You’re in the bathroom, you glance down, and there’s a streak of red. Your brain immediately goes to one of two places: "I definitely ate too many spicy wings last night" or "Oh no, I'm dying." Most guys choose the wing theory. They chalk it up to hemorrhoids, a rough workout, or just getting older. But when we talk about rectal cancer symptoms male patients often overlook, that "it’s probably nothing" mindset is exactly what gives the disease a head start.
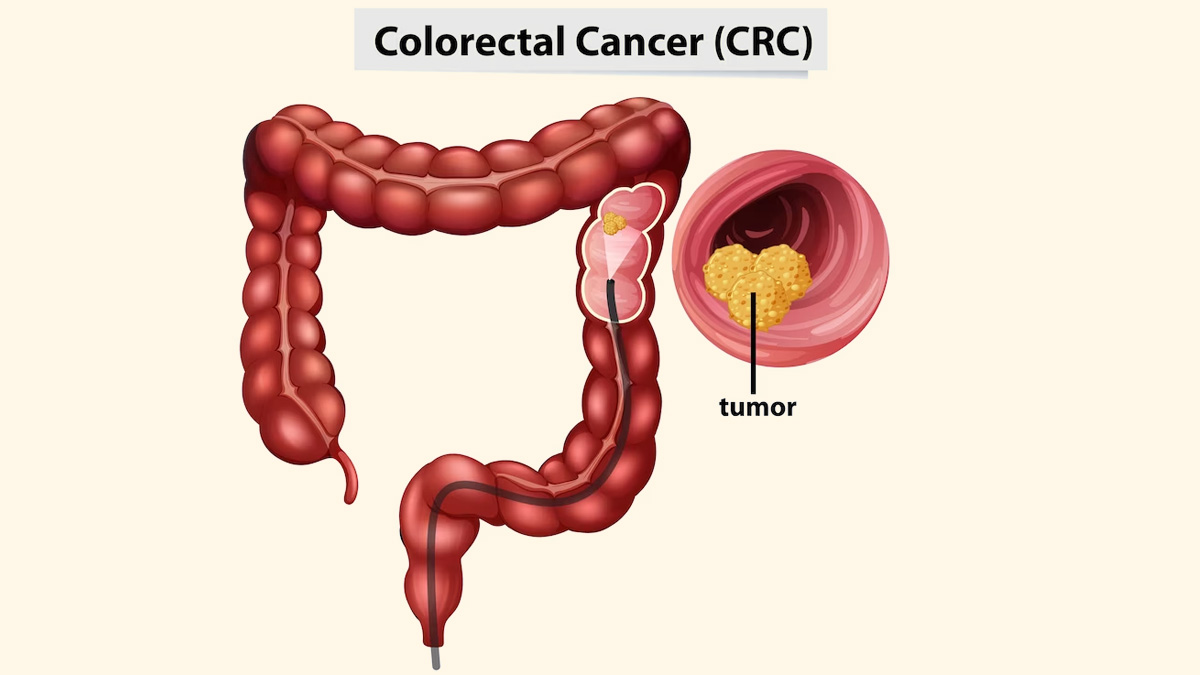
It’s scary. Let's be real. Nobody wants to talk about their rectum. It’s the least "dinner party" topic imaginable. But mortality doesn't care about your embarrassment. Rectal cancer is fundamentally different from colon cancer in how it presents and how it’s treated, even though they’re often lumped together under the "colorectal" umbrella. Because the rectum is the final six inches of the large intestine, the symptoms are often more "mechanical" and immediate than cancers located higher up in the colon.
That Blood Might Not Be Hemorrhoids
Most men assume rectal bleeding is just a flare-up of hemorrhoids. It’s a logical guess. About 75% of people will have hemorrhoids at some point. But here’s the kicker: you can have both. Having a known history of hemorrhoids doesn't mean you're immune to a tumor growing right next to them.
The blood associated with rectal cancer is often dark, almost maroon, or mixed thoroughly into the stool. However, because the rectum is so close to the "exit," the blood can also be bright red. Dr. Kimmie Ng from the Dana-Farber Cancer Institute has noted a disturbing rise in young-onset colorectal cancer, where rectal bleeding is the most common early warning sign. If you see blood, you don't guess. You get a scope.
It isn't just about the color of the blood. It’s about the consistency. If your stool looks like it’s been painted with a brush, or if you notice "occult" blood—which you can’t see but shows up on a FIT test—that’s a massive red flag.
The "Pencil Stool" Phenomenon
Ever heard of pencil-thin stools? It sounds like a weird medical myth, but it’s a very real rectal cancer symptom male patients should watch for. Think about the physics of it. Your rectum is a storage tank. As a tumor grows along the wall of the rectum, it narrows the passage. The stool has to squeeze through a smaller and smaller opening.
✨ Don't miss: Why Sometimes You Just Need a Hug: The Real Science of Physical Touch
The result? Stool that is consistently thin, narrow, or ribbon-like.
