You’re sitting there after a heavy dinner—maybe it was pizza, maybe a burger—and suddenly, there it is. A sharp, gnawing pressure right under your ribs on the right side. You might think it’s just bad indigestion or that the pepperoni is fighting back. Honestly, that’s how it starts for almost everyone. But then the pain migrates. It creeps up into your right shoulder blade or settles into a dull, heavy ache that makes you want to pace the floor at 2:00 AM.
That is the classic calling card of a biliary colic episode.
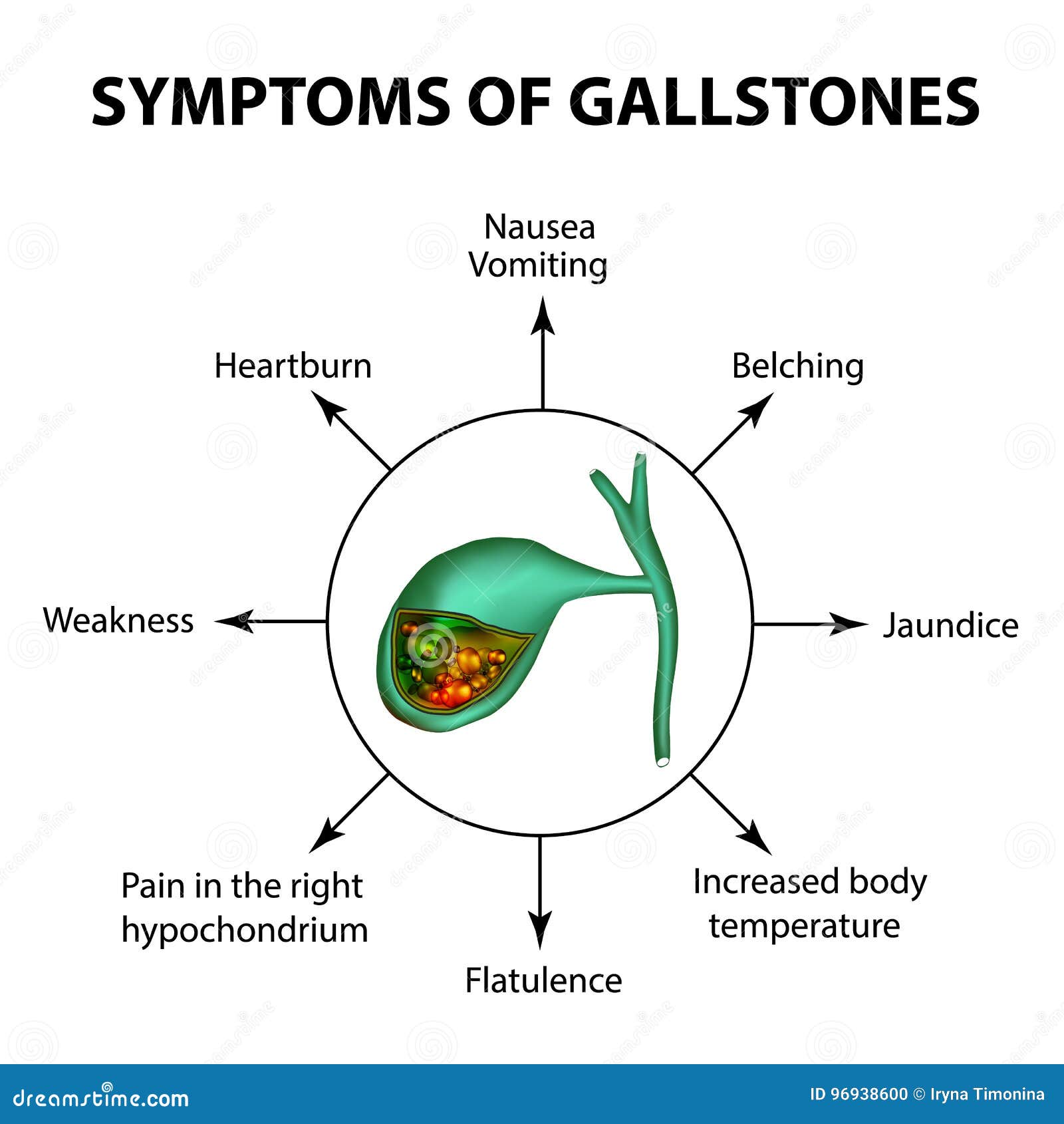
Understanding the signs of gall bladder problems isn't just about knowing where it hurts; it's about realizing that your gallbladder is basically a tiny storage pouch for bile, and when it stops working right, your whole digestive system goes sideways. Most people think they'll just see "yellow skin" and know they're in trouble. It’s rarely that simple. Sometimes it’s just a weird feeling of being "off" after a greasy meal. Other times, it's a full-blown emergency room visit because you’re convinced you’re having a heart attack.
