If you've ever felt like a number in a giant medical machine, you know the frustration of being handed a prescription and a "see ya in six months" wave. It's exhausting. For many dealing with chronic lung issues, the search for something more integrated often leads them to Pulmonary Associates Wellness Way.
Breathing isn't just about lungs. Honestly, it's about everything. Your heart, your stress levels, what you ate for breakfast, and even how you slept last night all collide in that one single breath.
Most people think pulmonary care is just inhalers and oxygen tanks. That's a mistake. Pulmonary Associates has built a reputation on the idea that "wellness" isn't a buzzword; it’s a logistical necessity for people with COPD, asthma, or pulmonary fibrosis.
Why the Wellness Way Approach Actually Matters
Typical healthcare is reactive. You cough, they treat the cough. But the Pulmonary Associates Wellness Way methodology tries to flip that script. It’s basically about looking at the patient as a whole human being who has to live a life, not just a set of lungs in a waiting room.
Think about it this way. If you have severe asthma, but your diet is triggering inflammation and your house is full of dust, an inhaler is just a Band-Aid. You’re fighting a losing battle. The "Wellness Way" concept—often seen in integrated clinics like those in Las Vegas or across various regional Pulmonary Associates groups—revolves around the pillars of pulmonary rehabilitation, nutritional guidance, and aggressive diagnostic monitoring.
It’s about the "how." How do you walk to the mailbox without getting winded? How do you manage the anxiety that hits when your chest feels tight?
Breaking Down the Diagnostic Engine
You can't fix what you haven't measured. This is where things get technical, but stay with me. Real pulmonary experts don't just guess; they use PFTs (Pulmonary Function Tests).
These tests are the bread and butter of the Pulmonary Associates Wellness Way. They measure $FEV_1$ (Forced Expiratory Volume in 1 second) and $FVC$ (Forced Vital Capacity). When a doctor looks at the ratio of these two numbers, they aren't just looking at a chart. They are seeing the literal elasticity of your lung tissue.
Many patients find the "Body Box" (plethysmography) intimidating. It's a clear booth where you sit and breathe into a tube. It feels weird. Kinda like being in a very small, very quiet phone booth from the 80s. But it provides the most accurate data on total lung capacity. Without this data, "wellness" is just a guess.
💡 You might also like: Can I overdose on vitamin d? The reality of supplement toxicity
The Role of Pulmonary Rehabilitation
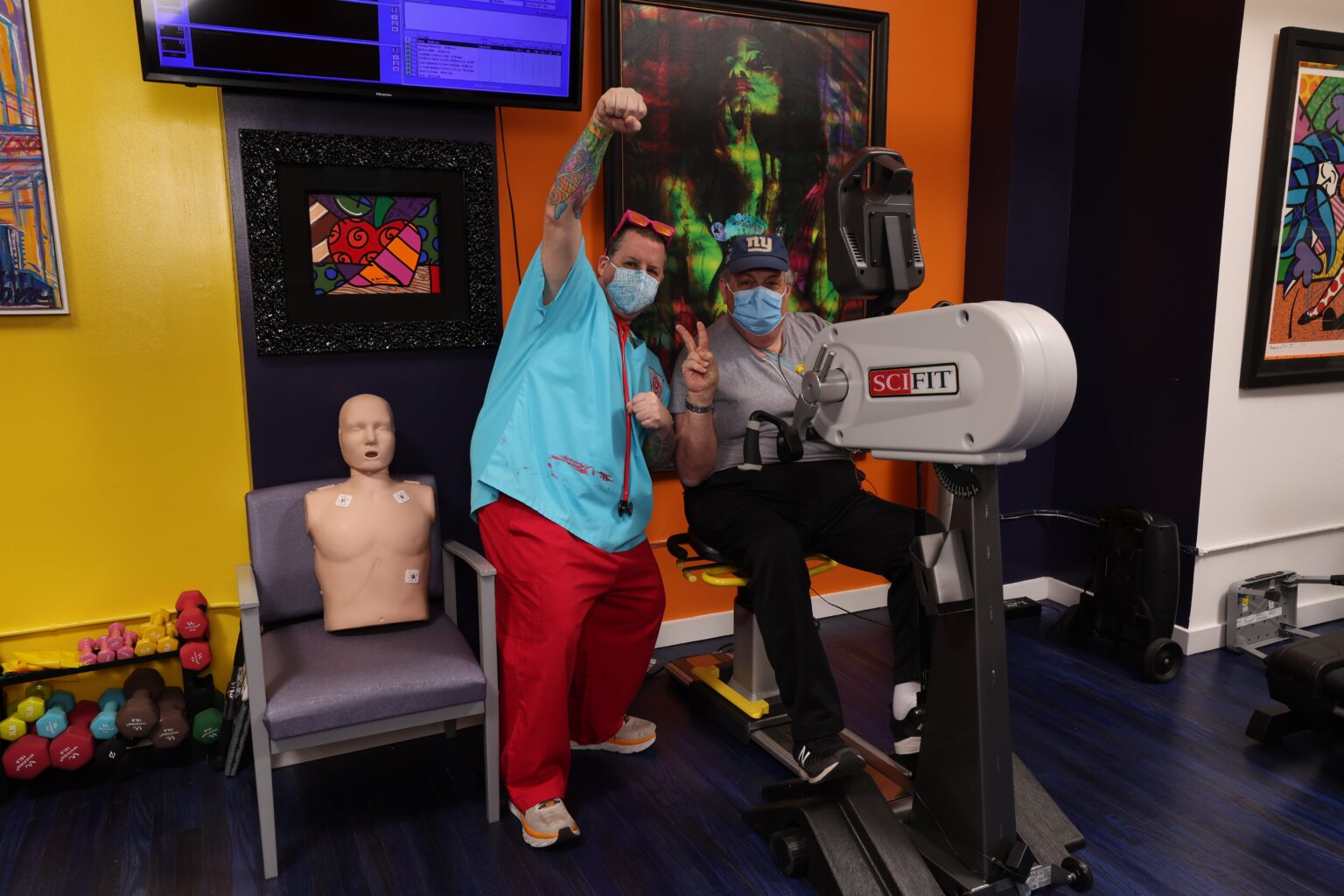
If you ask anyone who has gone through a structured program, they'll tell you: rehab is hard. It's not a spa day. Pulmonary rehabilitation is a supervised exercise program tailored specifically for people with chronic lung disease.
