You’re standing in front of the bathroom mirror. You see it. That weird, slightly raised bump on your shoulder that wasn't there last month. Your first instinct is to grab your phone and start scrolling. Suddenly, you're staring at a types of skin lesions chart full of terrifying medical jargon and high-resolution photos that all look suspiciously like a death sentence. It’s overwhelming. Honestly, most people just end up more confused than they were before they started looking.
Skin isn't just a wrapper. It’s your largest organ. It reacts to everything—the sun, your gut health, that cheap laundry detergent you bought on sale, and your genetics. When something pops up on the surface, doctors call it a "lesion." That sounds scary. It’s not necessarily. A lesion is basically just any part of the skin that has an abnormal growth or appearance compared to the skin around it. It could be a freckle. It could be a blister. It could be something that needs a surgeon.
Understanding what you’re looking at requires a bit of nuance. You can’t just match a picture to your arm and call it a day. You have to understand the "alphabet" of dermatology.
Primary vs. Secondary: The basic split
Most charts break things down into primary and secondary categories. Think of primary lesions as the "original" version. This is what appears first. If you leave it alone, or if you scratch it, pop it, or it starts to heal, it becomes a secondary lesion.
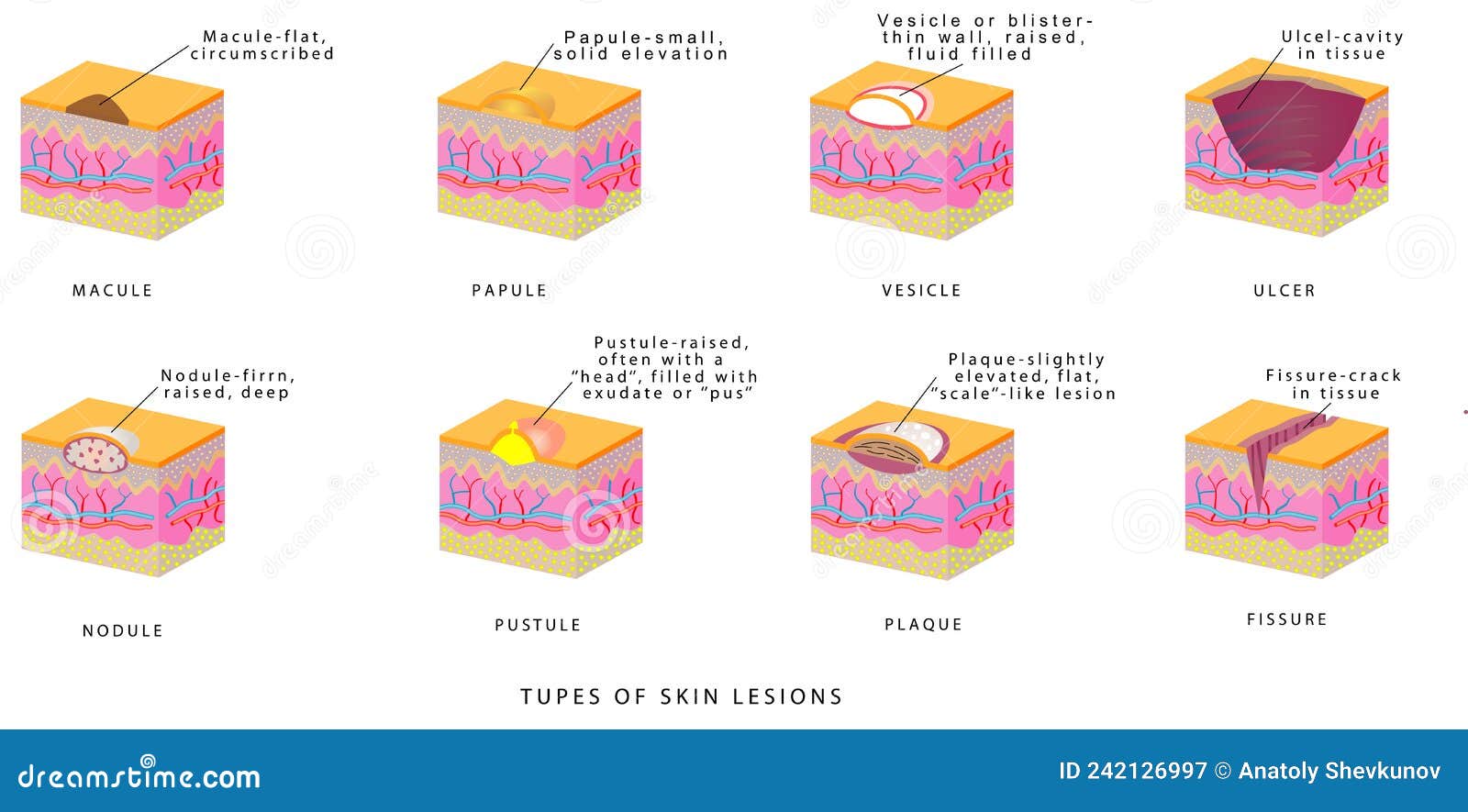
Let's talk about the flat stuff first. If you have a flat spot that’s less than 1 centimeter, doctors call it a macule. Think of a freckle or a flat mole. If it’s bigger than a centimeter, it’s a patch. Vitiligo is a classic example of a patch. These don't have texture. If you closed your eyes and ran your finger over them, you wouldn't feel a thing.
Then things get bumpy.
A papule is a small, raised bump. It’s solid. No fluid. If that bump gets bigger and wider, like a plateau on your skin, it’s a plaque. This is the hallmark of psoriasis. You might also see nodules, which are deeper and firmer. If you’ve ever had a deep, painful "underground" zit that never comes to a head, that’s a nodule.
The wet and the weary: Fluid-filled lesions
