If you’ve reached the point where you’re scouring the internet for grade 4 hemorrhoids pictures, things have likely gotten pretty uncomfortable. You aren't just dealing with a bit of itching anymore. It's painful. It’s physically invasive. Honestly, seeing those images for the first time can be a total shock to the system because grade 4 is the most advanced stage of hemorrhoidal disease. We’re talking about internal tissues that have migrated outside the body and, frankly, refuse to go back in.
It’s scary.
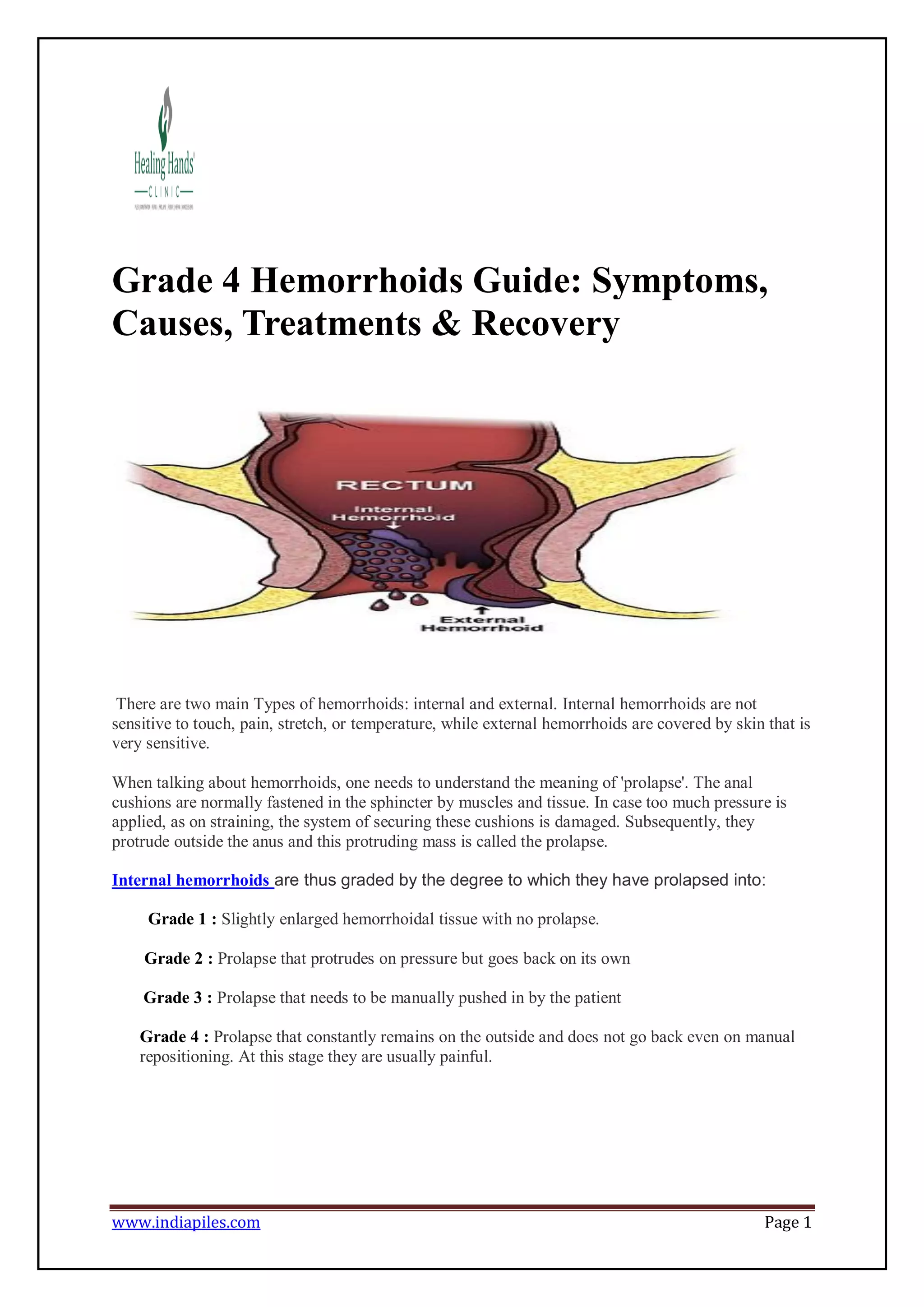
Most people start their journey with a little blood on the tissue. They ignore it. Then comes the "prolapse"—that feeling of something popping out during a bowel movement. In the earlier stages, like grade 2 or 3, you can usually push that tissue back in, or it might even slide back on its own. But grade 4? That’s a different beast entirely. At this stage, the hemorrhoids are permanently prolapsed. No amount of pushing or manual "reduction" is going to fix it. When you look at grade 4 hemorrhoids pictures, you’re seeing what doctors call "incarcerated" or "strangulated" tissue. It's often dark, swollen, and looks nothing like the healthy skin around it.
Why Grade 4 Hemorrhoids Look So Intense
When you look at medical diagrams or actual clinical photos, the first thing you’ll notice is the color. It isn’t just pink. Because the blood flow is often constricted, the tissue can turn a deep purple, blue, or even a necrotic black. This happens because the anal sphincter muscle is basically acting like a tiny, unintended tourniquet. It’s squeezing the life out of the hemorrhoid.
This isn't just a cosmetic issue.
Medical experts like Dr. Gary Hoffman at the Los Angeles Colon and Rectal Surgical Associates often point out that grade 4 cases frequently involve thrombosis. That’s a fancy way of saying a blood clot has formed inside the hemorrhoid. If you've seen a photo where the area looks like a shiny, tense grape, that's likely a thrombosed external component or a severely prolapsed internal one. It hurts. A lot. It's a sharp, stabbing, "I can't sit down" kind of pain.
