Honestly, the way movies portray heart attacks is a total lie. You’ve seen it: some guy clutches his chest, gasps for air, and falls face-first onto the sidewalk. It’s dramatic. It’s loud. It’s also kinda rare. Real life is usually much messier and way more subtle. Knowing the signs of a heart attack isn't just about spotting a "Hollywood moment." It’s about catching that weird, nagging ache in your jaw that won't go away or the sudden "flu-like" exhaustion that hits you on a Tuesday afternoon.
People wait. They wait because they aren't sure. They don't want to look stupid calling 911 for "indigestion." But every second your heart muscle is starved of oxygen-rich blood, it's dying. It’s that simple.
The Chest Pain Myth (and Reality)
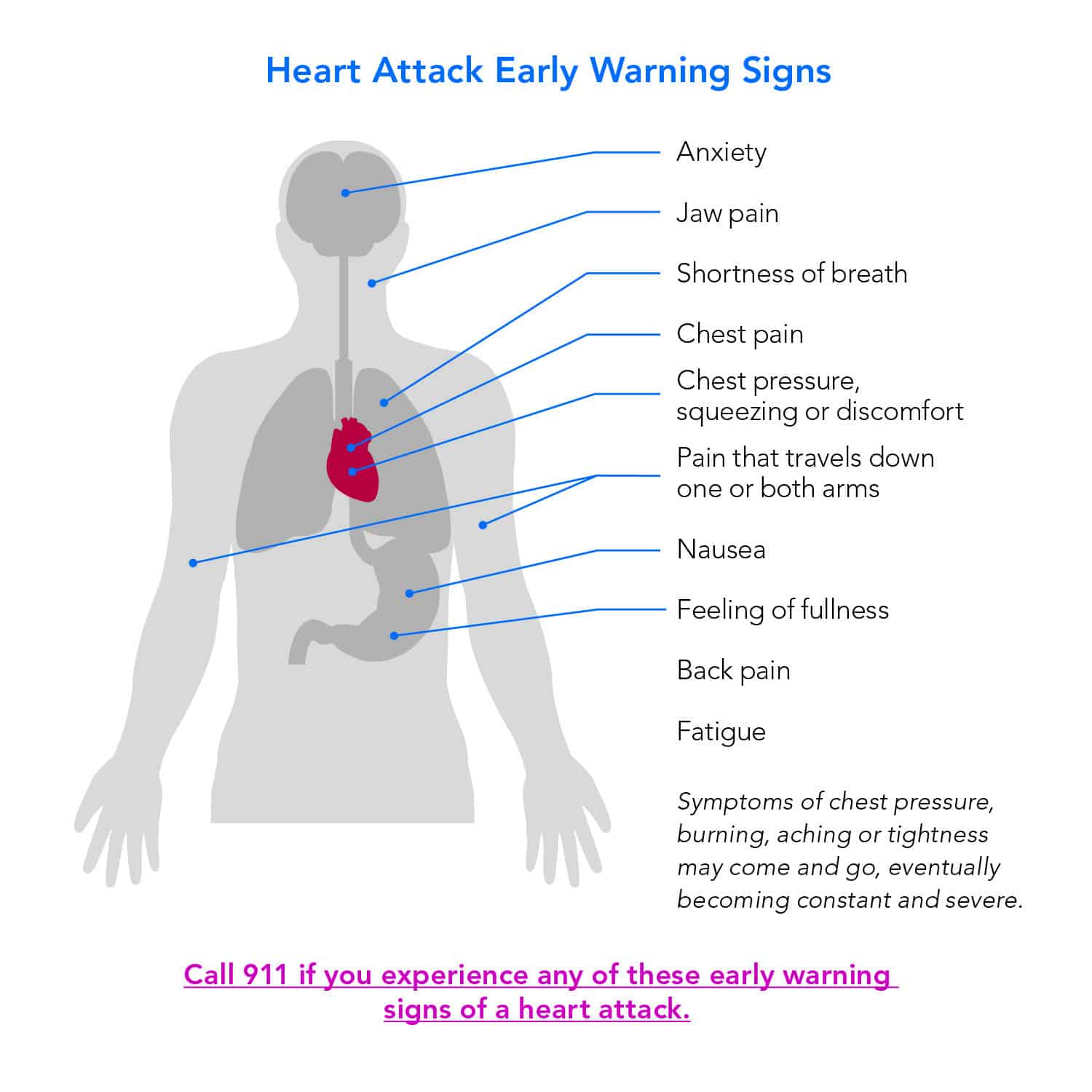
Everyone talks about the "elephant sitting on your chest." That’s the classic description doctors at the Mayo Clinic and American Heart Association still use because it happens often. But it isn't always sharp. For many, it's just a vague pressure. It's discomfort. It’s a feeling of fullness or a squeezing sensation that lasts for more than a few minutes or goes away and comes back.