If this happens once after a night of heavy drinking or a weird diet change, fine. But if your "new normal" looks like a No. 2 pencil, your anatomy is being compressed by something. Often, that "something" is a mass.
Tenesmus: The Feeling That You're Never "Done"
There is a specific, frustrating sensation called tenesmus. It’s that nagging feeling that you still need to go, even though you just finished. You sit there, you strain, and nothing happens. This happens because a tumor in the rectum mimics the presence of stool. Your nerves are sending signals to your brain saying, "Hey, there's something in here that needs to get out!" except it’s a solid mass, not waste.
It’s incredibly annoying. It ruins your day. It makes you stay near a bathroom constantly.
Guys often mistake this for constipation or IBS. They take Laxatives. They eat more fiber. But if the issue is a physical blockage in the rectal vault, all the Metamucil in the world won't move it. You're basically trying to push a car through a doorway that's been partially boarded up.
🔗 Read more: Can I overdose on vitamin d? The reality of supplement toxicity
Changes in Bowel Habits That Last
We all have "off" days. But if your bathroom routine has fundamentally shifted for more than two weeks, that’s the clinical threshold for concern. This might look like:
- Alternating between sudden diarrhea and intense constipation.
- A feeling of fullness in the lower abdomen that doesn't go away.
- Increased gas pain or cramping that feels "lower" than usual.
Why Are Men Getting This Younger?
We used to think of this as an "old man's disease." Not anymore. The American Cancer Society recently reported that the proportion of colorectal cancer cases in people under age 55 doubled between 1995 and 2019. This is why the screening age was dropped from 50 to 45.
Diet plays a role. Processed meats, low fiber, and sedentary lifestyles are the usual suspects. But there’s also something happening with the gut microbiome that researchers are still trying to pin down. For men specifically, there's a stubborn tendency to "tough it out." We wait until the pain is unbearable or the bleeding is constant before seeing a doctor. By then, the cancer might have moved through the rectal wall into the lymph nodes or nearby organs like the prostate or bladder.
The Fatigue and Weight Loss Factor
Unexplained weight loss is rarely the first sign of rectal cancer, but it’s a serious one. If you’re losing weight without trying—meaning you haven’t started a New Year’s resolution or joined a CrossFit gym—your body is burning calories at an accelerated rate to fight an internal battle.
Then there’s the exhaustion. Not "I stayed up too late" tired. More like "I slept 9 hours and I still feel like I ran a marathon" tired. This is often caused by chronic, microscopic blood loss that leads to anemia. You’re literally losing iron every time you go to the bathroom, even if you don't see the blood.
💡 You might also like: What Does DM Mean in a Cough Syrup: The Truth About Dextromethorphan
Screening: The Part Everyone Dreads (But Shouldn't)
The "Gold Standard" is the colonoscopy. Yeah, the prep sucks. Drinking a gallon of salty Gatorade-tasting liquid isn't anyone's idea of a Friday night. But the actual procedure? You’re asleep. You wake up, you have some of the best farts of your life because of the air they pump in, and you’re done.
More importantly, a colonoscopy is one of the only "preventative" cancer tests. Most tests just find cancer. A colonoscopy can prevent it. If the doctor sees a polyp (a precancerous growth) in your rectum, they snip it out right then and there. Boom. Potential cancer gone before it ever started.
If you’re absolutely terrified of the scope, there are stool-based tests like Cologuard or FIT. They’re better than nothing, but they aren't perfect. They look for DNA markers or blood. If they come back positive, guess what? You’re getting a colonoscopy anyway.
What to Do If You Notice Symptoms
Don't panic. Panic helps nobody. But don't ignore it either. If you have any of the rectal cancer symptoms male biology presents—especially the bleeding or the "pencil stools"—you need to book an appointment with a gastroenterologist.
When you talk to the doctor, be specific. Don't say "My stomach hurts." Say "My stools have changed shape" or "I am seeing red blood in the bowl three times a week." Doctors hear this stuff all day. They don't care about the "gross" factor. They care about the stage of the tumor.
Actionable Next Steps
- Track your habits for 7 days. Note the frequency, consistency, and any presence of blood. Having a "log" makes your doctor's visit 10x more productive.
- Check your family history. Did your dad have polyps? Did your uncle have "colon issues"? Genetics are a massive factor in rectal cancer risk.
- Audit your diet. Start hitting the 30g of fiber a day mark. It’s not just for old people; it’s literal fuel for a healthy gut lining.
- Demand a digital rectal exam (DRE). It’s quick, it’s a bit uncomfortable, but a doctor can often feel a low-lying rectal tumor with a simple manual exam.
- Stop the "Hemorrhoid Excuse." If you use an over-the-counter cream and the bleeding doesn't stop within a week, it’s not just a hemorrhoid. Get a professional opinion.
Early-stage rectal cancer has a very high survival rate—over 90% if caught early. The survival rate drops significantly if it spreads. The difference between a minor surgery and a life-altering battle is often just the three months you spent "waiting for it to go away." Listen to your gut. Literally.