You're staring at two bottles on your nightstand. One is a heavy-duty antibiotic prescribed by your doctor to kill off that stubborn sinus infection. The other is a bottle of expensive probiotics you bought because you heard they "protect the gut." Now comes the million-dollar question: Do you take them together, or is that just flushing money down the toilet?
Most people think it’s a zero-sum game. They assume the antibiotic will just "delete" the probiotic on contact. While that’s partially true if you’re reckless with the clock, the reality of probiotics and antibiotics timing is a lot more nuanced—and honestly, a bit more annoying to manage—than just swallowing a handful of pills at breakfast.
Antibiotics are scorched-earth agents. They don't have a GPS. They can’t tell the difference between the Streptococcus causing your throat to feel like it's full of glass and the Lactobacillus helping you digest your lunch. If you take them at the exact same moment, the antibiotic is basically going to treat those expensive probiotics like a snack.
The Two-Hour Rule is Actually a Thing
It’s not just an old wives' tale. Most pharmacists and researchers, including those published in journals like Gastroenterology & Hepatology, suggest a window of at least two hours. Personally, I think three is better if you can swing it.
Think of it like a battlefield. You want the "good guys" (probiotics) to arrive after the "bombs" (antibiotics) have already moved through the primary landing zone of your stomach and upper GI tract. If you take your antibiotic at 8:00 AM, wait until at least 10:30 AM or 11:00 AM for the probiotic. This gives the medication time to be absorbed into your bloodstream, reducing the direct physical contact between the drug and the live cultures in the supplement.
Does this save every single microbe? No. But it prevents total annihilation.
Why You Shouldn't Wait Until the Prescription is Over
There is a weird, lingering myth that you should wait until you’ve finished the entire Z-Pack before touching a probiotic. This is actually bad advice for most people.
💡 You might also like: How to Treat Uneven Skin Tone Without Wasting a Fortune on TikTok Trends
The whole point of taking these supplements during a course of meds is to prevent Antibiotic-Associated Diarrhea (AAD). If you wait ten days until the prescription is done, the damage to your microbiome is already a "done deal." You're essentially trying to replant a forest after it’s already burned to the ground, rather than trying to protect the soil while the fire is still burning.
A massive meta-analysis published in JAMA looked at over 600 studies and found that taking probiotics during the antibiotic course reduced the risk of diarrhea by about 42%. That’s not a small number. If you wait until day 11, you’ve missed the window where the probiotics act as a placeholder, preventing opportunistic pathogens like Clostridioides difficile (C. diff) from taking over the empty real estate in your gut.
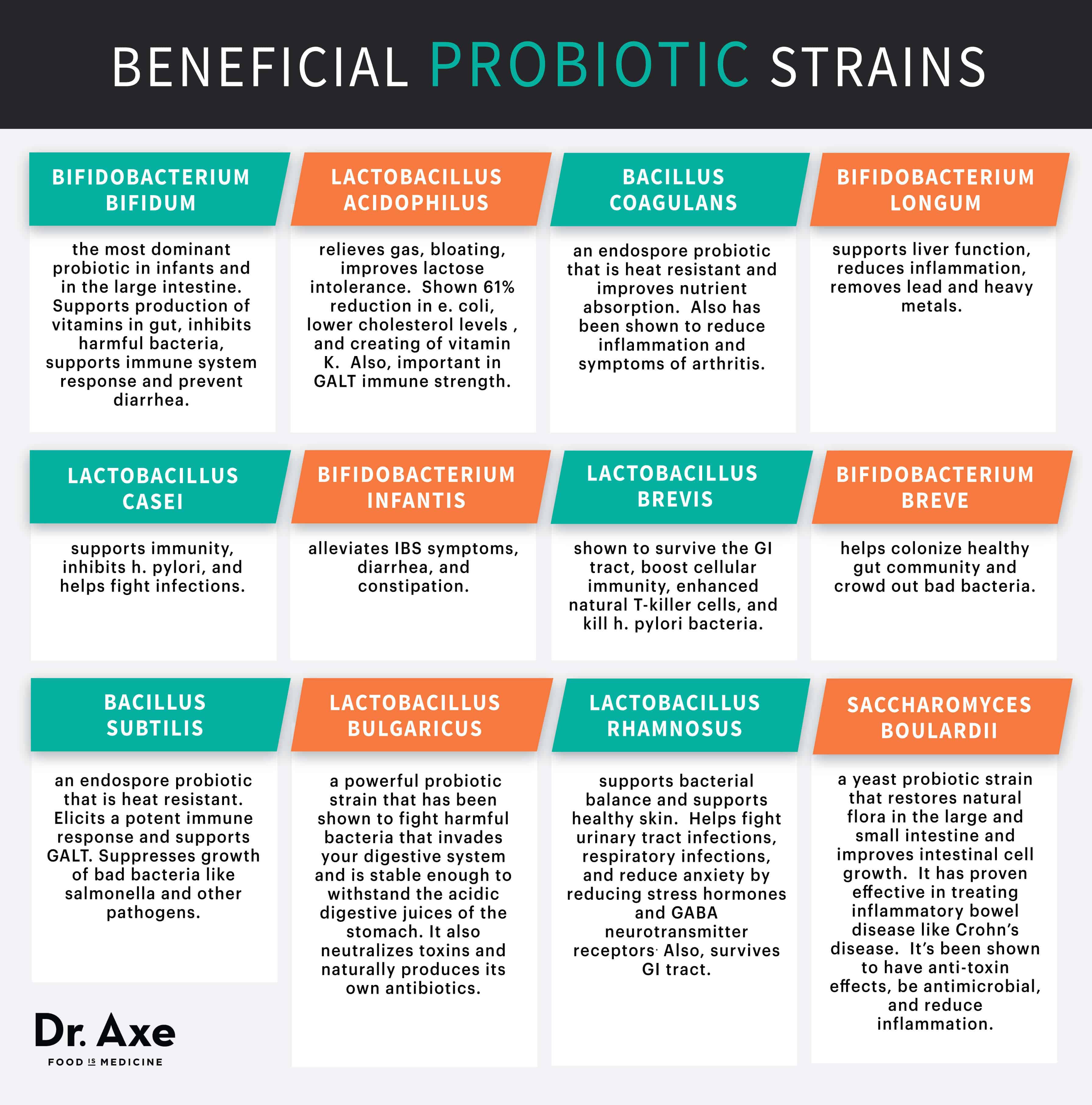
The Specific Strains Matter More Than the Brand
