You're standing at the pharmacy counter. You glance at the white paper bag and see a different name than last month. Maybe you were on 40mg of Simvastatin, but now the doctor switched you to 10mg of Rosuvastatin. Your brain immediately does the math. Ten is less than forty. You feel like you’re getting ripped off, or maybe your cholesterol is suddenly "cured" and you need less medicine. Honestly? That's not how it works at all. Statin dose equivalence is a weird, non-linear world where a smaller number often packs a much bigger punch.
It's confusing.
Most people think of drugs like Tylenol—if you take 500mg, it’s half as strong as 1000mg. Simple. But statins are specialized tools. Comparing them is less like comparing weights and more like comparing the heat of different chili peppers. A tiny Habanero is way hotter than a giant Bell Pepper. In the world of HMG-CoA reductase inhibitors (the nerdy name for statins), Rosuvastatin is your Habanero.
What exactly is statin dose equivalence?
When doctors talk about equivalence, they are looking at one specific metric: how much does this pill lower your LDL cholesterol? That’s the "bad" stuff. We don't care about the physical weight of the powder in the capsule. We care about the result in your bloodstream.
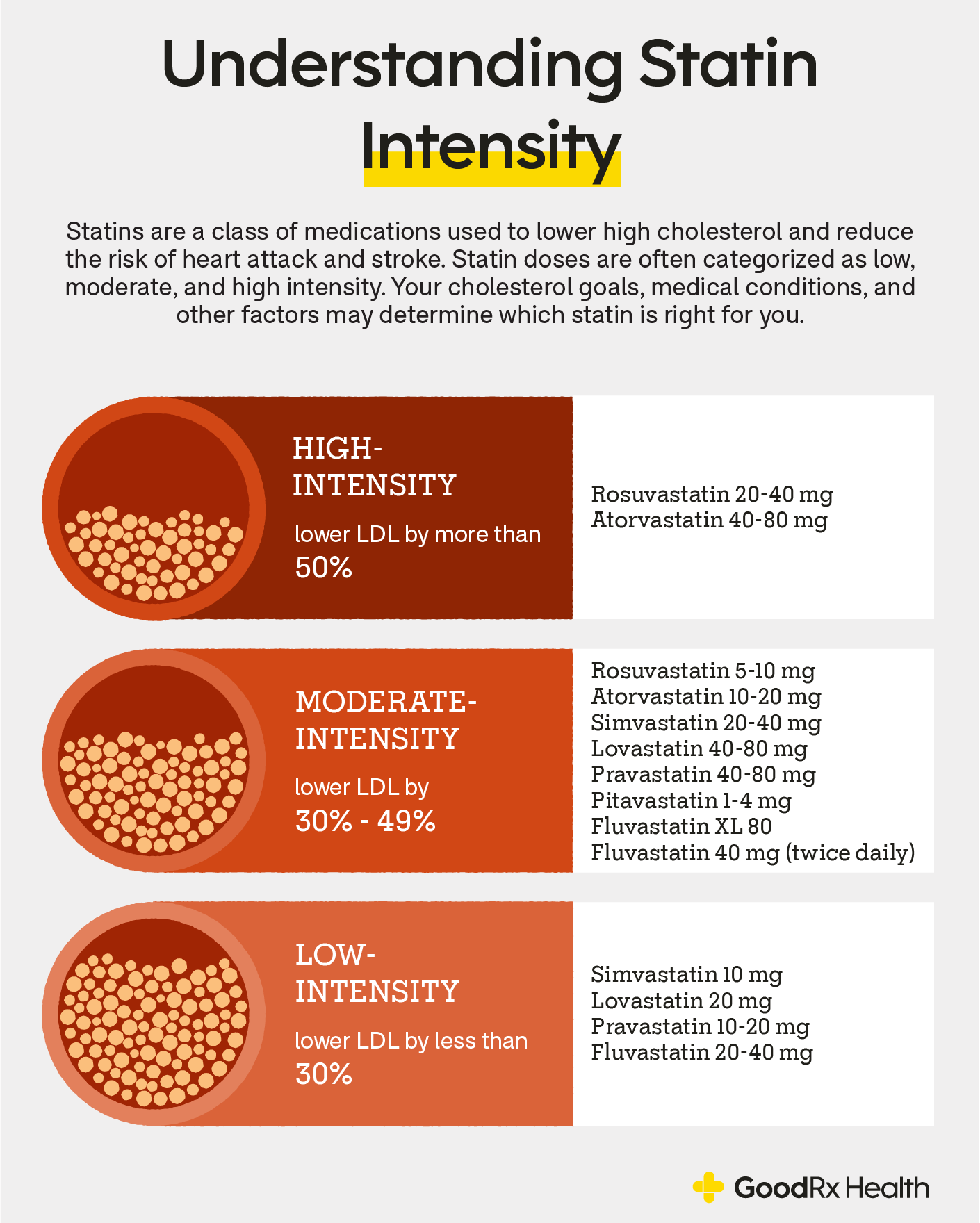
The medical community generally splits these drugs into three buckets: high-intensity, moderate-intensity, and low-intensity. A "high-intensity" dose is expected to drop your LDL by 50% or more. To get that 50% drop, you might only need 20mg of one drug, but you’d need 80mg of another. Some drugs can’t even hit that 50% mark no matter how much you take because they aren't "strong" enough.
