Drink more water. It’s the advice we hear for everything from clear skin to weight loss, and usually, it’s solid. But when you’re staring at a lab report that says your GFR is between 30 and 59, that "common sense" advice starts to feel a little shaky. Honestly, stage 3 kidney disease water intake is one of the most misunderstood parts of renal care because the "right" amount isn't a fixed number. It’s a moving target.
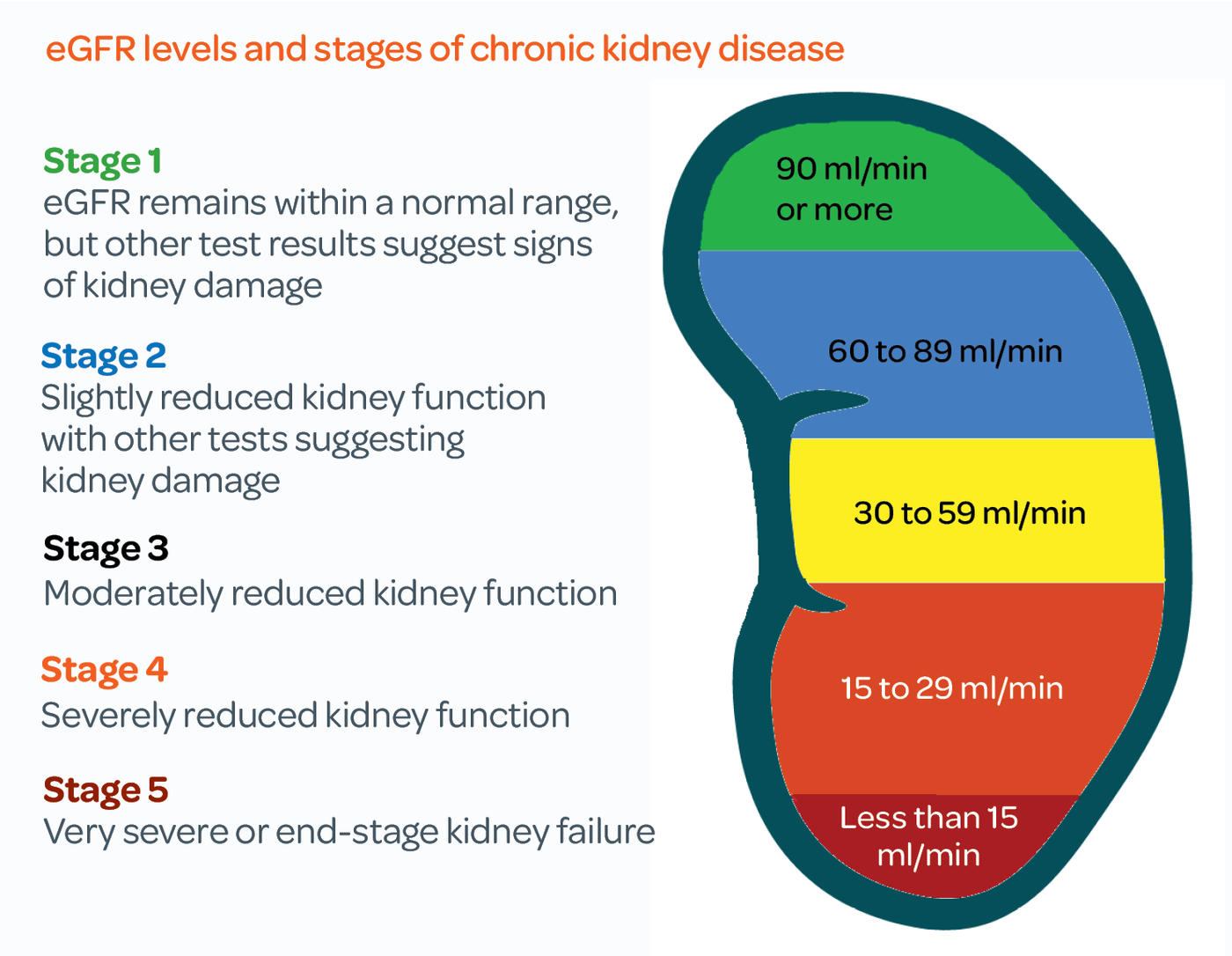
Your kidneys are basically the world’s most sophisticated filtration system. By Stage 3, they aren't failing completely, but they’re definitely tired. They’re working at about 30% to 60% capacity. This means they can still process fluid, but they’ve lost their "buffer" for extremes. If you drink too little, you risk dehydration and a further drop in kidney function. If you drink too much, you might actually overwhelm the filters, leading to swelling or high blood pressure.
The myth of the gallon jug
You’ve probably seen those massive water bottles with time markers on the side. For someone with healthy kidneys, those are a harmless trend. For you? They could be a problem.
The National Kidney Foundation generally notes that for most Stage 3 patients, fluid restriction isn't necessary yet. That sounds like a relief, right? But "no restriction" doesn't mean "unlimited." Most nephrologists, like those at the Mayo Clinic, suggest that unless you’re seeing significant swelling (edema), you should aim for about 1.5 to 2 liters a day. That’s roughly 6 to 8 cups.
Wait.
