When you first start Googling stevens johnson syndrome photos, you're probably scared. Honestly, you should be a little concerned if you're seeing a rash that doesn't look like anything you've ever had before. It’s not just a "bad reaction." Stevens-Johnson Syndrome (SJS) is a medical emergency that basically involves your skin deciding to quit its job.
It starts like the flu. You feel crappy, your bones ache, and maybe your eyes feel a bit gritty. Then the rash hits. It’s not just a red patch; it’s a blistering, peeling nightmare that can cover your entire body. If it covers more than 30% of your body, doctors call it Toxic Epidermal Necrolysis (TEN). It's the same disease, just a different scale of chaos.
Why Searching for Stevens Johnson Syndrome Photos Is So Complicated
The problem with looking at pictures online is that SJS is a shapeshifter. In the early stages, it might look like a drug eruption or even a weird case of hives. But there’s a specific look to it—doctors call them "targetoid" lesions. They look like little bulls-eyes. If you see those, stop reading this and go to the ER. Seriously.
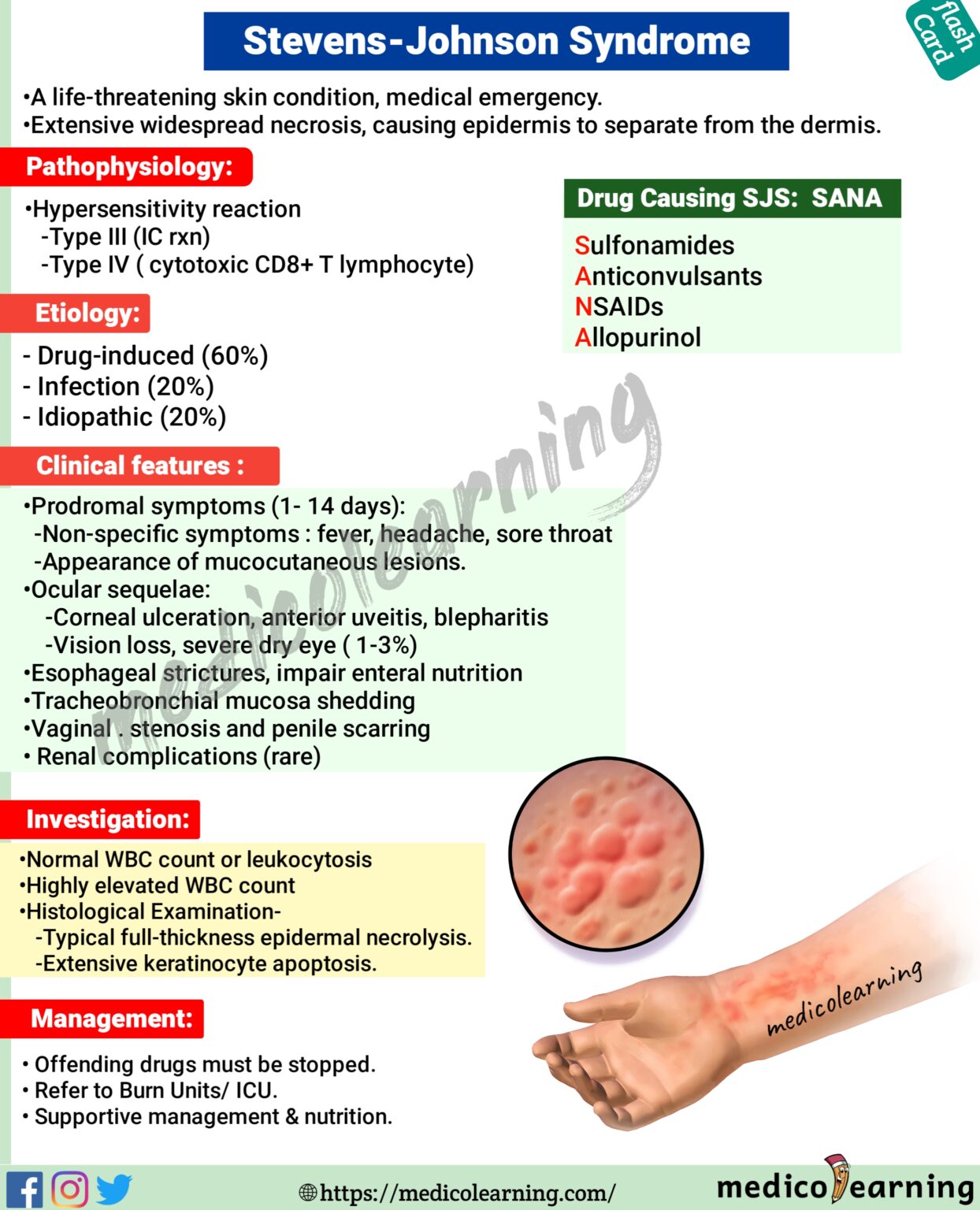
Most people think SJS is rare. It is. But for the person lying in a burn unit because their skin is sloughing off in sheets, "rare" doesn't mean much. Usually, this happens because of a medication. It could be something common like Ibuprofen (Motrin/Advil) or something specific like Allopurinol for gout. Your immune system basically has a catastrophic meltdown and starts attacking your own skin cells (keratinocytes).