Bubbles on the skin are a different beast. A vesicle is a tiny, fluid-filled blister, like what you see with chickenpox or shingles. If it’s huge—think a bad friction blister from new shoes—it’s a bulla. If that blister is filled with pus instead of clear fluid, it’s a pustule. Acne is the most famous version of this.
💡 You might also like: Resistance Bands Workout: Why Your Gym Memberships Are Feeling Extra Expensive Lately
But here is where a types of skin lesions chart gets complicated. What happens when these things change?
Secondary lesions are the "aftermath." When a pustule pops and dries, it forms a crust (a scab). If the skin thins out and looks like tissue paper, that’s atrophy. If you scratch a spot until the top layer of skin is gone, you’ve created an excoriation. These aren't the original problem, but they are what the doctor sees when you finally make an appointment three weeks later.
Why color and border matter more than size
People obsess over size. "It's so big!" they say. Honestly? The color and the edges are usually way more telling.
Dermatologists like Dr. Sandra Lee (yes, the one from TV) and researchers at the American Academy of Dermatology often point to the "ABCDE" rule for a reason. While that's specifically for melanoma, the logic applies to most items on a types of skin lesions chart.
- Asymmetry: If you drew a line down the middle, do the halves match?
- Border: Are the edges blurry, jagged, or notched?
- Color: Is it one shade of brown, or does it look like a tie-dye of black, blue, and red?
- Diameter: Is it bigger than a pencil eraser?
- Evolving: This is the big one. Is it changing?
A lesion that stays the same for ten years is rarely a crisis. A lesion that changes in three weeks is a red flag. Evolution is the most important metric.
The common culprits you’ll see on any chart
You’ll likely encounter a few specific names over and over again. These are the "usual suspects."
Actinic Keratosis (AK)
These feel like sandpaper. Usually, you feel them before you see them. They’re precancerous, caused by years of sun damage. They often show up on the scalp, ears, or backs of hands. If you ignore them, they can turn into squamous cell carcinoma.
