda" gross. But it works for many people when the stool is just too dry to slide out.
Manual Disimpaction (The "Don't Try This Alone" Warning)
You’ll see "digital evacuation" mentioned in medical texts. This is exactly what it sounds like: using a lubricated, gloved finger to gently break up the stool. While some people with chronic spinal cord injuries are taught to do this safely, for the average person, you can really hurt yourself. You can tear the delicate lining of the rectum (an anal fissure) or cause a massive flare-up of hemorrhoids. Worse, you could trigger a vasovagal response, which is a sudden drop in heart rate and blood pressure that makes you faint. Not ideal when you’re alone in a bathroom.
When the DIY approach becomes a medical emergency
How do you know when you’ve crossed the line? If you start vomiting, it’s an emergency. If your stomach is hard and bloated like a drum, or if you have severe abdominal pain, go to the ER. This could mean a total bowel obstruction.
✨ Don't miss: No Alcohol 6 Weeks: The Brutally Honest Truth About What Actually Changes
Doctors have more tools. They might use a "Milk and Molasses" enema—an old-school but highly effective remedy—or stronger polyethylene glycol (PEG) solutions. In some cases, they may need to perform manual removal under sedation if the mass is too large or the patient is in too much pain.
The "Overflow" Confusion
There is a weird phenomenon called paradoxical diarrhea. This is one of the biggest "gotchas" with impacted stool. You feel totally constipated, but then you have frequent bouts of liquid, watery stool. You might think, "Oh, I have a stomach bug" and take Imodium. Do not do this. What’s actually happening is that liquid waste from higher up in the digestive tract is leaking around the hard, impacted mass. If you take anti-diarrheal medication, you are essentially locking the "gate" even tighter. If you feel impacted but have watery leakage, you should treat it as an impaction, not diarrhea.
Long-term fixes that actually work
Once you get through the immediate crisis of what to do impacted stool, you have to make sure it never happens again. Because once you’ve been impacted, your rectum can get "stretched out" (megacolon), making it harder to feel the urge to go in the future. It’s a vicious cycle.
- The Squatty Potty isn't a gimmick. Our bodies were designed to squat. Sitting at a 90-degree angle on a standard toilet actually keeps the puborectalis muscle partially choked around the rectum. Lifting your knees above your hips straightens that path. It’s basic physics.
- Magnesium is your friend. Specifically magnesium citrate or glycinate. It’s an osmotic, meaning it keeps water in the colon. Many people are chronically low in magnesium anyway.
- The "Gastrocolic Reflex" is your best tool. Your gut is most active about 20 to 30 minutes after you eat, especially after breakfast. Make it a habit to sit on the toilet at the same time every morning, even if you don't feel like you have to go. You're retraining your brain and gut to communicate.
- Fiber needs a "Water Chaser." If you increase your fiber (beans, oats, lentils) but don't double your water intake, you’re just making more "concrete." Fiber without water is a recipe for a repeat impaction.
The Nuance of Laxatives
Stimulant laxatives like Dulcolax or Senna are like a drill sergeant for your bowels. They force the muscles to cramp and push. They’re fine for occasional use, but your bowels can become "lazy" if you rely on them. They stop knowing how to move on their own. Osmotic laxatives (like Miralax) are generally considered safer for longer-term management because they just influence water movement rather than forcing muscle contractions.
Every body is different. Some people find that a simple daily kiwi fruit (with the skin!) keeps them regular because of a specific enzyme called actinidin. Others need a more clinical approach.
🔗 Read more: The Human Heart: Why We Get So Much Wrong About How It Works
Specific steps for right now
If you are currently struggling with what feels like an impaction, here is the logical progression.
First, stop eating solid, heavy foods for a few hours; stick to clear liquids to avoid adding bulk. Try a glycerin suppository first. It's the least invasive. If there is no movement after an hour, you might try a saline enema, but only if you don't have heart or kidney issues. Throughout this, do not strain until your eyes turn red. Excessive straining can cause Rectal Prolapse, where the lining of the rectum actually pushes out of the body.