🔗 Read more: Tdap Shot During Pregnancy: Why the Timing Actually Matters
The Pain Profile: It’s Not Just a Stomach Ache
The pain associated with gallbladder issues is distinct. Doctors often call it "biliary colic." It doesn’t usually throb like a headache. It’s a steady, intense pressure. You’ll feel it in the upper right quadrant of your abdomen. But here is the kicker: the nerves in that area are messy. They branch out. Because of this, many patients report "referred pain." This means you might feel the signs of gall bladder problems in your back, specifically between the shoulder blades, or even in your right shoulder.
It’s a deep ache. It lasts.
Usually, an attack peaks within an hour and then slowly fades over several hours. If it lasts more than six hours, you aren't just dealing with a "lazy" gallbladder or a small stone passing; you might be looking at cholecystitis, which is a fancy word for inflammation. According to the Mayo Clinic, this happens when a gallstone gets stuck in the cystic duct, backing up bile and causing the organ to swell like a balloon. It’s incredibly uncomfortable. You might find yourself unable to get comfortable in any position—sitting, standing, or lying down doesn't help.
Why the "Fatty Meal" Connection Matters
Bile's whole job is to break down fats. When you eat something greasy, your small intestine sends a hormonal signal (cholecystokinin) to the gallbladder: "Hey, squeeze out some bile!" If you have stones or sludge, that squeeze causes the gallbladder to contract against an obstruction.
That's why the timing of your pain is a massive clue. If you feel fine most of the day but feel like you’ve been punched in the ribs 30 minutes after eating fried chicken or a creamy pasta, your gallbladder is screaming for help.
Beyond the Pain: The "Silent" Digestive Red Flags
Sometimes, there is no sharp pain. Instead, you get a collection of symptoms that people often mistake for Irritable Bowel Syndrome (IBS) or simple acid reflux. Chronic signs of gall bladder problems can be subtle. We’re talking about persistent bloating that doesn't go away with Antacids. Or maybe it's "fatty" stools.
If your poop is light-colored, grayish, or even clay-like, pay attention. This happens because bilirubin—the pigment that makes stool brown—isn't reaching the digestive tract because the bile duct is blocked. If your stool floats or looks oily, that’s malabsorption. Your body isn't processing the fats you eat. Instead of being broken down and used, the fat just passes through you. It’s messy, it’s gross, and it’s a definitive sign that the bile flow is compromised.
Nausea is another big one. Not just "I feel sick" nausea, but a chronic, low-grade queasiness that seems to hang around after meals. You might find yourself burping way more than usual. Some people describe it as a "heavy" feeling in the gut, like they’ve swallowed a lead weight.
The Jaundice Myth
Let's talk about the yellowing of the skin and eyes. While jaundice is a hallmark of gallbladder and liver issues, it usually means the problem has progressed significantly. You shouldn't wait for your eyes to turn yellow to see a doctor. By the time jaundice appears, a stone has likely moved out of the gallbladder and into the common bile duct, blocking the exit for both the gallbladder and potentially the liver. This is a "red alert" situation.
Who Is Actually at Risk? (The 4 F’s and More)
Medical students have been taught the "4 F's" for decades: Female, Fat, Forty, and Fertile. It’s a bit of a crude mnemonic, but it’s rooted in statistical reality. Estrogen increases cholesterol in the bile and decreases gallbladder contractions. This is why women, especially those who have been pregnant or are on birth control, are at a higher risk.
But honestly? The "4 F's" are an oversimplification.