Take Atorvastatin (Lipitor). It’s the workhorse of the industry. To get a high-intensity effect, you need 40mg to 80mg. If you’re on Rosuvastatin (Crestor), you only need 20mg to 40mg to reach that same "high-intensity" tier.
Why the numbers don't match up
It comes down to pharmacokinetics. Basically, how your body absorbs, uses, and gets rid of the drug.
Some statins are lipophilic (fat-soluble), and others are hydrophilic (water-soluble). This isn't just a chemistry trivia fact; it changes everything. Simvastatin and Atorvastatin love fat. They can slip into cell membranes easily. Rosuvastatin and Pravastatin prefer water. Because Rosuvastatin is water-soluble and has a very high "uptake" into the liver—where cholesterol is actually made—it can do more work with a smaller physical dose. It’s efficient.
📖 Related: Products With Red 40: What Most People Get Wrong
Lowering LDL isn't a 1:1 ratio. If you double the dose of any statin, you don't double the results. There is something called the "Rule of Six."
Every time you double a statin dose, you usually only get about a 6% further reduction in LDL.
Think about that. If 10mg of a drug gets you a 30% drop, 20mg gets you 36%, and 40mg gets you 42%. You’re taking four times as much medicine for only a 12% gain. This is why switching to a different, more potent molecule (like moving from Simvastatin to Atorvastatin) is often smarter than just cranking up the dose of a weaker one. It minimizes the stuff circulating in your blood that isn't doing work but might be causing those annoying muscle aches.
The chart your doctor is probably looking at
When a cardiologist decides to swap your meds, they aren't guessing. They use guidelines from the American College of Cardiology (ACC) and the American Heart Association (AHA). They have these "intensity" tiers burned into their brains.
High-Intensity Statins (The Heavy Hitters)
These lower LDL by roughly 50% or more. You're looking at:
- Atorvastatin: 40mg to 80mg
- Rosuvastatin: 20mg to 40mg
Moderate-Intensity Statins (The Middle Ground)
These aim for a 30% to 49% reduction. This is where most people live.
- Atorvastatin: 10mg to 20mg
- Rosuvastatin: 5mg to 10mg
- Simvastatin: 20mg to 40mg
- Pravastatin: 40mg to 80mg
- Lovastatin: 40mg to 80mg
- Pitavastatin: 2mg to 4mg
Low-Intensity Statins (The Gentle Touch)
These drop LDL by less than 30%. They are rarely used as first-line therapy these days unless someone is very sensitive to side effects.
👉 See also: Why Sometimes You Just Need a Hug: The Real Science of Physical Touch
- Simvastatin: 10mg
- Pravastatin: 10mg to 20mg
- Lovastatin: 20mg
Is 80mg of Simvastatin still a thing?
Short answer: No. Not really.
Back in the day, doctors used to prescribe 80mg of Simvastatin all the time to get patients into that "high-intensity" zone. Then the FDA stepped in around 2011 with a pretty stern safety communication. They found that the 80mg dose of Simvastatin was linked to a much higher risk of myopathy—that's the medical word for muscle damage. Specifically, it could lead to rhabdomyolysis, which is a scary condition where muscle tissue breaks down and clogs up your kidneys.