📖 Related: Why Your Low Carb Diet Macro Calculator Might Be Lying to You
Think about it like this: your heart is screaming for help, but the signals get crossed. The pain doesn't stay in the chest. It travels. It creeps up into your neck. It radiates down your left arm—or sometimes the right one, which confuses people. It can even settle in your back between your shoulder blades. If you’re feeling a dull ache in your jaw that you can't explain by a trip to the dentist, you need to pay attention.
The discomfort is often "stuttering." It’s not always a constant, escalating agony. It might feel like bad heartburn. You take an antacid. It doesn't help. You sit down. It eases up. You stand up. It returns. That pattern is a massive red flag.
Why Women Experience Different Signs of a Heart Attack
This is where it gets complicated. Men and women don’t always experience the same symptoms, and this discrepancy kills people. Women are significantly more likely to report "atypical" symptoms.
Instead of crushing chest pressure, a woman might feel an overwhelming sense of fatigue. I’m talking about the kind of tired where you can’t even lift a coffee cup. You might feel nauseous or actually vomit. It’s easy to write this off as a stomach bug or a long week at work. But if that nausea is paired with shortness of breath or a cold sweat, it’s not the flu.
Dr. Nieca Goldberg, a leading cardiologist and author, has spent years pointing out that women’s symptoms are often dismissed—even by doctors. Women tend to have blockages not just in the main arteries, but in the smaller ones that branch out, a condition called small vessel heart disease. This leads to a different sensation. It’s more of a diffuse ache or a feeling of "doom."
- Shortness of breath without a clear reason.
- Lightheadedness or actual fainting.
- Pressure in the upper back that feels like a pulled muscle but won't quit.
- Breaking out in a cold sweat while sitting perfectly still.
The "Silent" Killers and Diabetic Nuance
If you have diabetes, your internal "alarm system" might be broken. High blood sugar over years can damage the nerves that carry pain signals from your heart to your brain. This is called autonomic neuropathy.
✨ Don't miss: Why "You're Not Good Enough" Is Actually Your Brain Being Lazy
Basically, you could be having a full-blown myocardial infarction and feel almost nothing. Maybe you just feel a bit "off." Maybe you’re suddenly breathless while walking to the mailbox. This is why regular screenings are non-negotiable for the diabetic community. You can’t rely on pain as your guide.
Then there’s the "silent" heart attack. These are often discovered weeks or months later during a routine EKG. The patient might remember a "bad bout of indigestion" or a "rough couple of days with the flu." In reality, their heart was struggling to survive.
The Biology of What’s Actually Happening
Your heart is a pump. It needs its own fuel. This fuel arrives via the coronary arteries. A heart attack happens when one of these "fuel lines" gets gunked up with plaque—a mix of fat, cholesterol, and other waste.
When a piece of that plaque ruptures, a blood clot forms around it. Boom. The pipe is blocked.