Rapid weight loss is a huge, often overlooked trigger. When you lose weight very quickly—think bariatric surgery or crash dieting—your liver secretes extra cholesterol into the bile. This can lead to "sludge" or stones forming almost overnight. If you've recently dropped 20 pounds in a month and suddenly start feeling upper abdominal pressure, don't ignore it.
Diabetics also face a higher risk. The correlation isn't perfectly understood, but it’s believed that higher levels of triglycerides and autonomic neuropathy (which affects how the gallbladder contracts) play a role. If you have Type 2 diabetes, you might not even feel the typical "sharp" pain because of nerve damage, making the other signs of gall bladder problems, like nausea and bloating, even more important to track.
The "HIDA" Scan and Why Ultrasounds Miss Things
You go to the doctor. They run an ultrasound. They tell you, "Everything looks clear! No stones!"
You leave feeling crazy because you know something is wrong.
Here is what most people (and even some general practitioners) get wrong: you can have a "sick" gallbladder without having stones. This is called Acalculous Cholecystitis or Biliary Dyskinesia. Basically, your gallbladder is just lazy. It isn't squeezing the bile out effectively.
An ultrasound is great for seeing solid stones. It sucks at seeing how the organ functions. This is where a HIDA scan (Hepatobiliary Iminodiacetic Acid scan) comes in. They inject a radioactive tracer that travels to your liver and then your gallbladder. Then, they give you a "fatty meal" in a cup or an injection of a hormone that makes the gallbladder squeeze. They measure the "ejection fraction." If your gallbladder only squeezes out 15% of its contents instead of the normal 35-50%, you've found your problem.
It’s a functional issue, not a structural one.
Long-term Complications: What Happens If You Ignore It?
Ignoring the signs of gall bladder problems is a dangerous game. It’s not just about the pain. A blocked duct can lead to a backup that affects the pancreas. This is called gallstone pancreatitis. The pancreas is a temperamental organ; when it gets inflamed, it's an excruciating, life-threatening situation.
There’s also the risk of "porcelain gallbladder." This is when the gallbladder walls become calcified due to chronic inflammation. It sounds fancy, but it actually increases the risk of gallbladder cancer. While rare, it's not something you want to gamble with.
Actionable Steps: What to Do Right Now
If you suspect your gallbladder is acting up, you need a plan that goes beyond just "waiting for it to pass."
✨ Don't miss: Does Pot Help With Back Pain? What the Science Actually Says vs. The Hype
- Track the triggers. Keep a food diary for 72 hours. Be specific. Did the pain start after the avocado toast or the black coffee? High-fat foods are the usual suspects, but sometimes even healthy fats (like nuts or olive oil) can trigger a sensitive gallbladder.
- Check your temperature. If you have abdominal pain accompanied by a fever or chills, stop reading this and go to Urgent Care. That indicates an infection.
- The "Jump Test." This is an old-school trick. If you have sharp pain in your right side and jumping up and down (or even just walking) makes the pain jar and feel significantly worse, it might be inflammation of the lining (peritonitis) or a very angry gallbladder.
- Ask for the right tests. If a standard ultrasound comes back clear but the symptoms persist, specifically ask your gastroenterologist about a HIDA scan or an Endoscopic Ultrasound (EUS). An EUS can find "micro-stones" or sludge that a regular scan misses.
- Modify the diet immediately. Switch to a low-fat, high-fiber diet to take the pressure off. Think steamed vegetables, lean proteins like chicken breast or white fish, and whole grains. Avoid "trigger" vegetables like broccoli or onions if you’re also experiencing heavy gas.
- Hydrate, but wisely. Water is essential, but avoid carbonated drinks which can worsen the bloating and pressure in the upper abdomen.
The gallbladder is one of those organs you don't think about until it's the only thing you can think about. It’s small, but it’s mighty. When it fails, it impacts everything from your energy levels to your bathroom habits. Listen to the subtle cues—the bloating, the weird shoulder pain, the nausea—before they turn into an emergency. Taking the signs of gall bladder problems seriously today can save you from a surgical emergency tomorrow.
Talk to a specialist. Get the imaging. Don't let a "clear" ultrasound talk you out of what your body is clearly telling you.