Nowadays, if you need that level of LDL lowering, your doctor will just move you to 20mg of Rosuvastatin. It’s safer and more effective. If you are still on 80mg of Simvastatin, you should probably have a chat with your GP about modernizing your script.
Why would you even switch?
Cost used to be the biggest reason. Years ago, Crestor (Rosuvastatin) was expensive and brand-name only. Simvastatin was cheap. So, people stayed on higher doses of the cheap stuff. Today, almost all of these are generic and affordable.
The real reason to switch now is side effects or "drug-drug interactions."
Some statins are processed by a specific enzyme in your liver called CYP3A4. A lot of other drugs—like certain blood pressure meds or even grapefruit juice—use that same pathway. If you're taking a statin that uses that pathway and you add another drug that competes for it, the levels of the statin in your blood can skyrocket. That's when you get the side effects.
Pravastatin and Rosuvastatin don’t really use that CYP3A4 pathway. So, if you’re a "poly-pharmacy" patient (someone taking five or more pills a day), your doctor might switch you to a 10mg or 20mg dose of Rosuvastatin even if your cholesterol was fine on your old med, just to avoid a chemical traffic jam in your liver.
✨ Don't miss: Can I overdose on vitamin d? The reality of supplement toxicity
Real-world efficacy: It’s not just about the LDL
We focus on the LDL numbers because they're easy to track on a blood test. But statins have "pleiotropic" effects. This is a fancy way of saying they do cool stuff we didn't originally intend for them to do. They stabilize the plaque in your arteries.
Imagine your artery is a pipe and there's a bump of "gunk" (plaque) on the inside. If that gunk is soft and squishy, it can pop. That's a heart attack. Statins sort of "calcify" or toughen up that plaque so it’s less likely to rupture.
Does dose equivalence matter for plaque stability? Yes. The higher-intensity doses—even if the LDL drop is similar—seem to provide better "fireproofing" for your arteries. This is why after someone has a heart attack, they are almost always put on a high-intensity dose (like 80mg Atorvastatin) regardless of what their cholesterol levels were to begin with. We aren't just chasing a number; we're trying to stop the next "pop."
Navigating the "muscle pain" dilemma
The biggest hurdle with statin dosing is the "nocebo" effect. You’ve heard statins cause muscle pain. You take the pill. Your leg hurts. You stop the pill.
However, big trials like the SAMSON trial showed that a huge percentage of people who reported muscle pain while on statins also reported muscle pain while taking a placebo (a sugar pill).
That said, the pain is real to the person feeling it. If you're on a high-dose moderate-intensity statin (like 80mg of Pravastatin) and your legs ache, the move isn't usually to quit. The move is to look at the statin dose equivalence chart and find a more potent molecule that requires a lower physical mass. Moving to 5mg or 10mg of Rosuvastatin might give you the same heart protection with a much lower concentration of drug in your systemic circulation.
Steps you can take right now
Don't just stare at the bottle and wonder. If you’ve been moved from a "large" dose of a 1st-generation statin to a "small" dose of a 3rd-generation one, you haven't been downgraded.
- Check your intensity tier. Look at your current prescription. Match it against the categories above. Are you on high, moderate, or low intensity? If you have known heart disease and you're on "low," ask why.
- Review your "Rule of Six." If your LDL isn't where it needs to be, don't just assume you need to double your current dose. Ask your doctor if a "potency switch" (changing the drug) is better than a "dose hike."
- Time it right. Some statins with short half-lives (like Simvastatin, Lovastatin, and Pravastatin) work way better if you take them at night. Why? Because your liver makes most of its cholesterol while you sleep. However, the heavy hitters like Atorvastatin and Rosuvastatin stay in your system so long it doesn't really matter when you take them.
- Bloodwork is king. Equivalence charts are averages. Your genetics might make you a "hyper-responder" to one drug and a "non-responder" to another. Always re-test your lipids 6 to 8 weeks after any dose or drug change.
The goal isn't to take the most medicine. It's to take the most effective medicine at the lowest dose necessary to keep your arteries clear. Understanding that 10mg can be stronger than 40mg is the first step in actually managing your heart health instead of just swallowing a pill because you were told to.