At a facility following the Pulmonary Associates Wellness Way model, this usually involves:
- Monitored Exercise: You’re on a treadmill or a stationary bike while a nurse or therapist watches your oxygen saturation ($SpO_2$) and heart rate. If your oxygen drops below 88%, they stop you. They adjust. They teach you how to push without being dangerous.
- Breathing Retraining: Pursed-lip breathing sounds simple. It is. But doing it correctly under stress is a different story. It creates back-pressure in the airways, keeping them open longer so you can get more air out.
- Education: Understanding why your lungs feel like they’re "trapped" in your chest helps reduce the panic. Panic makes shortness of breath worse. It’s a vicious cycle.
Nutrition: The Fuel for the Fire
Did you know that digestion requires oxygen? For a healthy person, it's no big deal. For someone with advanced lung disease, eating a huge meal can actually make it harder to breathe. This is a nuance many general practitioners miss, but it's a staple of the Pulmonary Associates Wellness Way.
Carbohydrates produce more carbon dioxide ($CO_2$) when metabolized compared to fats. If your lungs are struggling to clear $CO_2$, a high-carb diet can literally make you feel more short of breath. Experts often recommend a "pulmonary diet" that is higher in healthy fats and lower in simple sugars.
Small, frequent meals are the move. If you fill your stomach too much, it pushes against your diaphragm. Your diaphragm needs room to move down so your lungs can expand. If there’s a giant plate of pasta in the way, you’re going to struggle.
The Mental Health Component Nobody Talks About
There is a massive link between lung disease and clinical anxiety. It makes sense. If you feel like you can’t breathe, your brain goes into "survival mode." This triggers cortisol and adrenaline. Your heart rate spikes. You breathe faster and shallower.
The Pulmonary Associates Wellness Way often incorporates behavioral health. Sometimes, the best thing for a pulmonary patient isn't another pill—it's learning how to manage the "air hunger" panic.
Dr. Richard Casaburi, a renowned expert in pulmonary rehab, has long advocated for the psychological benefits of group settings. When you see someone else with an oxygen tank working out and living their life, the "sick" identity starts to fade. You realize you’re a person who has a condition, not a person who is a condition.
📖 Related: What Does DM Mean in a Cough Syrup: The Truth About Dextromethorphan
Sleep and the Pulmonary Connection
You can’t talk about wellness without talking about the night. Sleep apnea isn't just about snoring. It’s a systemic stressor. If your oxygen levels are tanking while you sleep, your heart is working overtime.
