Movies lied to us. We’ve all seen the scene where a character suddenly clutches their chest, eyes bulging, and collapses dramatically onto the floor. It’s cinematic. It’s clear. It’s also kinda rare in real life. Most people waiting for that "Hollywood moment" end up sitting on their couch for three hours wondering if they just ate too much spicy pizza. They wait. They hope it goes away. And honestly, that’s the most dangerous thing you can do when your body is trying to tell you something is wrong.
Understanding the signs of heart attack isn't just about memorizing a checklist; it's about recognizing how your specific body reacts to a plumbing problem in your chest. A myocardial infarction—the medical term for a heart attack—happens when blood flow to the heart muscle is severely reduced or cut off. This is usually due to a buildup of fat, cholesterol, and other substances, which form a plaque in the arteries. When that plaque ruptures, a clot forms. If that clot blocks the "pipe," the muscle starts to die. Fast.
What Most People Get Wrong About Chest Pain
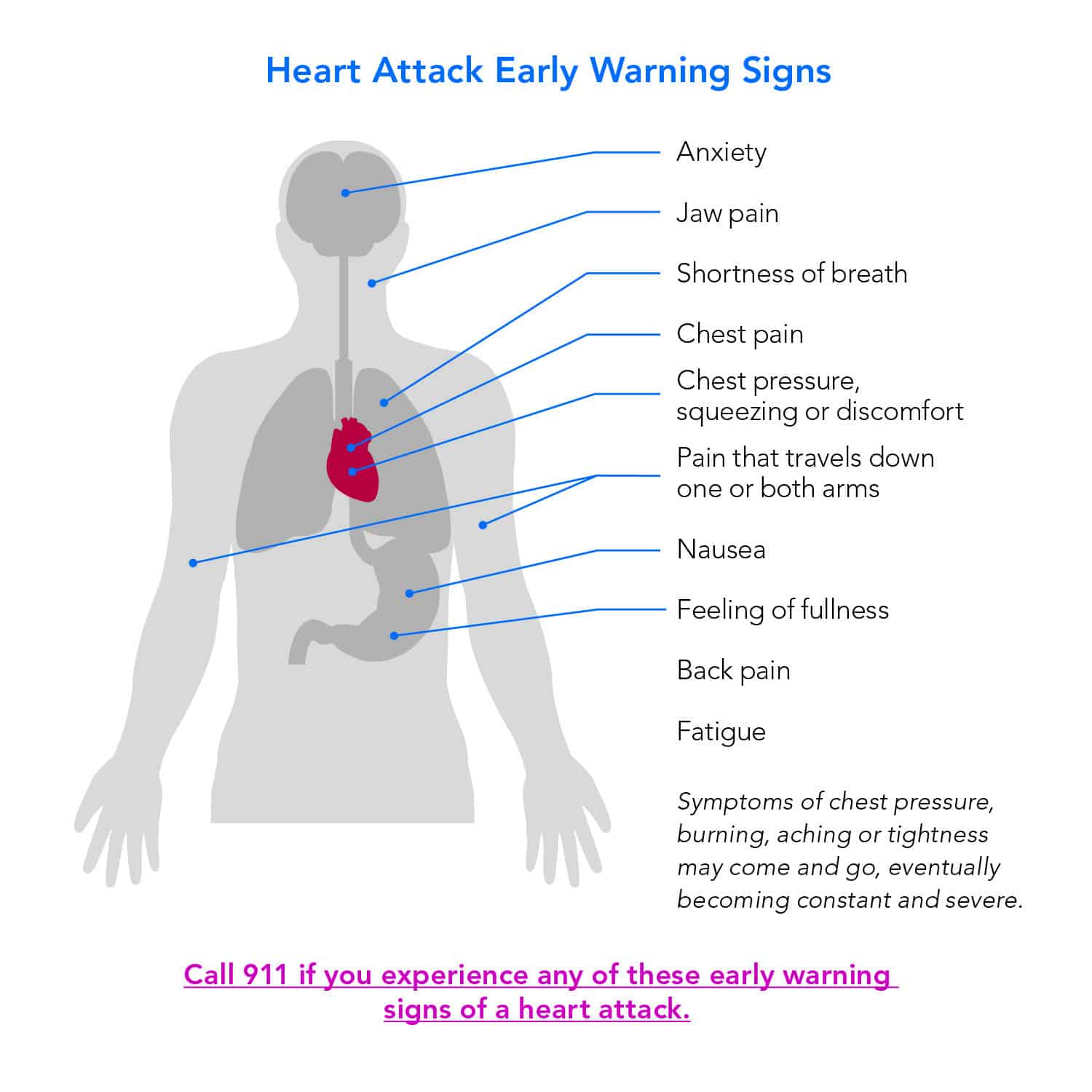
Everyone talks about "crushing" pain. Doctors often describe it as an elephant sitting on your chest. But here’s the thing: it might just feel like pressure. Or a weird squeezing. Some patients I’ve talked to described it as a "fullness," like they swallowed something too big and it got stuck right behind the breastbone.
