Let’s be honest. Nobody really wants to stare into the toilet bowl for too long. It’s awkward, it’s a bit gross, and we’ve mostly been conditioned to flush and forget as fast as possible. But here’s the thing: that quick glance before you hit the lever is basically a free, daily status report from your digestive system. Understanding a stool color chart adults can use as a reference isn't just for medical students or people with weird hobbies; it’s a legitimate way to track your internal health.
Your gut is a complex chemical processing plant. By the time waste makes its exit, it has been dyed, diluted, and transformed by bile, enzymes, and whatever you ate for lunch yesterday. Most of the time, a change in shade is just because you went heavy on the blueberries or took an iron supplement. Sometimes, though, the color is a literal red flag. Or a green one. Or even a pale, ghostly white one.
The Spectrum of "Normal" and Why Brown Rules
Brown is the gold standard. It’s the color we expect, and for good reason. It gets its earthy hue from a combination of bile—which starts out green or yellowish in the gallbladder—and bilirubin, a byproduct of the natural breakdown of old red blood cells. As these fluids travel through your intestines, enzymes break them down into something called stercobilin. That’s what gives poop its signature brown look.
But "brown" is a wide range. It can be tan, mahogany, or deep chocolate. Generally, if you're in that neighborhood, your liver and gallbladder are doing their jobs.
Did you know that transition time matters? If things move too fast through your colon, the bile doesn't have enough time to break down fully. This is why diarrhea is often green or bright yellow. It’s basically "raw" bile that hasn’t had its chemical makeover yet. On the flip side, if things sit in your colon for a long time—hello, constipation—the stool can become very dark brown because it has been significantly dehydrated and concentrated.
When the Stool Color Chart for Adults Turns Green
Seeing green in the bowl can be a bit of a shock. You might immediately think of an infection, but usually, it's just your diet. If you’ve been smashing kale smoothies, eating bowls of spinach, or decided that "green goddess" dressing is its own food group, expect a tint. Chlorophyll is a powerful pigment.
🔗 Read more: In the Veins of the Drowning: The Dark Reality of Saltwater vs Freshwater
Even purple foods like blueberries or black liquorice can sometimes come out looking greenish-black due to the way they interact with stomach acid.
Then there’s the "fast transit" issue. If you’re experiencing a bout of the runs, the bile doesn't have the window of time it needs to turn brown. It stays green. If you feel fine otherwise, it’s probably just those tacos from last night moving through you at record speed. However, if the green stool is accompanied by cramping and fever, you might be looking at a guest appearance by Salmonella or Giardia. According to the Mayo Clinic, these pathogens irritate the lining of the gut, forcing everything out before the color change can occur.
The Warning Signs: Red, Black, and Pale
This is where we need to pay attention. While many shifts in the stool color chart adults see are harmless, these three categories—red, black, and pale—require a bit more detective work.
Bright Red (Hematochezia)
Seeing red is terrifying. Before you panic, think: did I eat beets? Seriously. Beets can cause a condition called beeturia, which turns both urine and stool a startling shade of pink or red. Red food coloring, cranberries, and tomato soup can also play tricks on your eyes.
If it isn't food, bright red blood usually suggests the "end of the line." We’re talking about the lower gastrointestinal tract. This often means hemorrhoids or small tears called anal fissures. While uncomfortable, they aren't usually life-threatening. However, red blood can also be a sign of diverticulitis or, more seriously, colon cancer. If the blood is mixed into the stool rather than just on the surface, that’s a signal to call a doctor.
💡 You might also like: Whooping Cough Symptoms: Why It’s Way More Than Just a Bad Cold
Black and Tarry (Melena)
Black stool is a different beast entirely. If you’re taking iron supplements, Pepto-Bismol (bismuth subsalicylate), or eating a lot of Oreos, your stool can turn a deep, ink-black. That’s normal.
But if the stool is black, sticky, and smells incredibly foul—like nothing you’ve ever smelled before—it’s often melena. This is old, "digested" blood. It usually comes from the stomach or esophagus, perhaps from an ulcer. The blood gets oxidized by stomach acid, turning it from red to black. It’s a classic sign of an upper GI bleed and isn't something to ignore.
Pale, White, or Clay-Colored (Acholic)
This is perhaps the most overlooked color. If your stool looks like putty or light-colored clay, you have a "lack of bile" problem. Bile is what provides the pigment. If the bile duct is blocked—perhaps by a gallstone or a tumor in the pancreas—the bile can't reach the intestines.
