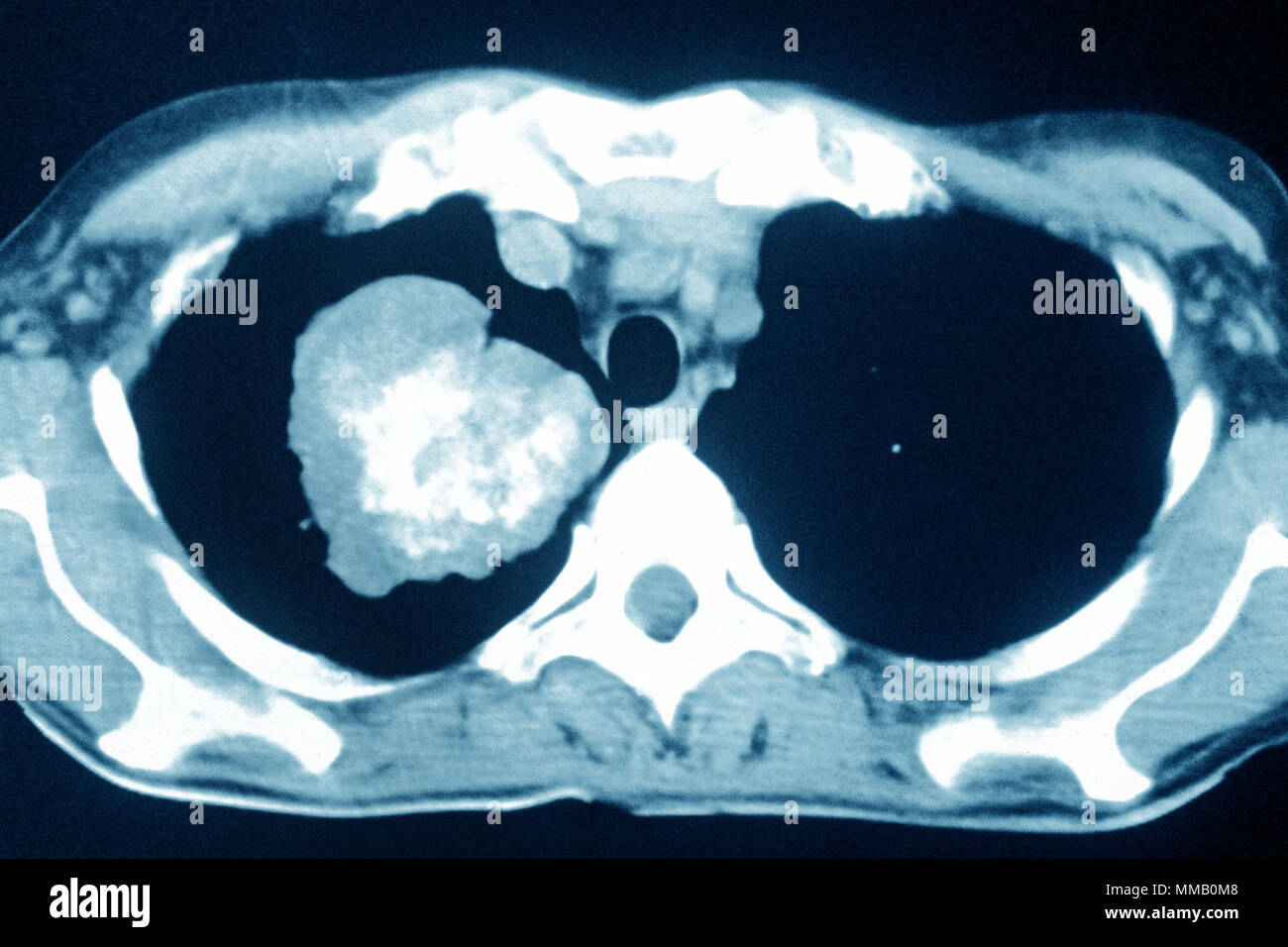
You’re sitting in a cold exam room, and the doctor swivels the monitor toward you. On the screen is a grainy, black-and-white cross-section of your chest. It looks like a Rorschach test made of static and shadows. These lung cancer ct scan images are the gold standard for finding trouble early, but honestly, looking at them without a medical degree is a recipe for a panic attack.