Identifying the Mess: Prolapse vs. Skin Tags
It’s actually pretty common for people to misidentify what they’re seeing. You might see a fleshy growth and think, "Yep, that’s a grade 4," when it’s actually just a large skin tag left over from a previous flare-up.
💡 You might also like: Can DayQuil Be Taken At Night: What Happens If You Skip NyQuil
Here is how to tell the difference without a medical degree:
- Grade 4 Hemorrhoids usually feel wet. Since they are technically internal lining (mucosa) now living on the outside, they secrete mucus. This can lead to something doctors call "soiling," where you find moisture or fecal matter on your underwear even after wiping well.
- Anal Skin Tags are just skin. They don't bleed much, they don't secrete mucus, and they aren't usually purple. They’re annoying, but they aren't a medical emergency.
- Rectal Prolapse is the "big brother" of hemorrhoids. This is where the actual wall of the rectum slides out. In photos, this looks like a series of concentric rings of tissue, almost like a small red telescope. Grade 4 hemorrhoids usually look more like distinct lobes or bunches.
The Physical Reality of Living with Grade 4
The daily grind of this condition is exhausting. You’re constantly managing hygiene. Because the tissue is stuck outside, the anal seal isn't tight. This leads to "pruritus ani"—which is just the medical term for a persistent, maddening itch caused by constant moisture and irritation.
You can't just "fiber" your way out of this.
While every doctor on the planet will tell you to eat more broccoli and drink more water, at grade 4, the structural integrity of the connective tissue (the Parks' ligament) has basically given up. It's stretched beyond its elastic limit. Think of it like a rubber band that’s been pulled so many times it finally snapped. No amount of Metamucil is going to pull that tissue back up into the anal canal.
According to the American Society of Colon and Rectal Surgeons (ASCRS), grade 4 hemorrhoids are often the primary indicator that surgery is no longer an "option" but a necessity.
What the Pictures Don't Show: The Risk of Gangrene
It sounds dramatic. It is dramatic.
📖 Related: Nuts Are Keto Friendly (Usually), But These 3 Mistakes Will Kick You Out Of Ketosis
When a hemorrhoid is grade 4, it can become "strangulated." This means the blood supply is cut off so completely that the tissue begins to die. In clinical grade 4 hemorrhoids pictures, you might see areas that look greenish or black. This is a sign of tissue death (necrosis). If this happens, the pain often shifts from a dull ache to a localized, intense throbbing.
This is where you stop googling and start driving to the ER.
The risk of infection at this stage is real. You have open, dying tissue in an area that is—by definition—not a sterile environment. Sepsis is rare, but local abscesses are not. If you see pus or have a fever along with the visible prolapse, the situation has moved past simple "hemorrhoid management."
Cutting Through the "Natural Cure" Noise
You'll see ads. We all see them. "Shrink your grade 4 hemorrhoids with this one weird root!" or "The 24-hour miracle cream."
Let’s be real for a second.
If you truly have grade 4 hemorrhoids, those creams are basically like putting a Band-Aid on a broken leg. They might numb the surface. They might reduce the swelling for an hour. But the structural failure—the prolapse—is mechanical. You cannot "cream" a mechanical displacement back into place.
👉 See also: That Time a Doctor With Measles Treating Kids Sparked a Massive Health Crisis
Surgical Pathways: What Actually Works?
Since grade 4 is the "end of the line" for conservative treatment, surgery is usually the conversation you’ll have with a proctologist. It’s not the 1950s anymore; you have options, though none of them are exactly a walk in the park.
The Traditional Hemorrhoidectomy
This is the "gold standard," and honestly, the one most people dread. Doctors like those at the Cleveland Clinic often reserve this for the most severe grade 4 cases. They literally cut the excess tissue away. It’s highly effective—the recurrence rate is incredibly low—but the recovery is legendary for being tough. You’ll be on a first-name basis with your sitz bath for a few weeks.
Stapled Hemorrhopexy (PPH)
This one is interesting. Instead of cutting the tissue off on the outside, a surgeon uses a circular stapling device to "hoist" the tissue back up and staple it into place. It cuts off the blood supply to the excess tissue so it shrinks, while simultaneously re-anchoring the prolapse. It usually hurts less than a traditional excision, but it has a slightly higher risk of the hemorrhoids coming back later.
THD (Transanal Hemorrhoidal Dearterialization)
This is a more modern, "minimally invasive" approach. Using ultrasound, the surgeon finds the specific arteries feeding the hemorrhoid and ties them off. No cutting of the actual sensitive skin. For some grade 4 patients, this is a godsend, but if there's too much "excess" skin, you might still end up needing a bit of a trim.
Taking Action Today
If you’ve been looking at grade 4 hemorrhoids pictures and they match what you see in the mirror, your first step is a formal diagnosis. Don't self-diagnose based on a JPEG. Other conditions, like anal cancer or large polyps, can sometimes mimic the appearance of a grade 4 hemorrhoid to the untrained eye.
Start by tracking your symptoms. Is there a fever? Is the pain constant or only during movements?
If the tissue is purple or black, seek immediate medical attention at an urgent care or emergency room. This indicates a lack of blood flow that needs to be addressed before the tissue becomes necrotic.
For those not in an emergency state but definitely at grade 4, schedule a consultation with a board-certified colorectal surgeon. General practitioners often lack the specialized equipment (like an anoscope or proctoscope) to fully grade the extent of the internal damage. In the meantime, switch to using a bidet or unscented wet wipes; dry toilet paper on grade 4 tissue is like using sandpaper on an open wound. Keep the area as dry as possible after cleaning to prevent the skin from breaking down further.