This often goes hand-in-hand with jaundice (yellowing of the skin or eyes) and dark urine. When bile can't get out through the gut, it backs up into the bloodstream and exits through the kidneys instead. If you see clay-colored stools, you don't wait a week to see if it clears up. You go in.
Yellow and Greasy: The Malabsorption Factor
Yellow stool is fairly common, but it’s the texture that matters here. If it’s yellow, greasy, and has a film that looks like oil on top of the toilet water, you’re looking at steatorrhea. Essentially, your body isn't absorbing fat.
📖 Related: Why Do Women Fake Orgasms? The Uncomfortable Truth Most People Ignore
This happens often in people with Celiac disease. When someone with Celiac eats gluten, their immune system attacks the lining of the small intestine, flattening the villi that are supposed to soak up nutrients. No absorption means the fat stays in the stool. It can also point toward chronic pancreatitis or cystic fibrosis, where the body doesn't produce enough enzymes to break down lipids.
Real World Factors: Medications and Extras
We often forget that what we swallow for health can change what we see in the bathroom.
- Antibiotics: These are like a nuclear bomb for your gut microbiome. By killing off the "good" bacteria that help process pigments, your stool color can fluctuate wildly.
- Antacids: Some can turn stool a lighter shade.
- Iron Supplements: As mentioned, these are the primary cause of harmless black stool.
- Vitamins: High doses of vitamin A can sometimes lead to an orange tint.
Interestingly, it isn't just color. Mucus in the stool is another common concern. A little bit is normal—the intestines are lined with it to keep things moving. But if you see globs of white or yellowish mucus, it could be a sign of inflammation, like Crohn’s disease or Ulcerative Colitis. Your body is overproducing "lube" because the walls of the gut are irritated.
Summary of the Stool Color Chart for Adults
| Color | Likely Cause | Action Level |
|---|---|---|
| Brown | Normal bile breakdown. | Keep doing what you're doing. |
| Green | Leafy greens, food dye, or fast transit. | Usually fine; check for diarrhea. |
| Yellow (Greasy) | Malabsorption of fat (Celiac, etc.). | Mention to a doctor if it persists. |
| Bright Red | Beets, food dye, or lower GI bleeding. | Investigate; see a doctor if persistent. |
| Black (Tarry) | Iron, Pepto-Bismol, or upper GI bleed. | Emergency if sticky and foul-smelling. |
| Pale/White | Bile duct obstruction or liver issues. | See a doctor immediately. |
| Orange | Carrots, sweet potatoes, or certain meds. | Generally harmless. |
Moving Beyond the Color
While the stool color chart adults rely on is a great tool, it’s only one piece of the puzzle. The Bristol Stool Scale is another clinical tool that looks at shape. Ideally, you want a "Type 3" or "Type 4"—a smooth, sausage-like shape. If the color is brown but it looks like small hard pebbles, you're dehydrated. If it’s brown but liquid, you’ve got a different issue.
Don't ignore the context. One weird-colored bowel movement is rarely a crisis. It's usually the pizza you had at 1 AM. It’s the pattern that matters. If your stool has changed color and stayed that way for more than a few days, or if the color change is paired with unexplained weight loss, intense pain, or a fever, that is your body's way of shouting for help.
Actionable Steps for Better Gut Health Monitoring
Checking your stool shouldn't be a source of anxiety. It’s just data. To get the most accurate "read" on your internal health, try these steps:
- Hydrate Consistently: Dehydration changes the concentration of pigments in your stool, making it harder to tell what's "normal" for you. Drink enough water so your urine is pale yellow; this keeps the transit time in your gut consistent.
- Track Your "Food to Flush" Time: If you eat something very distinct, like corn or beets, note how long it takes to show up. A healthy transit time is usually between 24 and 72 hours. If it’s appearing in 6 hours or taking 4 days, the color will be affected regardless of your organ health.
- Perform a "Dietary Audit" First: Before calling a specialist about red or black stool, look back at your last 48 hours of intake. Did you have a smoothie with activated charcoal? Did you eat a whole bag of Flamin' Hot Cheetos? Most "scary" colors are found in the pantry, not the pathology lab.
