Let’s be honest. Nobody actually wants a chronic, life-altering mental health diagnosis. When people search for schedule 1 how to get schizophrenic, they usually aren’t looking for a "how-to" guide on developing a brain disorder. Usually, they are terrified. Maybe they’ve been experimenting with substances and started hearing things that aren't there. Or maybe they are worried that a heavy weekend of drug use has permanently rewired their brain. It’s a valid fear because the link between Schedule 1 controlled substances and the onset of psychotic disorders isn't just a myth—it’s a massive area of study in modern psychiatry.
Schizophrenia isn’t something you "get" like a cold. It is a complex, neurodevelopmental condition. However, you can absolutely trigger a psychotic break that looks, acts, and feels exactly like it. In clinical circles, we talk about the "diathesis-stress model." Basically, you might have a genetic "loaded gun," and certain Schedule 1 drugs—like high-potency cannabis or synthetics—can be the finger that pulls the trigger.
The Schedule 1 Connection: What the Research Actually Says
When the DEA classifies something as Schedule 1, they are saying it has no accepted medical use and a high potential for abuse. Think LSD, MDMA, and (federally, at least) marijuana. Now, the relationship between these substances and psychosis is messy. It's not a straight line.
Dr. Robin Murray, a prominent professor of psychiatric research at King's College London, has spent decades documenting how high-potency THC specifically impacts the development of schizophrenia. His work suggests that if you start using high-THC products during your teenage years—when your prefrontal cortex is still basically a construction zone—you are significantly increasing your risk of a psychotic outcome. We aren't talking about the "mellow" weed of the 1970s. We’re talking about 90% THC concentrates that can induce "Schedule 1 how to get schizophrenic" symptoms in people who might have otherwise stayed healthy.
It’s about the dopamine. Almost all drugs of abuse cause a surge in dopamine in the brain's reward system. But in people prone to schizophrenia, this dopamine dysregulation happens in the mesolimbic pathway. When you flood that pathway with synthetic stimulants or heavy hallucinogens, you’re mimicking the exact chemical environment of a schizophrenic brain.
📖 Related: The Cure for the Black Death: Why 14th-Century Doctors Failed and What Actually Works Today
The Role of Genetics
You can't ignore the DNA. Research involving the COMT gene has shown that individuals with a specific variation are much more likely to develop psychosis after using cannabis. If you have this genetic vulnerability, using Schedule 1 substances is essentially playing Russian roulette with your sanity. You might feel fine for months. Then, one day, the "switch" flips. Once that switch is flipped, the symptoms—hallucinations, delusions, disorganized thinking—don't always go away when the drug wears off.
Drug-Induced Psychosis vs. Chronic Schizophrenia
There is a huge distinction that often gets lost in the panic of a bad trip. Drug-induced psychosis is technically a temporary state. You take a substance, you lose touch with reality, and as the substance leaves your system, you return to baseline. But here is the kicker: a study published in The American Journal of Psychiatry found that nearly 32% of people who experienced drug-induced psychosis were later diagnosed with schizophrenia or schizoaffective disorder.
The transition is most common with cannabis (around 47%) and hallucinogens. It’s a terrifying prospect. You think you’re just exploring your consciousness with a Schedule 1 substance, but you’re actually fast-tracking a latent condition.
What Does the Break Look Like?
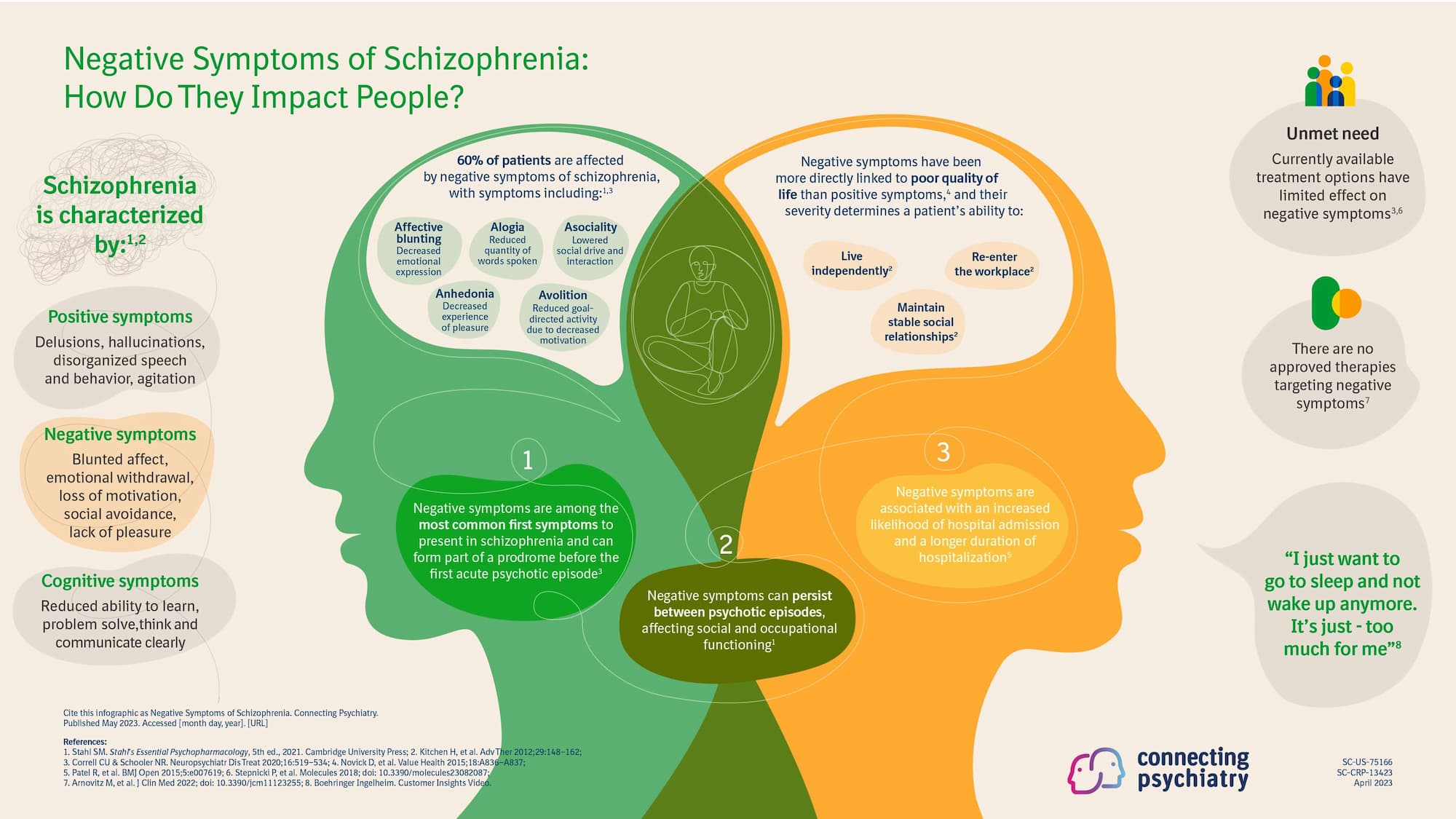
