You’re exhausted. Your brain is ready to shut down, but your legs have other plans. It’s that creepy-crawly, itching, tugging sensation that only seems to show up the second you get under the covers. If you’ve ever felt like you need to kick a hole through your mattress just to find relief, you know exactly how frustrating it is to figure out what helps with restless legs at night.
It’s called Restless Legs Syndrome, or RLS. Most people think it’s just a "fidgety" habit, but for those living with it, it’s a neurological hurdle that ruins sleep and spikes stress. Honestly, it’s maddening.
The medical community often refers to it as Willis-Ekbom Disease. While it sounds fancy, the reality is a lot more primal—your nervous system is essentially sending "go" signals when it should be sending "stop" signals.
The Irony of Iron: Why Your Blood Work Might Be Lying to You
One of the most common things that helps with restless legs at night is addressing an iron deficiency. But here’s the kicker: your "normal" lab results might actually be the problem.
Standard blood tests look at ferritin levels. Most doctors see a ferritin level of 30 or 50 ng/mL and say, "You're fine." However, the Restless Legs Syndrome Foundation and many neurologists suggest that for RLS sufferers, that number needs to be much higher—often above 75 or even 100 ng/mL.
💡 You might also like: Is Tap Water Okay to Drink? The Messy Truth About Your Kitchen Faucet
Why? Because iron is a co-factor for producing dopamine.
Dopamine isn't just about feeling happy; it’s the chemical that regulates smooth muscle movement. When iron is low in the brain (even if it's "okay" in the blood), dopamine production glitches. Your legs start to twitch because the signaling is frayed. If you’re struggling, ask your GP for a full iron panel and specifically look at that ferritin number. Don’t just take a supplement blindly, though, because iron overload is a real risk. It’s a delicate balance.
The Magnesium Myth vs. Reality
Everyone on the internet will tell you to take magnesium. It’s basically the "essential oil" of the RLS world.
Does it work? Sometimes.
📖 Related: The Stanford Prison Experiment Unlocking the Truth: What Most People Get Wrong
Magnesium helps muscles relax and can regulate calcium transport in the nerves. But taking a random pill from the drugstore might just give you a stomach ache. Magnesium oxide, the cheapest version, has terrible bioavailability. If you want to see if magnesium is what helps with your restless legs at night, look for Magnesium Glycinate. It’s easier on the gut and more likely to actually reach your nervous system. Some people swear by Epsom salt baths, which use magnesium sulfate. While the science on skin absorption is a bit shaky, the warm water alone helps desensitize the nerves for a short window, which might be all you need to fall asleep.
The "Dopamine Agonist" Trap
For years, doctors handed out drugs like pramipexole (Mirapex) or ropinirole (Requip) like candy. These are dopamine agonists. They mimic dopamine in the brain and, at first, they feel like a miracle. The twitching stops. You sleep.
Then comes "augmentation."
This is the dark side of RLS treatment. Over time, these meds can actually make the symptoms worse. They start earlier in the day. They spread to your arms. It’s a physiological backfire. Dr. Mark Buchfuhrer, a leading expert at Stanford, has spent years highlighting how many patients are actually suffering more because of the very meds meant to help them. Nowadays, many specialists are moving toward alpha-2-delta ligands—drugs like gabapentin or pregabalin—as the first line of defense because they don't carry the same risk of making the condition spiral.
👉 See also: In the Veins of the Drowning: The Dark Reality of Saltwater vs Freshwater
Habits That Actually Calm the "Creepy Crawlies"
Sometimes the best thing for restless legs isn't a pill. It's weird stuff.
- Weighted Blankets: The deep pressure stimulation can "distract" the nerves. It’s like giving your nervous system a hug so it stops screaming.
- The Freeze/Heat Cycle: Some people find that a freezing cold shower on the legs right before bed resets the sensation. Others need a heating pad. You have to experiment.
