Pancreatic cancer has a reputation. It's the one doctors dread. Honestly, the reason it's so terrifying isn't just the biology of the tumor itself, but the fact that the signs of pancreatic cancer are incredibly quiet until they aren't. It’s a "silent" disease. By the time someone notices something is off, the cancer has often been hitchhiking in the body for years.
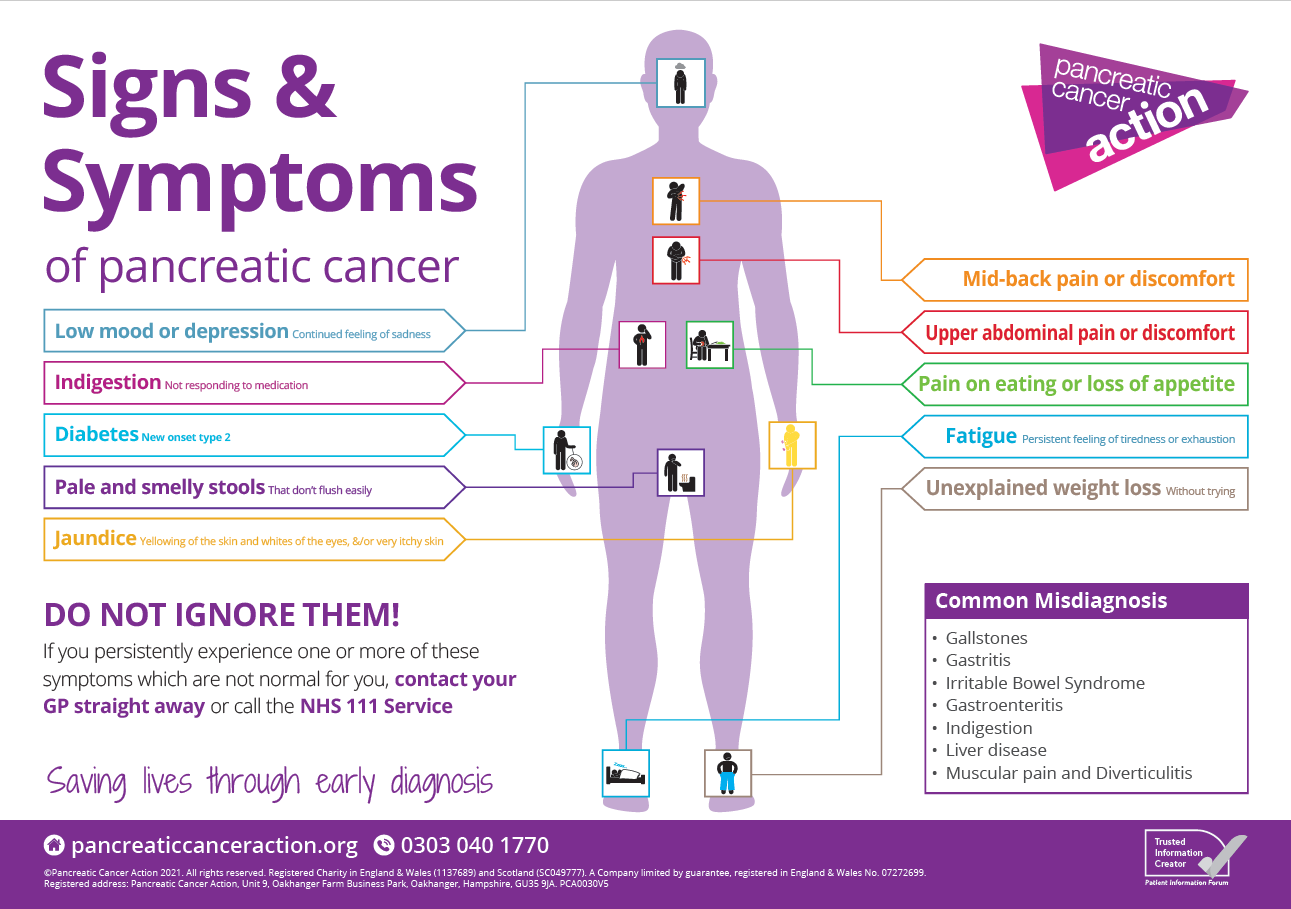
Most people think of cancer as a giant, flashing neon sign. A massive lump. Excruciating pain. But with the pancreas—a thin, carrot-shaped organ tucked deep behind your stomach—the symptoms are more like a whisper. It starts with a little indigestion. Maybe your back aches after a heavy meal. You ignore it. Why wouldn't you? Everyone has a backache sometimes.
But understanding these subtle shifts is the only way to move the needle on survival rates.
The Jaundice Red Flag (And Why It Happens)
If there is one "classic" symptom, it’s jaundice. This is when your skin and the whites of your eyes take on a yellowish tint. It’s not a tan. It’s a chemical buildup.
The pancreas sits right next to the common bile duct. If a tumor starts growing in the "head" of the pancreas, it acts like a kink in a garden hose. It pinches the duct. This stops bile—which contains bilirubin—from flowing into the intestines. Instead, that bilirubin backs up into your blood.
You might notice your pee looks like Coca-Cola. Or your poop looks like light-colored clay or putty. This happens because bilirubin is what actually gives stool its brown color. If the "brown" can't get through the duct, the stool turns gray. It’s weird. It’s unsettling. If you see this, you don't wait. You go to the ER or your GP immediately.
Dr. Anirban Maitra at MD Anderson Cancer Center has often noted that while jaundice is a clear sign, it often means the tumor is already large enough to press on surrounding structures. However, for tumors in the head of the pancreas, jaundice can actually be a "lucky" early warning that leads to faster diagnosis compared to tumors in the body or tail of the organ.