Many patients at Pulmonary Associates clinics undergo sleep studies. Using a CPAP or BiPAP machine isn't just about stopping the snoring; it’s about giving your lungs and heart a rest so they can function during the day. It’s all connected. You can’t have "wellness" on four hours of fragmented, low-oxygen sleep.
What People Get Wrong About Pulmonary Care
There’s this myth that if you have lung disease, you should just "take it easy." That’s actually the worst thing you can do. It leads to deconditioning. Your muscles get weaker, so they need more oxygen to move. Because they need more oxygen, your lungs have to work harder.
The Pulmonary Associates Wellness Way pushes back against this. The goal is to get you as active as possible within the limits of your physiology.
Another misconception? That it’s only for "smokers." While smoking is a huge factor in COPD, plenty of patients have genetic conditions like Alpha-1 Antitrypsin Deficiency, or environmental scarring from years of working in construction or around chemicals. Wellness doesn't judge the cause; it focuses on the current state of the tissue.
Making the "Wellness Way" Practical
So, how do you actually use this information? It's not just about finding a specific office; it's about adopting the mindset.
First, get a pulse oximeter. They are cheap. Knowing your baseline is vital. If you’re feeling "off," check the number. If you’re at 95%, your brain might just be anxious. If you’re at 89%, you need to use your rescue techniques.
Second, look at your indoor air quality. HEPA filters are not a luxury for pulmonary patients. They are essential equipment.
👉 See also: Creatine Explained: What Most People Get Wrong About the World's Most Popular Supplement
Third, movement is medicine. Even if it’s just walking from the couch to the kitchen and back five times a day. Build the "muscle" of breathing.
Evidence-Based Results
Studies published in journals like The Lancet and CHEST consistently show that integrated pulmonary care—the kind championed by the Pulmonary Associates Wellness Way—reduces hospital readmissions. When patients understand their triggers and their medications, they don't end up in the ER every time they get a cold.
It’s about self-management. The most successful patients are the ones who treat their lung health like a job. They track their peak flow, they attend their rehab sessions, and they don't skip the "boring" stuff like vaccinations (flu, pneumonia, and COVID-19 are all major risks for this population).
Actionable Steps for Better Lung Health
If you are looking to integrate the Pulmonary Associates Wellness Way into your own life or the life of a loved one, start with these specific moves:
- Request a Full PFT: Don't settle for just a handheld spirometry test at a primary care office. Get the full workup in a plethysmography booth to find your True Total Lung Capacity.
- Audit Your Diet: Switch to a "pulmonary-friendly" eating schedule. Five small meals. Higher protein and healthy fats (avocado, nuts) and lower refined sugars to keep $CO_2$ production down.
- Master the Diaphragm: Practice diaphragmatic breathing (belly breathing) for 10 minutes every morning. Most people breathe with their shoulders and neck when they are stressed. That’s inefficient.
- Check Your Meds: Ensure you are using your inhaler correctly. Statistics show up to 70% of patients don't use the proper technique, meaning the medicine hits the back of the throat instead of the deep lung tissue. Ask for a "spacer" if you use an MDI (metered-dose inhaler).
- Hydration is Key: Thin mucus is easier to cough up than thick mucus. Drink enough water to keep those secretions moving.
Living with a pulmonary condition is a marathon, not a sprint. The Pulmonary Associates Wellness Way isn't a magic cure, but it is a roadmap. It shifts the focus from "surviving" to "optimizing." By combining high-tech diagnostics with "low-tech" lifestyle changes like diet and movement, you can reclaim a significant amount of your quality of life.
Focus on the numbers, but don't forget the feeling of the wind on your face. That’s what the wellness journey is actually for.
Key Resources & References:
- Global Initiative for Chronic Obstructive Lung Disease (GOLD) Guidelines.
- American Lung Association: "Benefits of Pulmonary Rehab."
- Journal of Clinical Sleep Medicine: "The Interaction of COPD and Sleep Apnea."
Implementation Guide
To move forward, schedule a consultation with a board-certified pulmonologist who specializes in "Integrated Pulmonary Care." Ask specifically about their "Wellness" or "Rehabilitation" tracks. Ensure your insurance covers a formal Pulmonary Rehab program (Code G0424), as this is often the cornerstone of the entire process. Start a daily log of your oxygen levels and activity to provide your medical team with real-world data rather than just a snapshot from an office visit.