📖 Related: Core Fitness Adjustable Dumbbell Weight Set: Why These Specific Weights Are Still Topping the Charts
Seborrheic Keratosis
These look terrifying but are totally harmless. They’re often called "barnacles of aging." They look like someone melted a brown candle and dripped it on your skin, or like a mole that was "stuck on" with glue. They can be itchy, but they aren't cancerous.
Cherry Angiomas
Small, bright red bumps. They look like a tiny drop of blood. They’re just clusters of blood vessels. Almost everyone gets them as they get older. They’re benign.
Basal Cell Carcinoma (BCC)
The most common skin cancer. It often looks like a pearly, shiny bump or a sore that bleeds, scabs over, and then refuses to heal. It grows slowly. It rarely spreads to other parts of the body, but it can eat into the tissue where it sits.
The danger of "Dr. Google" and DIY diagnosis
It is so easy to look at a types of skin lesions chart and convince yourself you have something rare. Or, worse, convince yourself that a dangerous spot is "just a mole."
The human eye is remarkably bad at detecting subtle variations in pigment depth. Dermatologists use a tool called a dermatoscope. It’s basically a high-powered magnifying glass with polarized light that lets them see under the top layer of skin. You can't do that with a smartphone camera and a bathroom light.
There’s also the issue of skin tone. Historically, medical charts and textbooks were heavily biased toward white skin. This is a massive problem. A lesion that looks red on fair skin might look purple, grey, or dark brown on deeper skin tones. This leads to misdiagnosis and delayed treatment for People of Color. If you are looking at a chart that only shows one skin type, find a better chart. Resources like "VisualDx" or "Mind the Gap" are trying to fix this disparity by showing how lesions manifest across all ethnicities.
When to actually worry
Stop panicking. Start observing.
👉 See also: Why Doing Leg Lifts on a Pull Up Bar is Harder Than You Think
The "Ugly Duckling" sign is a real clinical concept. If you have twenty moles on your back and nineteen of them look similar, but one looks like a weirdo—that’s the one to get checked. It doesn't matter if it fits the "perfect" description of a cancer on a types of skin lesions chart. If it doesn't belong with the others, it's an outlier.
Also, look for the "symptomatic" signs.
Does it itch constantly?
Does it bleed when you brush it with a towel?
Does it hurt?
Healthy moles and skin tags generally don't hurt or bleed spontaneously.
Actionable steps for your skin health
Instead of just staring at charts, take these concrete steps to manage your skin health properly.
1. Perform a monthly skin self-exam
Do it on the first of the month. Use a full-length mirror and a hand mirror. Check your scalp, the soles of your feet, and between your toes. Yes, you can get skin cancer where the sun doesn't shine.
2. Create a "Skin Map"
Take photos of any spots you’re worried about. Put a ruler or a coin next to the lesion for scale. Save these in a specific folder on your phone. In three months, take another photo. Compare them side-by-side. This is the only way to objectively track "evolution."
3. Use the right terminology with your doctor
When you call for an appointment, don't just say "I have a bump." Say, "I have a pigmented lesion on my thigh that has changed color and has irregular borders." This helps the triage nurse understand the urgency.
4. Don't DIY remove anything
There are "mole removal pens" and "wart freezers" sold online. Do not use them on a lesion you haven't had identified by a professional. If you "freeze off" a melanoma, you haven't cured it; you've just removed the visible part while the roots continue to grow deeper into your bloodstream.
5. Get a professional baseline
If you’re over 30, see a dermatologist for a full-body skin check once. They will tell you which of your spots are "normal" for you. Once you have a baseline, it’s much easier to spot the newcomers.
Understanding the different types of skin lesions is about literacy, not self-surgery. Use the charts as a tool to help you describe what you see, but let the experts handle the "what it is" part. Skin health is a long game. Be patient with the process, but be aggressive with the observation. Your future self will thank you for being the person who noticed that "tiny little change" before it became a big problem.