It’s not always sharp. In fact, if it’s a sharp, stabbing pain that happens when you take a deep breath, it might be something else, like pleurisy or a pulled muscle. Heart attack pain is usually dull, heavy, and persistent. It might last for a few minutes, go away, and then come back with a vengeance. That "stop and start" nature is a massive red flag.
Don't assume it has to be on the left side, either. While the heart is slightly to the left, the discomfort often radiates to the center of the chest. It can feel like it’s spreading to your shoulders, your neck, or even your jaw. I once knew a guy who went to the dentist because his lower teeth ached so badly, only to find out he was actually mid-infarction. That’s how tricky the nervous system can be. The nerves that serve the heart and the nerves that serve the jaw are basically neighbors in the spinal cord, and sometimes the brain gets the signals mixed up. It’s called referred pain.
The Gender Gap in Symptoms
This is where things get really complicated. For a long time, medical research focused almost exclusively on men. Because of that, the "standard" symptoms we hear about are often the ones men experience. Women are much more likely to have "atypical" presentations.
A woman might not feel any chest pressure at all. Instead, she might experience extreme, unexplained fatigue. We’re talking about the kind of tired where you can’t walk from the kitchen to the living room without needing a nap. Shortness of breath, nausea, and lightheadedness are also huge markers for women.
📖 Related: Orgain Organic Plant Based Protein: What Most People Get Wrong
According to the American Heart Association (AHA), women are also more likely to experience pain in the back or the jaw. Because these symptoms don't scream "heart," many women wait longer to go to the ER. They think they have the flu. They think they’re just stressed or "getting older." This delay is why heart attacks are often more fatal for women than for men. If you’re a woman and you feel like you’ve been hit by a truck for no reason, coupled with a sense of "impending doom," take it seriously.
That "Funny Feeling" in Your Stomach
Is it indigestion? Or is it a signs of heart attack? This is the million-dollar question that leads to thousands of people taking Tums when they should be calling 911.
The heart sits right above the diaphragm, which sits right above the stomach. When the bottom part of the heart (the inferior wall) isn't getting enough oxygen, it can irritate the nerves that trigger nausea. You might feel "queasy." You might actually vomit.
- The Sweat Test: If you’re feeling "indigestion" but you’re also breaking out in a cold, clammy sweat (the kind of sweat you get when you have a high fever, but your skin is cold), it’s almost certainly not the pizza.
- The Activity Link: If the "heartburn" gets worse when you walk around and better when you sit still, that’s a classic sign of angina or an evolving heart attack. Real acid reflux doesn't usually care if you're walking or sitting; it cares if you're lying flat.
Silent Heart Attacks are Real
You might have already had one. It sounds terrifying, but "silent" myocardial infarctions (SMIs) account for nearly 45% of all heart attacks. These don't have the classic symptoms. They might feel like a mild case of the flu or a strained muscle in the upper back.
Usually, people only find out they had one months or years later during a routine EKG. The problem is that even though you didn't feel it, the damage was done. Scar tissue forms where the muscle died, which makes your heart less efficient and sets the stage for heart failure or a second, much louder heart attack later on.