The muscle downstream from that blockage starts to suffocate. Within minutes, cells begin to die. This is why cardiologists say "time is muscle." The longer the blockage lasts, the more permanent the damage. If you get to a hospital quickly, doctors can use "clot-busting" drugs or perform an angioplasty to shove that artery open with a stent. If you wait eight hours? That part of your heart might never beat again, leading to chronic heart failure.
Warning Signs Most People Ignore
- The "Gray" Look: If you look in the mirror and your skin looks ashen or gray, and you're sweating despite being cold, your circulatory system is failing.
- Sudden Anxiety: Some people describe an "impending sense of doom." It sounds "woo-woo," but it’s a documented physiological response to a massive internal stressor.
- Sleep Disturbances: Many people who have had heart attacks report waking up gasping for air or being unable to sleep due to a weird discomfort in the days leading up to the event.
What to Do (And What NOT to Do)
If you suspect you or someone else is showing signs of a heart attack, the first thing you do is call 911. Do not drive yourself to the hospital. If you black out behind the wheel, you’re a danger to yourself and everyone else. Plus, paramedics can start treatment the second they walk through your door. They have EKGs in the ambulance. They can transmit that data to the ER before you even arrive.
Chew an aspirin. Don't just swallow it. Chewing it gets the medicine into your bloodstream faster. Aspirin helps thin the blood and can prevent the clot from getting worse. But—and this is important—only do this if you aren't allergic and haven't been told by a doctor never to take it.
Do not "wait and see." Do not wait for the pain to become "bad enough." Hospitals would much rather send you home with a prescription for Pepcid than have you arrive too late for life-saving intervention.
Risk Factors vs. Reality
We all know the usual suspects: smoking, high blood pressure, and high cholesterol. But genetics plays a massive role. You can be a marathon-running vegan and still have a heart attack if your family tree is littered with early cardiac events.
Lipoprotein(a), or Lp(a), is a specific type of cholesterol that is purely genetic. Standard tests often miss it. If you have high Lp(a), your risk is elevated regardless of how many salads you eat. This is why understanding your family history is just as vital as knowing the signs of a heart attack.
The Mental Health Connection
Stress isn't just "in your head." Chronic stress keeps your cortisol levels high and your blood vessels constricted. "Broken Heart Syndrome" (Takotsubo cardiomyopathy) is a real thing. It can mimic a heart attack perfectly—chest pain, EKG changes—but it's often triggered by severe emotional distress. While it's usually temporary, it shows just how much the brain and the heart are tethered together.
Taking Action Today
Prevention is the boring part, but it's the part that keeps you alive. It's not about one giant lifestyle change; it's about the small, annoying stuff.
- Get a Calcium Score: If you’re over 40, ask your doctor about a CT calcium scan. It's a quick, non-invasive way to see if there's actual calcified plaque in your arteries. It’s way more predictive than just a cholesterol number.
- Know Your Numbers: "Good" blood pressure is now considered 120/80 or lower. If you're consistently at 130/90, you're already in the danger zone.
- Move Your Body: You don't need to run a 5K. A 20-minute brisk walk changes the way your blood vessels dilate.
- Listen to Your Gut: If something feels wrong, it probably is. You know your body better than any textbook.
If you feel a weird pressure that moves to your neck, or if you're suddenly sweating buckets while sitting on the couch, call emergency services. Forget your pride. Forget the cost of the ambulance. Your heart is the only one you've got.
Immediate Steps to Take:
- Store your medical history and a list of current medications on your phone's "Medical ID" feature so first responders can see it even if your phone is locked.
- Schedule a dedicated "heart health" check-up specifically to discuss your risk factors, rather than just waiting for a generic physical.
- Purchase a home blood pressure cuff and track your readings for one week. Bring that log to your doctor. One reading in a stressful doctor's office is rarely accurate.
- Talk to your immediate family about their history. Find out if anyone had a "sudden" event before age 55 (for men) or 65 (for women).