You’ve probably heard the word "trauma" thrown around a lot lately. People use it to describe everything from a breakup to a stressful day at the office. But honestly, that’s not what it actually is. Not in the clinical sense. When we talk about psychological trauma, we aren't talking about being upset. We are talking about a literal rewiring of the brain. It’s what happens when your internal circuit breaker flips because the "voltage" of an experience was just too high for your system to handle.
It sticks. It lingers in the body.
Most people think trauma is about an event—a car crash, a natural disaster, or a violent act. That’s only half the story. Dr. Gabor Maté, a leading expert on the subject, often says that trauma isn’t what happens to you; it’s what happens inside you as a result of what happened to you. It is the wound that remains. It’s the loss of flexibility in how you respond to the world. If you’ve ever felt like you’re overreacting to something small, or if you feel nothing at all when you should be feeling a lot, you’re likely seeing the footprints of trauma.
The Science of the Stuck Brain
Trauma isn't a character flaw. It’s biology. When you experience something terrifying, your amygdala—the brain's alarm system—goes into overdrive. Usually, the hippocampus (the librarian of the brain) helps process that event and files it away in the "past" section of your memory. But with psychological trauma, the librarian gets knocked unconscious. The memory doesn't get filed. Instead, it stays "live."
It’s raw.
✨ Don't miss: Ankle Stretches for Runners: What Most People Get Wrong About Mobility
Because the memory isn't properly archived, your brain thinks the threat is still happening. This is why a specific smell, a certain tone of voice, or even a rainy day can trigger a full-blown panic attack years later. Your body is reacting to 2012 as if it were 2:00 PM today. Dr. Bessel van der Kolk explains this beautifully in his book The Body Keeps the Score. He notes that trauma survivors often have an overactive "smoke detector" in their brain, making it nearly impossible to feel safe, even when the environment is perfectly calm.
Big T vs. Little t Trauma
The clinical world used to focus almost exclusively on "Big T" traumas. We’re talking about war, physical assault, or surviving a hurricane. These are the life-threatening events that most people associate with Post-Traumatic Stress Disorder (PTSD). However, researchers are now paying much more attention to "little t" traumas.
These are different. They are the "death by a thousand cuts."
Think about emotional neglect. Think about a messy divorce, bullying, or growing up in a household where you never knew which version of a parent was going to walk through the door. While these might not be "life-threatening" in a physical sense, they are deeply threatening to a child's developing sense of self. Over time, these experiences can result in Complex PTSD (C-PTSD), which is often harder to treat because there isn't one single "event" to point to. It’s a pervasive feeling of being "wrong" or "broken."
🔗 Read more: Can DayQuil Be Taken At Night: What Happens If You Skip NyQuil
Why Some People Bounce Back and Others Don't
It seems unfair. Two people can be in the same car accident; one is back at work the next day, and the other can't get behind a wheel for a decade. Why?
It comes down to resilience and "protective factors." If you have a solid support system, a sense of agency, and the ability to talk about what happened immediately after the event, your chances of avoiding long-term psychological trauma are much higher. Isolation is the fuel that keeps trauma burning. When we are alone with our terror, the brain can't integrate the experience.
Another huge factor is childhood history. The Adverse Childhood Experiences (ACE) study, a landmark piece of research by the CDC and Kaiser Permanente, showed a direct link between childhood stressors and adult health outcomes. Basically, if your "foundation" was shaky, your "house" is more likely to sustain damage during a storm later in life. It sucks, but it’s the reality of how our nervous systems are built.
The Physical Toll Nobody Talks About
Trauma isn't just "in your head." It shows up in the gut. It shows up in chronic back pain, migraines, and autoimmune issues. When you are constantly in "fight or flight" mode, your body is flooded with cortisol and adrenaline.
💡 You might also like: Nuts Are Keto Friendly (Usually), But These 3 Mistakes Will Kick You Out Of Ketosis
This is exhausting.
Over years, this chronic stress wears down the immune system. You might find yourself catching every cold that goes around. Or maybe you have unexplained inflammation. Doctors like Dr. Arielle Schwartz, who specializes in complex trauma, emphasize that healing must involve the body, not just talk therapy. You can't just "think" your way out of a nervous system that feels like it's being hunted by a predator.
Common Signs You Might Be Dealing With It
- Hypervigilance: You're always scanning the room for exits or watching people's body language for signs of anger.
- Dissociation: You "zone out" or feel like you’re watching your life through a foggy window.
- Emotional Numbing: You can't feel the "bad" stuff, but you can't feel the "good" stuff either.
- Intrusive Thoughts: Memories of the event pop up when you’re trying to focus on something else.