- Listen to the "Ache": Color alone is rarely the only symptom of a serious GI issue. If you see a color change and feel a dull ache in your upper right abdomen (where your liver/gallbladder live), that's a much stronger signal than color alone.
- Use a Journal if Chronic: If you have IBS or other digestive issues, keep a quick log on your phone. Note the color and any accompanying symptoms like bloating or gas. This is incredibly helpful for doctors to see patterns that you might miss.
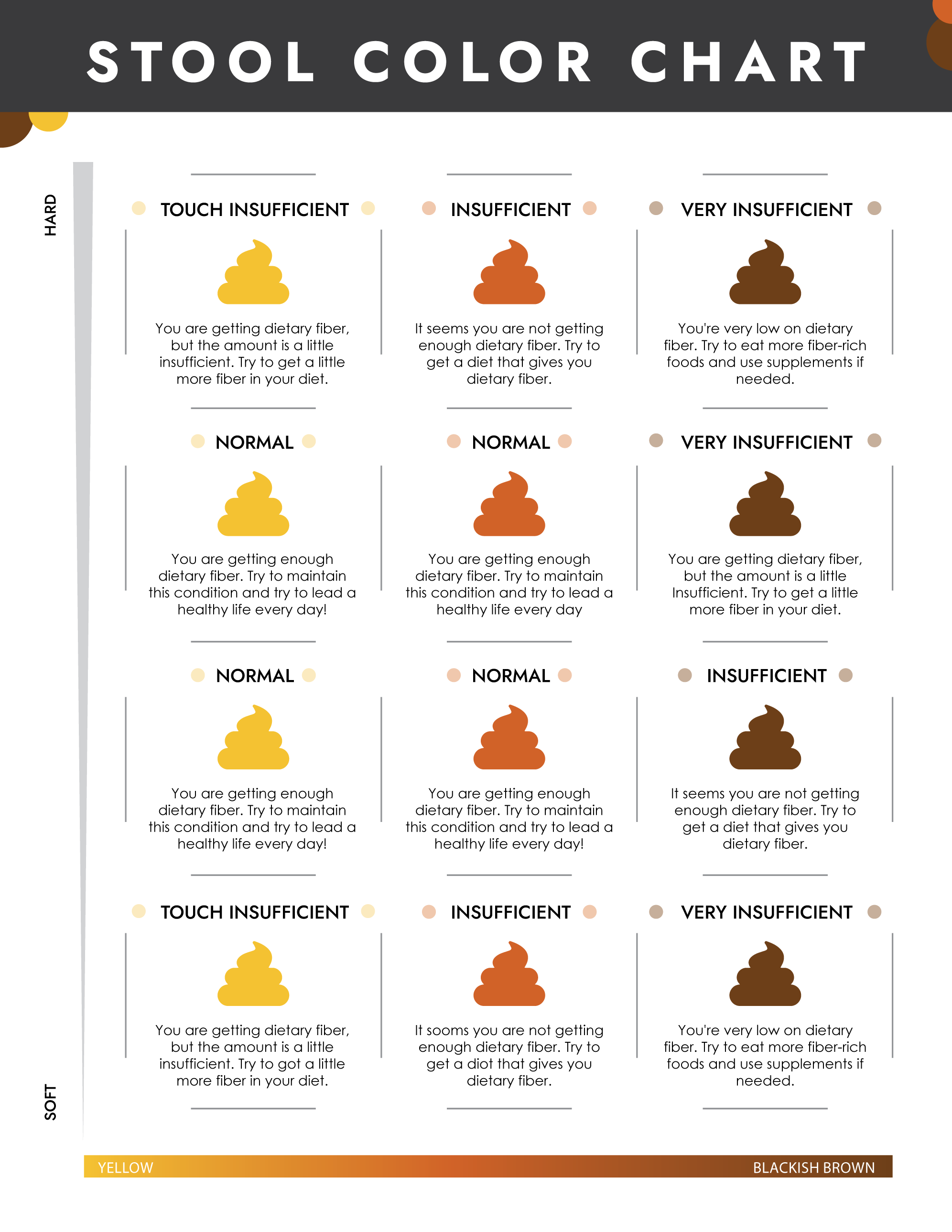
Focusing on fiber intake—roughly 25 to 35 grams a day—will help keep your stool "textbook" brown by ensuring a steady, healthy transit through the colon. This gives the natural chemical processes enough time to work their magic, turning that bile into the brown hue we like to see.