The Phases of the SJS Rash
You won't see the full horror in the first hour. It’s a progression.
👉 See also: Why the Ginger and Lemon Shot Actually Works (And Why It Might Not)
- The Prodrome: This is the "fake out" phase. You have a fever. Your throat hurts. You might think you have COVID or a nasty cold.
- The Initial Breakout: This is where the stevens johnson syndrome photos start to match what’s on your body. You get these dusky, flat, red or purple spots. They usually start on the trunk (your chest and back) and spread to the limbs and face.
- The Mucosal Attack: This is a big one. SJS loves "wet" skin. Your mouth, your eyes, and your genitals. If you have a rash AND your lips are starting to crust or your eyes are turning beet red and oozing, that is a massive red flag.
- Denudation: This is the medical term for the skin falling off. It’s as painful as it sounds.
Nikolsky’s Sign: A Crucial Detail
There is a thing called Nikolsky’s sign. If you take your finger and apply slight pressure to a red area and the skin just... slides off... that’s a positive Nikolsky sign. You won't always see this in every photo, but it is a hallmark of the condition. It means the bond between your top layer of skin (epidermis) and the bottom layer (dermis) has dissolved.
Real Stories and Drugs That Trigger It
Let’s talk about the culprits. We know from data published by the Stevens-Johnson Syndrome Foundation and researchers at the Mayo Clinic that certain drugs are high-risk.
- Anticonvulsants: Carbamazepine and Lamotrigine are famous for this.
- Sulfonamides: "Sulfa" drugs like Bactrim.
- NSAIDs: Even the stuff you buy at CVS can do it in rare cases.
- Nevirapine: Used for HIV.
I remember a case involving a young woman who was prescribed Lamotrigine for mood stabilization. She was told to watch for a rash. She saw a few spots on her chest—they looked like bug bites. Within 48 hours, she was in a medically induced coma because her airway was blistering. This isn't to scare you for no reason; it's to highlight that SJS moves fast.
The Difference Between SJS and Other Rashes
If you’re looking at stevens johnson syndrome photos and comparing them to your own skin, you might be confused by Erythema Multiforme (EM). EM is often caused by the Herpes Simplex Virus. It looks similar—lots of target lesions—but it’s usually much less severe and doesn't involve the massive skin peeling that SJS does.
✨ Don't miss: How to Eat Chia Seeds Water: What Most People Get Wrong
Then there’s DRESS syndrome (Drug Reaction with Eosinophilia and Systemic Symptoms). DRESS gives you a fever and a rash, but it also messes with your internal organs like your liver. You won't usually see the "peeling" in DRESS like you do in SJS.
[Image comparing Erythema Multiforme, SJS, and DRESS syndrome]
What Happens in the Hospital?
If you go to the hospital with suspected SJS, they won't just give you a cream and send you home. You’re going to the ICU or a Burn Unit. Why a burn unit? Because losing your skin to SJS is functionally the same as being burned. Your skin is your barrier. Without it, you lose fluids and you get massive infections.
Doctors like Dr. Elizabeth Phillips at Vanderbilt University have done incredible work on the genetic markers for SJS. Some people have a specific gene—HLA-B*1502—that makes them much more likely to react to certain drugs. This is why some populations, particularly those of Asian descent, are often screened before starting high-risk meds.
🔗 Read more: Why the 45 degree angle bench is the missing link for your upper chest
Treatment Reality
- They stop the offending drug immediately.
- IV fluids—lots of them.
- Pain management (usually morphine or similar).
- Wound care using specialized dressings like Biobrane or silver-impregnated bandages.
- Sometimes Cyclosporine or IVIG (Intravenous Immunoglobulin) to try and stop the immune system from killing more skin.
Long-term Complications Nobody Warns You About
Surviving SJS is the first step, but the "after" is its own battle. Many photos of survivors show scarring, but the eyes are the biggest issue. Chronic dry eye, light sensitivity, and even blindness are common. The eyelashes can grow inward and scratch the cornea.
Your skin might come back a different color (hyperpigmentation or hypopigmentation). It might be thinner. You might lose your fingernails or toenails. It's a long road.
How to Protect Yourself
If you’re starting a new medication and you notice a fever followed by a painful, spreading rash, don't wait. Don't take an antihistamine and go to sleep.
Actionable Next Steps
- Check your meds. Look at any new prescriptions from the last 2 to 8 weeks. That's the typical window for SJS to appear.
- Examine your mouth. Use a flashlight. Are there sores on your tongue or the inside of your cheeks? Are your lips bleeding or crusty?
- Document the spread. Take your own photos every few hours. If the rash is moving and changing rapidly, show these to the emergency doctor. It helps them see the velocity of the reaction.
- Seek a Specialist. If you survive SJS, you need to see a dermatologist and an ophthalmologist (eye doctor) regularly. You also need to wear a medical alert bracelet. Taking that same drug again could be fatal.
If you or someone you know is going through this, the SJS Foundation provides resources for families. It’s a lonely, terrifying disease because so few people understand it. But knowing what those early target lesions look like can quite literally save a life.
Stop scrolling through the worst-case scenario images and look at your own skin objectively. If it's blistering, if it's painful rather than itchy, and if you have a fever, get to the hospital now.