That Weird Mid-Back Pain
Back pain is a tricky one. Millions of people have bad backs. You probably sat wrong at your desk or lifted a grocery bag poorly, right? Usually, yes. But the signs of pancreatic cancer often include a very specific type of discomfort that starts in the upper abdomen and "radiates" to the back.
📖 Related: High Protein Vegan Breakfasts: Why Most People Fail and How to Actually Get It Right
Think of it like a dull pressure. It feels deep.
Because the pancreas is located near a dense cluster of nerves called the celiac plexus, a growing tumor can press against these nerves. This causes a gnawing pain. It often feels worse when you lie down flat and feels slightly better when you lean forward. If you find yourself hunched over your kitchen table because it's the only way your back doesn't throb, that's a massive clinical indicator.
Digestive Chaos and "Greasy" Stools
This is the part people don't like to talk about at dinner. The pancreas is your primary enzyme factory. It creates the juices that break down fats and proteins. When a tumor gets in the way, your body stops absorbing fat correctly.
The result? Steatorrhea.
It’s a fancy medical term for oily, foul-smelling stools that float. If you notice a film on the water in the toilet or if things are particularly difficult to flush, your pancreas might be failing to produce lipase. This isn't just "bad gas." It’s a sign of malabsorption.
People also report a sudden, "out of nowhere" loss of appetite. You sit down to eat your favorite meal and after two bites, you’re done. You feel full. Bloated. This is often dismissed as GERD or an ulcer. In fact, many pancreatic cancer patients are treated for acid reflux for six months before anyone thinks to order a CT scan.
The New-Onset Diabetes Connection
This is one of the most fascinating and overlooked signs of pancreatic cancer. If you are 55 or older and you are suddenly diagnosed with Type 2 diabetes out of the blue—especially if you are thin and have no family history of the disease—it’s a huge red flag.
👉 See also: Finding the Right Care at Texas Children's Pediatrics Baytown Without the Stress
The pancreas produces insulin. A tumor can disrupt the islet cells that regulate blood sugar.
Research published in The Lancet Gastroenterology & Hepatology suggests that new-onset diabetes can be an early paraneoplastic phenomenon. Basically, the cancer is causing the diabetes. In some cases, the blood sugar spike happens up to three years before the cancer is actually diagnosed. If your A1C jumps for no reason, ask your doctor to look at your pancreas. It might save your life.
Blood Clots and Random Swelling
Sometimes the first sign isn't in the belly at all. It's in the leg.
Trousseau’s sign of malignancy is a well-known phenomenon in oncology. Pancreatic cancer can make the blood "sticky." This leads to deep vein thrombosis (DVT)—a blood clot in a large vein, usually the leg. The leg gets red, swollen, and warm.
If that clot breaks loose, it travels to the lungs. That's a pulmonary embolism. While many things cause clots—long flights, surgery, birth control—unexplained clots in older adults are a known "silent" signal that something is wrong internally, often involving the pancreas or lungs.
Why We Miss It: The Diagnostic Gap
The reality is that the pancreas is a "deep" organ. You can't feel it during a routine physical. A doctor pressing on your stomach won't feel a small pancreatic tumor like they might feel an enlarged liver.
Standard blood tests don't usually catch it either. The CA 19-9 marker is sometimes used, but it's notoriously unreliable for early screening. Some people have high levels without cancer, and some people with cancer have normal levels.
✨ Don't miss: Finding the Healthiest Cranberry Juice to Drink: What Most People Get Wrong
We don't have a "mammogram for the pancreas" yet. This is why paying attention to the constellation of symptoms—the back pain, the weight loss, the yellowing eyes—is so vital.
The Mental Health Component
Believe it or not, some patients report a sense of "impending doom" or sudden depression months before their physical symptoms manifest. While this sounds "woo-woo," there is some clinical evidence suggesting that the systemic inflammation or hormonal changes caused by pancreatic tumors can affect neurotransmitters.
If you feel "off" and your digestion is also acting up, don't let a doctor tell you it's just stress. You know your body better than anyone else does.
Actionable Steps: What To Do Right Now
If you are worried about the signs of pancreatic cancer, don't just spiral on Google. Take these specific steps:
- Audit Your Digestion: Keep a "poop diary" for three days. Note the color, consistency, and if it floats. This sounds gross, but it’s the best data you can give a gastroenterologist.
- Track Your Weight: Unintentional weight loss is a major marker. If you’ve lost 10 pounds in a month without trying, that is a medical emergency until proven otherwise.
- Request an Endoscopic Ultrasound (EUS): If you have symptoms but a standard CT scan comes back "clear," ask about an EUS. It’s a much more sensitive test that can see smaller lesions that a CT might miss.
- Check Your Family Tree: About 10% of these cancers are hereditary. If two or more first-degree relatives had it, or if you carry the BRCA1 or BRCA2 gene mutations (the "breast cancer genes"), your risk profile is different. You may qualify for specialized screening programs like the CAPS (Cancer of the Pancreas Screening) study.
- Consult a Specialist: If you have new-onset diabetes and upper abdominal pain, see a Gastroenterologist, not just a General Practitioner. Specialists are more likely to recognize the pattern.
Early detection is difficult, but not impossible. By the time the world hears about a celebrity like Patrick Swayze or Steve Jobs, the battle is usually late-stage. But for the average person, being a "difficult patient" who insists on imaging when things don't feel right is often what leads to a surgical window—the only real chance for a cure.
Stay vigilant about your metabolic health. If your skin yellows or your digestion changes overnight, act. Your pancreas is quiet, but it speaks in code. You just have to learn how to listen.