People with diabetes are particularly at risk for silent heart attacks. Over time, high blood sugar can damage the nerves (neuropathy) that carry pain signals from the heart to the brain. If the "alarm system" is broken, you won't hear the sirens.
👉 See also: National Breast Cancer Awareness Month and the Dates That Actually Matter
The Role of "Impending Doom"
There’s a symptom that doctors don't always put on the brochures, but it’s incredibly common: a sense of impending doom. It sounds like something out of a gothic novel, but it’s a real physiological response. Your body knows the heart is struggling before your conscious mind does. Your sympathetic nervous system goes into overdrive—the "fight or flight" response. This floods your system with adrenaline.
You might feel an overwhelming sense of anxiety or a feeling that you’re about to die. If you’re feeling this alongside any physical discomfort, don't let anyone tell you that you're "just having a panic attack." It’s better to be told it’s anxiety in the ER than to be treated for a heart attack in the morgue.
When to Act and What to Actually Do
Timing is everything. There’s a saying in cardiology: "Time is muscle." Every minute the blood flow is blocked, more heart cells die. Once they're gone, they don't grow back.
If you suspect you're experiencing signs of heart attack, here is the protocol.
First, call emergency services immediately. Do not—and I cannot stress this enough—try to drive yourself to the hospital. If you black out behind the wheel, you're not just a heart patient; you're a car crash victim and a danger to everyone else on the road. Paramedics can start treatment the second they walk through your door. They have EKGs in the ambulance. They can transmit that data to the hospital so the catheterization lab is ready the moment you arrive.
Second, if you aren't allergic, chew a full-strength aspirin (325mg). Chewing it helps it get into your bloodstream faster than swallowing it whole. Aspirin helps thin the blood and can prevent the clot from getting larger while you wait for help.
✨ Don't miss: Mayo Clinic: What Most People Get Wrong About the Best Hospital in the World
Third, sit down. Try to stay calm. Loosen any tight clothing. Don't try "cough CPR"—that's an internet myth that doesn't actually work and can waste precious energy.
Risk Factors vs. Reality
We all know the risks: smoking, high blood pressure, high cholesterol, and obesity. But plenty of "healthy" people have heart attacks too. Genetics play a massive role. If your father had a heart attack at 45, your "low cholesterol" might be giving you a false sense of security.
Lipoprotein(a), often called "Lp-little-a," is a type of cholesterol that is mostly determined by your genes and isn't usually measured in a standard lipid panel. You could have a perfect LDL score and still be at high risk because of this specific protein. If you have a strong family history of early heart disease, ask your doctor for a more detailed screening.
Inflammation is another huge factor. Conditions like rheumatoid arthritis or lupus can increase your risk because chronic inflammation damages the lining of the blood vessels. Stress, too, isn't just a mental state; it’s a physical one. Chronic stress keeps your cortisol levels high, which hardens arteries over time.
Actionable Steps for Your Next Checkup
Most people go to the doctor and just wait for the "all clear." You need to be your own advocate. Don't just settle for a blood pressure reading.
- Ask for your numbers: Know your blood pressure, your LDL (the "bad" cholesterol), and your A1C (blood sugar).
- Request a CAC Score: A Coronary Artery Calcium (CAC) scan is a quick, non-invasive CT scan that looks for actual calcified plaque in your heart's arteries. It’s a much better predictor of risk than just a blood test.
- Review your family tree: Go beyond "grandpa had heart issues." Find out when. Was he 50 or 85? Early onset in family members is the biggest red flag.
- Listen to your "baseline": Start paying attention to what your body feels like when it's healthy. If you usually climb three flights of stairs without thinking, and suddenly you're winded after one, that's your "check engine" light.
The reality is that many heart attacks are preventable, and almost all are treatable if you catch them in time. The biggest hurdle isn't medical technology—it's human denial. We don't want to be the person who called an ambulance for "just gas." But here’s the truth: the ER doctors would much rather send you home with a prescription for antacids than admit you to the ICU because you waited too long.
If you feel something weird in your chest, neck, or arms—especially if it’s accompanied by a sweat or a feeling of dread—make the call. You aren't being dramatic. You're being smart.