It usually starts small. Ideas of reference. You think the lyrics on the radio are a specific message for you. You start feeling like the "vibe" in the room is sinister for no reason. This is the prodromal phase. If you are looking into schedule 1 how to get schizophrenic because you feel "off," pay attention to those early signs. Social withdrawal, a sudden drop in hygiene, and a strange, flat way of speaking are all massive red flags.
Why Synthetics Are Changing the Game
We have to talk about "Spice" or "K2." These are synthetic cannabinoids often lumped into the Schedule 1 discussion because they are frequently illegal and highly dangerous. Unlike natural THC, which is a partial agonist of the CB1 receptor, these synthetics are full agonists. They hit the brain with the force of a sledgehammer.
I’ve seen cases where a single use of synthetic cannabinoids led to a prolonged psychotic break that required months of stabilization in a locked ward. This isn't just "getting high." This is chemical trauma to the brain. The brain's plasticity is a double-edged sword; it can learn and adapt, but it can also be scarred by intense toxic insults from these substances.
💡 You might also like: High Blood Sugar: What Actually Happens to Your Body in Real-Time
Environmental Triggers and the "Second Hit"
Psychiatry often talks about the "two-hit hypothesis." The first hit is your genetics—something you can’t control. The second hit is an environmental stressor. For many, that second hit is the use of a Schedule 1 drug during a vulnerable period of life.
Is it possible to "get" schizophrenia without drugs? Of course. But the data shows that drugs act as an accelerant. They bring the fire on faster and hotter than it would have occurred naturally. For some, the disorder might have remained "silent" forever if they hadn't introduced heavy psychoactive substances into the mix.
Real Steps Toward Recovery and Prevention
If you are worried that you’ve done permanent damage or if you are seeing symptoms of schizophrenia emerging after drug use, you need to act immediately. Brain health is time-sensitive. The longer a person remains in a state of untreated psychosis, the harder it is to return to their "old self." This is known as the "Duration of Untreated Psychosis" (DUP), and it’s a major predictor of long-term outcomes.
- Total Abstinence is Non-Negotiable. If your brain is showing signs of instability, you cannot put any more psychoactive substances into it. No "just a little weed to calm down." It’s like trying to put out a fire with gasoline.
- Get a Professional Evaluation. You need to see a psychiatrist who specializes in dual diagnosis. They can help determine if what you’re experiencing is a lingering drug effect or the start of a primary psychotic disorder.
- Genetic Testing. While not a perfect tool yet, some companies offer testing for the COMT and AKT1 genes, which can give you a better idea of your personal risk profile regarding substance-induced mental health issues.
- Focus on Neuroprotection. Prioritize sleep, Omega-3 fatty acids (which have some evidence in reducing the transition to psychosis in high-risk individuals), and a stable environment.
- Therapeutic Intervention. Cognitive Behavioral Therapy (CBT) for psychosis is a real thing. It helps people reality-test their thoughts and manage the anxiety that comes with "losing your mind."
Understanding the relationship between Schedule 1 drugs and schizophrenia isn't about scare tactics; it's about informed consent. Your brain is a delicate electrochemical machine. If you’re going to mess with the settings, you need to understand that some changes can't be "undone" with a simple restart.
If you or someone you know is experiencing a break from reality, contact a crisis line or a mental health professional immediately. Early intervention is the single most important factor in maintaining a high quality of life. The path back to stability starts with a clear head and a commitment to protecting your neurological health at all costs.