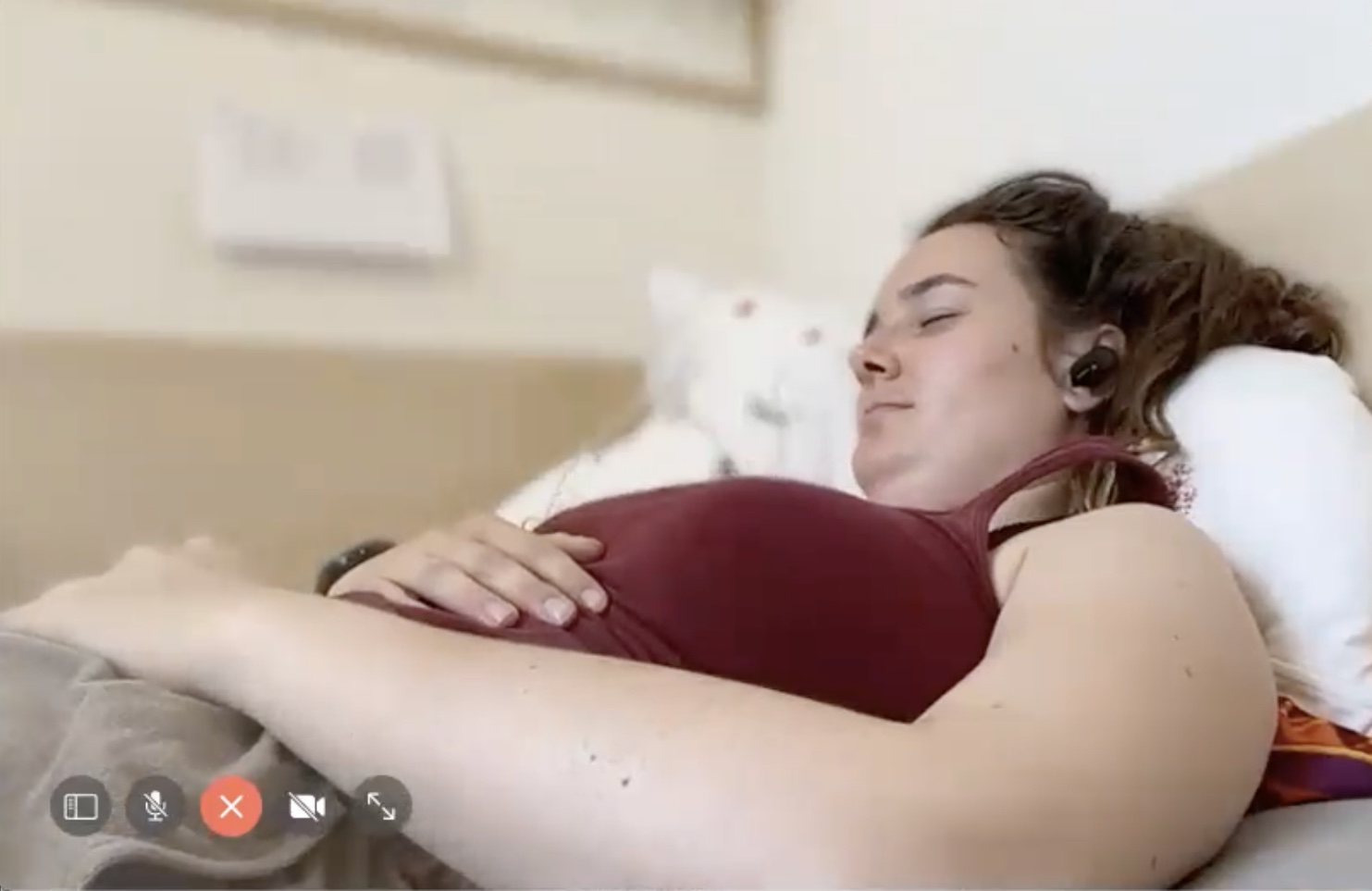
- Sleep Disturbances: Nightmares or the inability to stay asleep because your body is "on guard."
Moving Toward Recovery: What Actually Works
The good news? The brain is plastic. It can change. It can heal. But "just getting over it" is the worst advice you can give someone. You wouldn't tell someone with a broken leg to just walk it off; you shouldn't do that with psychological trauma either.
Standard "talk therapy" (CBT) can be helpful for some, but many people find that talking about the trauma actually re-traumatizes them. It keeps them stuck in the story. This is why "bottom-up" approaches are gaining so much ground. These methods focus on calming the body first so the brain can eventually catch up.
- EMDR (Eye Movement Desensitization and Reprocessing): This sounds like sci-fi, but it’s one of the most researched treatments for PTSD. It involves using bilateral stimulation (like moving your eyes back and forth) while briefly thinking about the traumatic memory. It helps the "librarian" hippocampus finally file that memory away.
- Somatic Experiencing: Developed by Peter Levine, this focuses on where the trauma is "held" in the body. It’s about noticing sensations—tightness in the chest, heat in the neck—and slowly releasing that stored energy.
- Neurofeedback: This uses real-time displays of brain activity to teach the brain how to regulate itself. It’s like a workout for your nervous system.
- Mindfulness and Yoga: These aren't just for "wellness influencers." For a trauma survivor, being "present" in the body is the scariest place to be. Gentle yoga can help people slowly re-inhabit their bodies in a way that feels safe.
Actionable Steps for Navigating Trauma
If you suspect you're living with the effects of psychological trauma, the first thing you need to do is stop blaming yourself. Your symptoms are actually brilliant adaptations. Your brain isn't "broken"—it's trying to protect you. It just doesn't realize the war is over.
- Find a trauma-informed therapist. This is non-negotiable. Look for someone who mentions "somatic," "EMDR," or "IFS" (Internal Family Systems). Avoid therapists who just want to do "general vent sessions" if you're trying to process deep-seated trauma.
- Track your triggers. Keep a small note on your phone. When you feel that sudden surge of anxiety or the urge to shut down, what just happened? Was it a sound? A smell? A certain type of person? Identifying the "smoke" helps you realize there isn't an actual fire.
- Practice "Grounding." When the past starts bleeding into the present, use the 5-4-3-2-1 technique. Look for five things you can see, four you can touch, three you can hear, two you can smell, and one you can taste. This forces your brain back into the current moment.
- Limit your "input." If your nervous system is already fried, watching the news for three hours or scrolling through stressful social media feeds is like throwing gasoline on a fire. Protect your peace aggressively.
- Prioritize sleep and protein. It sounds basic, but a dysregulated nervous system burns through energy. Your brain needs fuel to do the heavy work of healing.
Healing from trauma is rarely a straight line. It's more of a spiral. You might feel great for a month and then get hit with a wave of old feelings. That’s okay. The goal isn't to erase the memory; the goal is to make the memory just a memory—something that happened back then, rather than something that is happening right now. You deserve to live in the present.