You’re staring at a grainy, pinkish-red image on a screen or a printout from your gastroenterologist. It looks like a tiny mushroom or maybe a small, rounded pebble clinging to the wall of your stomach. Finding polyps in stomach pictures after an endoscopy can feel terrifying. Your mind immediately goes to the "C" word. Honestly, though? Most of the time, these little bumps are just accidental discoveries that don’t actually do much of anything.
But "most of the time" isn't "all the time."
The reality of gastric polyps is nuanced. You might have one. You might have fifty. Some are caused by the very medication you take to stop heartburn, while others are a red flag for genetic syndromes that require lifelong monitoring. Understanding what you’re looking at requires a mix of medical literacy and a bit of a reality check regarding how doctors actually diagnose what’s going on inside you.
What Are You Actually Seeing in Polyps in Stomach Pictures?
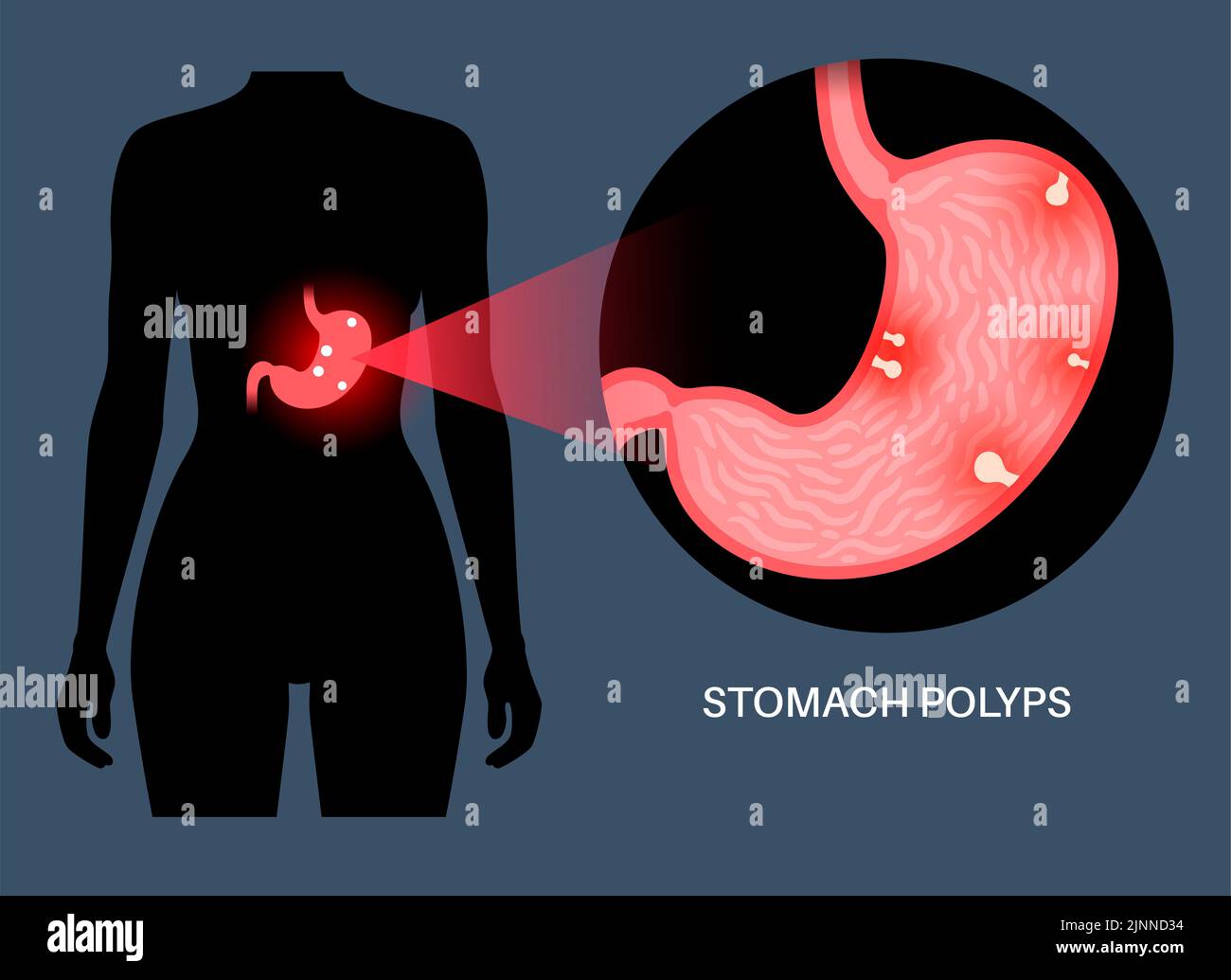
When a doctor slides an endoscope down your esophagus, they’re looking for irregularities in the mucosa—the lining of your stomach. In polyps in stomach pictures, these appear as protrusions. They can be sessile (flat and broad-based) or pedunculated (on a stalk, like a cherry).
The visual appearance alone is rarely enough for a definitive diagnosis. Dr. Michael Rice from the University of Michigan Health often notes that while certain features—like the color, size, or surface pattern—give us clues, the gold standard is always the pathology report. You can’t just look at a photo and know for sure if a polyp is benign or precancerous.
👉 See also: Why Your Best Kefir Fruit Smoothie Recipe Probably Needs More Fat
The Most Common Types You’ll Encounter
- Fundic Gland Polyps: These are the "common cold" of stomach polyps. If you’ve been on Proton Pump Inhibitors (PPIs) like Prilosec or Nexium for years, there is a high chance you have these. They look like small, smooth, glassy domes. They are almost always harmless.