That’s the "normal" advice. So why is Stage 3 different? It’s different because your margin for error has shrunk. If you spend a day hiking in 90-degree heat, a person with healthy kidneys can bounce back from dehydration quickly. At Stage 3, a single episode of acute dehydration can cause a permanent "step down" in your GFR. You might go from a 45 to a 38 and never quite get that number back up.
✨ Don't miss: The Truth Behind RFK Autism Destroys Families Claims and the Science of Neurodiversity
Why thirst isn't always your friend
In a perfect world, we’d just drink when we’re thirsty. But chronic kidney disease (CKD) messes with the body's signaling. Some people with Stage 3 find they aren't thirsty even when they’re getting dry. Others feel a constant, nagging thirst because their blood sugar is slightly elevated or because of medications like ACE inhibitors.
Dr. Joel Topf, a nephrologist often known on social media as the "Kidney Boy," frequently discusses how the body manages salt and water. He points out that water follows salt. If your Stage 3 diet is still high in sodium, you’re going to hold onto every drop of water you drink. This isn't "hydration." This is fluid overload. It puts pressure on your heart. It makes your blood pressure spike, which—you guessed it—damages the tiny capillaries in your kidneys even more.
How to tell if your stage 3 kidney disease water intake is actually on track
Forget the apps for a second. Look at your body.
If you wake up and your eyelids look puffy, or if your socks leave deep indentations in your ankles by 4:00 PM, you’re likely overdoing the fluids (or the salt). On the flip side, if your urine looks like apple juice or you’re feeling dizzy when you stand up, you’re running too dry.
The goal is "straw-colored" urine. Not clear. Clear urine often means you’re flushing out electrolytes that your kidneys are already struggling to balance.
🔗 Read more: Medicine Ball Set With Rack: What Your Home Gym Is Actually Missing
The "Hidden" fluids you're forgetting
Water isn't just what’s in your glass. About 20% of our fluid intake comes from food. This is where Stage 3 patients get tripped up.
- Watermelon and cucumbers are basically solid water.
- Soups and stews.
- Jell-O and popsicles.
- Even that morning bowl of oatmeal.
If you’re eating a diet rich in fruits and veggies (which is often recommended for CKD to keep your acidity levels down), you might need to drink slightly less plain water than someone eating a dry, processed diet. It’s all about the total volume.
When the rules change: Stage 3A vs. Stage 3B
We tend to lump Stage 3 all together, but there’s a massive difference between a GFR of 58 (Stage 3A) and a GFR of 31 (Stage 3B).
In Stage 3A, your kidneys are still pretty resilient. You can usually handle a bit of extra water without any drama. By the time you hit Stage 3B, your kidneys are nearing the "Stage 4" cliff. This is when the balance of minerals like potassium and phosphorus starts to get wonky. High water intake can sometimes dilute your sodium levels too much—a condition called hyponatremia—which is surprisingly common in older CKD patients who are trying "too hard" to be healthy.
Practical adjustments for daily life
You don't need a lab in your kitchen to manage this. You just need a routine.
💡 You might also like: Trump Says Don't Take Tylenol: Why This Medical Advice Is Stirring Controversy
Most experts recommend sipping throughout the day rather than chugging. Chugging a liter of water at once creates a "bolus" effect. It’s a sudden surge of volume that your kidneys have to process all at once. If you sip, you’re giving those tired nephrons a steady, manageable workload.
Also, pay attention to the weather. If you're sweating, you need more. If you're sedentary in an air-conditioned office, you need less. It sounds simple, but so many people stick to a rigid "8 glasses" rule regardless of what their body is actually doing.
The role of protein and water
Here is something people rarely talk about: protein. When you eat protein, your body produces urea, a waste product. Your kidneys need water to flush that urea out. If you’re on a high-protein diet (like Keto or Paleo) while having Stage 3 CKD, you’re forcing your kidneys to work double time. You’ll need more water to clear the waste, but that extra water and extra waste create more pressure (hyperfiltration).
This is why most renal dietitians suggest moderating protein. If you lower the protein, you lower the "thirst" for flushing waste, which keeps your fluid levels more stable.
Actionable steps for your next 24 hours
Stop guessing. Start measuring—just for a day or two. It’s eye-opening.
- Do a 24-hour fluid audit. Use a specific bottle and see exactly how many ounces you actually consume. Don't forget the coffee and the soup.
- Check your weight every morning. This is the gold standard for kidney patients. If you gain 2 or 3 pounds in a single day, it isn't fat. It’s water. That’s a sign your intake is outstripping your kidneys' ability to export.
- Monitor your blood pressure. If your BP is creeping up despite taking your meds, check your fluid and salt. Excess water in the bloodstream is like turning up the pressure on a garden hose.
- Talk to your nephrologist specifically about "diuretics." If you are on a "water pill" (like Furosemide or Hydrochlorothiazide), your water intake needs are totally different. These meds force your kidneys to dump water, and you have to be incredibly careful not to get dehydrated.
- Adjust for exercise. If you work out, drink about 4-8 ounces for every 20 minutes of activity, but don't go overboard.
Stage 3 is a wake-up call, not a death sentence. It’s the stage where you have the most power to slow things down. Managing your water intake isn't about following a generic rule; it’s about becoming an expert on your own internal chemistry. Keep the urine light yellow, keep the swelling down, and keep the sips steady.