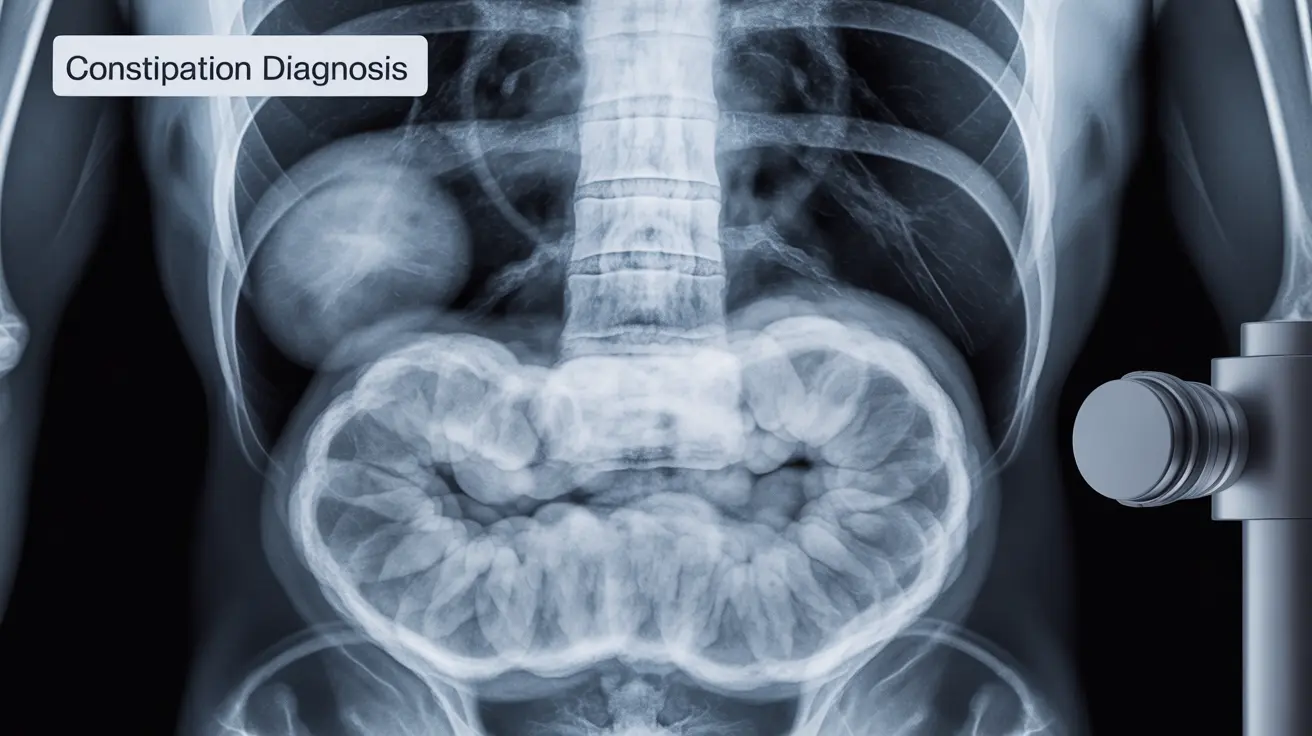
If these home steps don't work within 24 hours, or if you feel a "fullness" that won't go away despite passing some liquid, call a doctor. They can perform an abdominal X-ray or a digital exam to see exactly where the blockage is. It’s much better to have an awkward conversation with a nurse than to deal with a perforated bowel later.
Pay attention to your medications too. If you just started a new calcium supplement, an iron pill, or a blood pressure medication (like calcium channel blockers), those could be the "silent" reason your system stalled out. Sometimes, the solution isn't more laxatives; it's adjusting your existing meds with your doctor's help.
The goal isn't just to "get it out" today. It's to figure out why the "conveyor belt" stopped in the first place. Whether it's pelvic floor physical therapy, a change in diet, or managing a chronic condition, the "aftercare" of an impaction is just as important as the immediate fix. Get the blockage cleared, then start the work of keeping things moving. Use a stool softener like docusate sodium if things feel a bit dry, and never, ever ignore the urge to go when it finally returns. That urge is your body's way of saying the system is back online.