Everything looks like a spot. Every shadow feels like a threat.
But here is the thing: your lungs are messy. They are filled with blood vessels, lymph nodes, and scars from that bout of bronchitis you had three years ago. Radiologists spend a decade learning how to tell the difference between a harmless "nothing" and a malignant "something." If you've ever squinted at your own scan trying to play detective, you know how quickly your mind jumps to the worst-case scenario. It's human nature.
What those shadows on lung cancer ct scan images actually mean
When a radiologist looks at your scan, they aren't just looking for a "blob." They are looking at morphology. That's a fancy way of saying they look at the shape and the edges.
Imagine a pebble. If the edges are smooth and round, like a marble, that’s often a good sign. Doctors call these "well-circumscribed." Many benign nodules—non-cancerous growths—look like this. They might be hamartomas (a mix of normal tissues) or old granulomas from a fungal infection like histoplasmosis, which is super common if you live in the Ohio River Valley.
Now, imagine a tumbleweed.
If the growth has jagged, "spiculated" edges that reach out into the lung tissue like tiny tentacles, that’s when doctors get worried. This "spiculation" is a classic hallmark often seen in lung cancer ct scan images. It suggests the growth is invading the surrounding area rather than just sitting there. But even then, it's not a 100% guarantee of cancer. Inflammation can mimic that look too.
Then there is the "ground-glass opacity" or GGO. This sounds like a trendy interior design term, but in radiology, it describes a hazy area that doesn't quite hide the underlying bronchial structures. It looks like a smudge on the lens. These can be tricky. They might be a simple infection, or they could be a slow-growing type of cancer called adenocarcinoma in situ.
The weight of the "Nodule"
A single nodule is just a dot. Radiologists measure them in millimeters. If it’s under 6 millimeters and you aren't a heavy smoker, the Fleischner Society guidelines—which are basically the "bible" for how doctors manage these findings—often suggest doing... absolutely nothing. Or maybe just one follow-up scan in a year.
Size matters. A lot.
A 30-millimeter growth isn't a nodule anymore; it's a "mass." The statistical likelihood of a mass being malignant is significantly higher than a tiny 4mm speck. But even a large mass can be an abscess or a big wad of scar tissue. This is why "watchful waiting" is the most frustrating, yet common, part of the process. If a spot doesn't grow over two years of serial lung cancer ct scan images, it's almost certainly benign. Cancer is many things, but it is rarely patient. It wants to grow.
Why "AI" is actually helping (and why it's not replacing your doctor)
You’ve probably heard the hype about AI in medicine. In the world of thoracic imaging, it's actually becoming a reality. Software like ClearRead CT or various FDA-cleared algorithms are now being used to "pre-read" scans.
💡 You might also like: Why Chocolate Protein Ice Cream is Actually the Best Way to Hit Your Macros
They don't make the diagnosis.
Instead, they act like a second set of eyes that never gets tired. A radiologist might look at 100 scans a day. By 4:00 PM, eye fatigue is real. AI helps by circling "areas of interest" so the human doctor can give them a closer look. It's great at detecting "subsolid" nodules that are faint and easy to miss against the background of the ribs or heart.
But don't expect a computer to give you the final word. A computer might flag a scar as a tumor because it doesn't know you had a chest injury in 1998. The human doctor integrates your history—your smoking status, your family tree, your cough—with what's on the screen.
The "Screening" vs. "Diagnostic" Divide
Not all CT scans are created equal. This is a huge point of confusion.
If you are a high-risk individual (usually aged 50 to 80 with a heavy smoking history), you might get a Low-Dose CT (LDCT). This is a screening tool. It uses a much lower dose of radiation—about 1.5 millisieverts compared to the 7 or 8 millisieverts in a standard scan. It's grainy. It’s not meant to see every tiny detail; it’s meant to find the "big" stuff before it becomes a problem.