- Hyperplastic Polyps: These usually pop up because of chronic inflammation. Think of them like scar tissue or a callus. If you have H. pylori (a common bacterial infection), your stomach might sprout these as a reaction. Once the infection is cleared, they often just vanish.
- Adenomatous Polyps (Adenomas): These are the ones that demand attention. They are true precursors to cancer. They often look different in polyps in stomach pictures—maybe a bit more rugged or "villous"—but again, the microscope makes the final call.
The PPI Paradox: Why Your Heartburn Meds Might Be the Cause
It’s a bit ironic. You take a pill to feel better, and that pill causes a growth in your stomach. Fundic gland polyps (FGPs) have become incredibly common because of the widespread use of PPIs. When you suppress stomach acid, your body tries to compensate by producing more gastrin, a hormone that can cause the glands in your stomach to stretch and form tiny cysts.
Basically, the "pictures" you see of these polyps are often just a side effect of modern pharmacology. Most GI specialists won't even remove them unless they’re unusually large—usually over 1 centimeter. If they’re small and you’re on a PPI, your doctor might just shrug them off as a known trade-off for managed reflux.
When the Visuals Become Concerning
Size matters. If a polyp is bigger than 10mm, the risk profile changes. In polyps in stomach pictures, a large polyp might look imposing, but the real danger lies in its cellular architecture.
- Bleeding: Large polyps can ulcerate. You might not feel it, but you’ll see the evidence in a blood test showing anemia.
- Obstruction: In rare cases, a polyp near the "exit" of the stomach (the pylorus) can act like a literal cork, stopping food from moving into the small intestine.
- Dysplasia: This is the fancy medical word for "cells starting to look weird." This is the bridge between a harmless bump and cancer.
Consider the case of Familial Adenomatous Polyposis (FAP). This is a genetic condition where people develop hundreds or thousands of polyps throughout their digestive tract. In these patients, the polyps in stomach pictures look like a cobblestone street. It’s a completely different clinical scenario than a 55-year-old with one random bump found during a routine check for indigestion.
✨ Don't miss: Exercises to Get Big Boobs: What Actually Works and the Anatomy Most People Ignore
The Role of H. Pylori and Chronic Gastritis
We can’t talk about stomach polyps without talking about Helicobacter pylori. This bacteria is a master of survival in the acidic environment of the stomach. It causes chronic inflammation, and that inflammation is the breeding ground for hyperplastic polyps.
If your doctor finds hyperplastic polyps, the first thing they should do is test you for H. pylori. It’s a simple breath or stool test. If it’s positive, a round of antibiotics can often resolve the issue. It’s one of the few times in medicine where treating an infection can literally make "tumors" (even benign ones) disappear.
Beyond the Photo: The Biopsy Process
The photo is just the map; the biopsy is the destination. During the endoscopy, the doctor uses a small wire loop or forceps passed through the scope to snip off the polyp or take a sample.
- Cold Snare: For smaller polyps, they just "grab and go."
- EMR (Endoscopic Mucosal Resection): For larger, flatter polyps that look suspicious, they might inject fluid under the polyp to lift it away from the muscle layer before cutting it out. This keeps the procedure safe and prevents perforation.
You’ll get the "pictures" immediately after you wake up from sedation, but the "answers" take 3 to 5 business days. Waiting for that pathology report is the hardest part.
🔗 Read more: Products With Red 40: What Most People Get Wrong
Why You Shouldn't Google Your Endoscopy Photos
Seriously. Don't.
Searching for polyps in stomach pictures online will inevitably lead you to the most extreme, worst-case scenarios. Medical databases show images of advanced carcinomas and rare syndromes because those are "interesting" to students. Your single, 4mm fundic gland polyp is boring to a textbook, but it’s the most likely reality for you.
Furthermore, the lighting in an endoscopy can be deceptive. A little bit of bile or a trick of the camera’s flash can make a benign spot look angry and red. Trust the person who spent 10 years in school to interpret the live feed, not a search engine's image results.
Actionable Next Steps After Seeing Your Results
If you’ve just seen your endoscopy report and you’re looking at polyps in stomach pictures, here is exactly what you should do:
- Check the Pathology: Ask specifically, "Was this a fundic gland polyp, a hyperplastic polyp, or an adenoma?" This determines your entire future care plan.
- H. Pylori Status: If you haven't been tested for the bacteria, insist on it. It is the most treatable cause of many gastric issues.
- Review Your Meds: If you have FGPs and you've been on a PPI for years, talk to your doctor about whether you can taper down to a H2 blocker (like Pepcid) or use the PPI only "as needed."
- Schedule the Follow-Up: If it was an adenoma, you will likely need another endoscopy in 6 to 12 months. If it was a small fundic gland polyp, you might never need to think about it again.
- Family History: If you have multiple polyps, mention any family history of colon cancer or stomach cancer. Some stomach polyps are linked to syndromes that affect the colon too.
The most important thing to remember is that the "picture" is a moment in time. Most stomach polyps are discovered incidentally—meaning they weren't even the cause of the symptoms that sent you to the doctor in the first place. They are markers of your stomach's environment, not necessarily a death sentence. Stay focused on the pathology report, keep your H. pylori in check, and use those pictures as a tool for discussion with your specialist rather than a source of late-night anxiety.