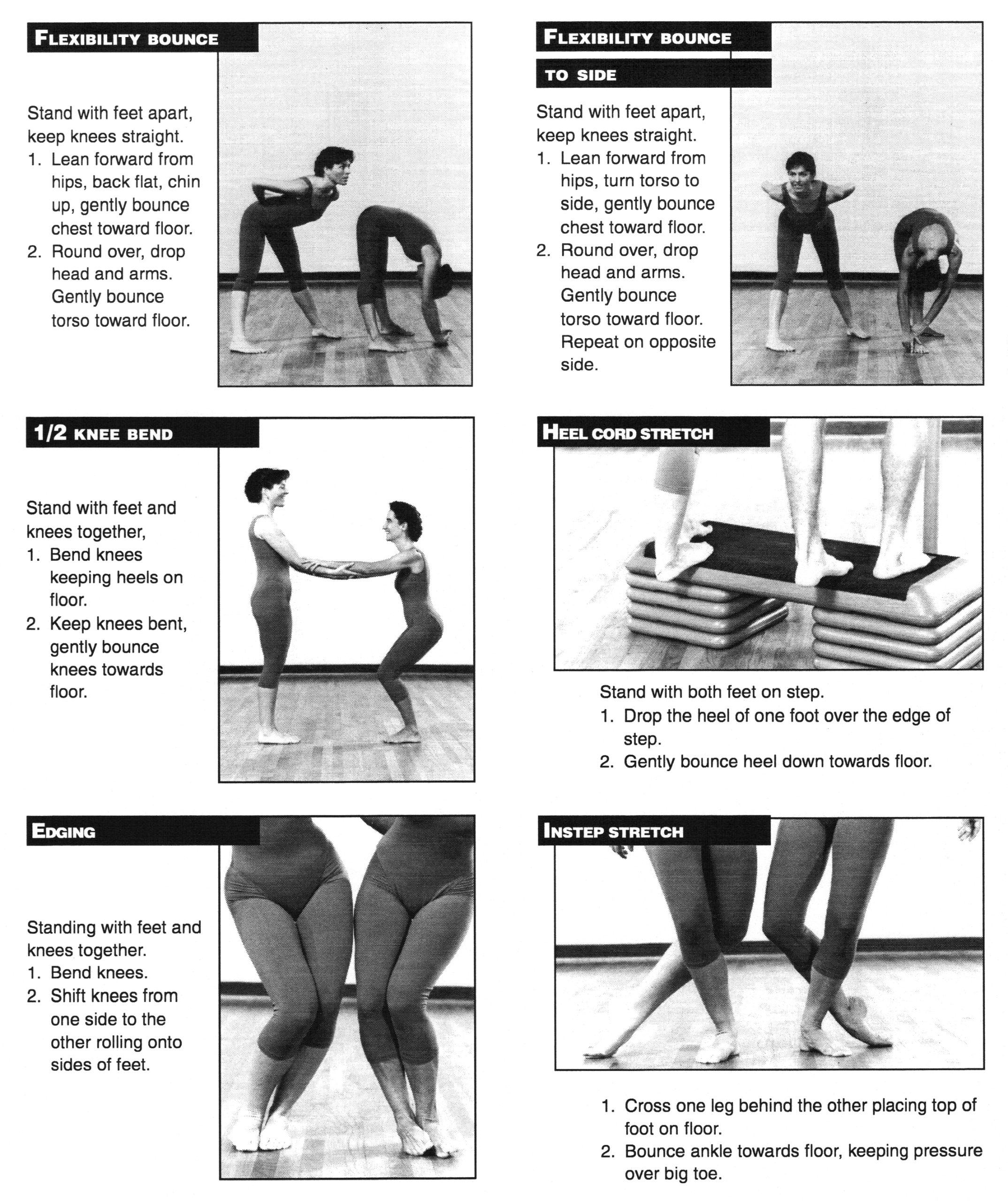
- Vigorous Calf Stretches: Not a light stretch. A deep, lunging calf stretch that almost hurts. This provides a different sensory input that can override the RLS signals for 20 or 30 minutes.
What You’re Drinking is Probably Making it Worse
Caffeine is the obvious villain. But alcohol is the secret assassin. While a glass of wine might help you drift off, it’s a notorious trigger for RLS "rebound" later in the night. The same goes for Benadryl (diphenhydramine). If you have RLS, Benadryl is often gasoline on a fire. Most over-the-counter sleep aids use antihistamines that block dopamine receptors, which is the exact opposite of what an RLS sufferer needs.
The Role of Modern Tech and Vibration
There’s a device called the Relaxis pad—it’s FDA-cleared and basically vibrates at a frequency that competes with the RLS sensations. It’s based on the "Gate Control Theory" of pain. If you provide a constant, non-painful stimulus (vibration), the brain busy-signals the RLS sensations. It’s expensive, and it doesn't work for everyone, but for some, it’s the only way to get four hours of peace.
Actionable Steps to Take Today
If you are staring at the ceiling at 3 AM right now, or if you’re planning for a better night tomorrow, here is the sequence of events that actually moves the needle.
- Check your meds. Go through your cabinet. Are you taking SSRIs for depression? Are you taking sedating antihistamines for allergies? These are massive RLS triggers. Talk to your doctor about alternatives that are "RLS-friendly."
- Get the right blood test. Demand a ferritin check. If it’s under 75, discuss an iron protocol with a professional.
- The "Last Hour" Routine. No sugar, no booze, and no caffeine after 4 PM. In the hour before bed, do 10 minutes of heavy leg stretching followed by a lukewarm bath with two cups of Epsom salts.
- Use Distraction. If the sensations start, don't just lie there and fight them. Get up. Walk. Use a percussion massage gun on your calves for five minutes. It buys you a window of "nerve silence" to try and fall asleep.
- Look into Gabapentinoids. If lifestyle changes fail, skip the old-school dopamine drugs and ask your neurologist about low-dose gabapentin enacarbil. It’s often more stable and has a lower risk of making your life a living hell three months down the line.
The reality is that RLS is a moving target. What works on Monday might not work on Thursday. But by focusing on brain iron levels, avoiding dopamine blockers, and using sensory distraction, most people can find a way to coexist with their twitchy legs without losing their mind.