A diagnostic CT is different. This often involves contrast—that dye they inject into your veins that makes you feel like you've suddenly peed your pants (you haven't, it's just the heat). Contrast helps the doctor see blood flow. Since tumors are "blood-hungry," they often "light up" or enhance when the dye hits them. If your screening scan shows something suspicious, the next step is usually the diagnostic scan with contrast to get the full picture.
Location, Location, Location
Where the spot is matters as much as what it looks like.
Lung cancer has "favorite" spots. Squamous cell carcinomas tend to hang out in the center of the chest, near the big airways (the bronchi). Adenocarcinomas are more like suburbanites; they prefer the outer edges of the lungs. If a radiologist sees a spiculated mass in the upper lobes, their "suspicion index" goes way up. Why? Because the upper lobes are where cigarette smoke tends to concentrate, making it the prime real estate for malignancy.
If you see mention of "hilar lymphadenopathy" on your report, don't ignore it. The hilum is the "root" of the lung where the vessels enter. When lymph nodes there get big, it could mean the cancer is trying to travel. Or, again, it could just mean you have a sinus infection. Nuance is everything.
Misconceptions that lead to unnecessary "Scanxiety"
"If it's on my scan, it's cancer."
Wrong.
Data from the National Lung Screening Trial showed that about 24% of screening scans were "positive" for something, but 96% of those findings turned out to be benign. That is a massive gap.
"I've never smoked, so this spot must be a mistake."
Also wrong.
While smoking is the primary driver, 10-20% of lung cancers happen in "never-smokers." These often show up as those "ground-glass" spots we talked about earlier.
"The radiation from the scan will give me cancer."
The risk is incredibly low. A single LDCT scan is roughly equivalent to the amount of background radiation you get from just living on Earth for six months. When you weigh that against the risk of an undiagnosed tumor, the math isn't even close.
What to do if your report looks scary
First, take a breath. Seriously.
If you read your own radiology report through a patient portal before the doctor calls (we all do it), you’re going to see words like "opacity," "attenuation," and "non-calcified." Don't Google every single word. You will end up convinced you have two weeks to live.
Look for the "Impression" section at the bottom. That is where the radiologist summarizes the technical jargon into a "What do we do now?" plan. They will usually assign a "Lung-RADS" score from 1 to 4.
- Lung-RADS 1 or 2: You're good. See you next year.
- Lung-RADS 3: Probably fine, but let's check again in 6 months just to be sure.
- Lung-RADS 4: We need more tests. This could be a biopsy, a PET scan, or a consultation with a pulmonologist.
Actionable Next Steps
If you are looking at your lung cancer ct scan images or reading a report, here is how you handle the next 48 hours:
- Ask for the Lung-RADS score. If it’s not in the report, ask your doctor. It’s the most standardized way to understand your risk level.
- Request a comparison. The most valuable thing in radiology isn't a single image; it's the change between images. If you had a chest X-ray or CT five years ago for a rib injury, make sure the radiologist has those old files. If the spot was there in 2019 and hasn't changed, you can stop worrying.
- Check your "calcification" status. If the report says a nodule is "diffusely calcified," that's usually code for "this is an old, dead scar." Calcium is generally a sign of a benign process in the lungs.
- Prepare for a PET scan. If the CT is suspicious, the PET scan is usually next. It uses a radioactive sugar tracer. Since cancer cells are "sugar hogs," they glow bright on a PET scan. If a spot is "PET-avid," the suspicion for cancer goes up significantly.
- Quit smoking today. It sounds cliché, but if a spot is found to be early-stage cancer, your outcomes are significantly better if your lungs aren't actively fighting smoke during treatment.
The reality of lung cancer ct scan images is that they are a tool, not a crystal ball. They provide the map, but the biopsy provides the destination. If your doctor suggests "watchful waiting," it's not because they are ignoring you; it's because the science shows that for tiny spots, waiting to see if they move is safer than sticking a needle into a healthy lung.