Don't just grab the "probiotic yogurt" with the prettiest packaging. Most of those are fine for general health, but they aren't clinical-grade protection against pharmaceutical-grade antibiotics.
If you want to be smart about probiotics and antibiotics timing, you need to look for two specific powerhouses:
- Saccharomyces boulardii: This is actually a beneficial yeast, not a bacteria. Because it’s a yeast, antibiotics can't kill it. You could literally swallow it with your penicillin and it wouldn't care. It’s the "tank" of the probiotic world.
- Lactobacillus rhamnosus GG: This is one of the most studied strains for preventing AAD. It’s tough. It sticks to the gut wall.
If your supplement doesn't list the specific strain (the letters and numbers after the name), it’s probably a generic blend that might not survive the trip.
The "Die-Off" Reality
Some people feel worse when they start probiotics mid-antibiotic. They get gas, bloating, or a weird "brain fog." This is often called a Herxheimer reaction, or more simply, "die-off." It’s basically your internal ecosystem undergoing a violent shift in power.
📖 Related: My eye keeps twitching for days: When to ignore it and when to actually worry
If this happens, don't quit. Just adjust. Maybe move the probiotic further away from the antibiotic dose. Instead of two hours, try four. The goal is consistency, not perfection. You're trying to maintain a "baseline" population of good bacteria so that when the antibiotics stop, your gut can bounce back in weeks rather than months.
Real World Timing Scenarios
Let's look at how this actually plays out in a daily schedule. If your doctor has you on a twice-daily (BID) antibiotic schedule—say, 9:00 AM and 9:00 PM—your "safe zones" for probiotics are the mid-day and the late afternoon.
- 9:00 AM: Antibiotic + Meal
- 1:00 PM: Probiotic (The "Sweet Spot")
- 6:00 PM: Probiotic (Optional second dose)
- 9:00 PM: Antibiotic + Meal
If you're on a once-a-day dose, it's way easier. Just put 12 hours between them. Antibiotic in the morning, probiotic before bed. Done.
The Role of Prebiotics (The Food for the Good Guys)
Taking the pill is only half the battle. If you’re dropping these expensive microbes into a gut that’s being ravaged by antibiotics, you need to give them something to eat so they can colonize quickly. This is where "prebiotics" come in.
While you're on the meds, try to eat:
- Onions and garlic (natural antimicrobials anyway)
- Slightly under-ripe bananas (resistant starch)
- Asparagus
- Oats
It’s like sending the soldiers in with a lunchbox. It gives them a fighting chance to stay put instead of just passing through your system.
👉 See also: Ingestion of hydrogen peroxide: Why a common household hack is actually dangerous
What About Fermented Foods?
I love kimchi and sauerkraut as much as the next health nut, but during an antibiotic course, they probably aren't enough on their own. The CFU (Colony Forming Units) count in a serving of yogurt is often much lower and less diverse than a high-quality capsule. Think of fermented foods as the "maintenance crew" and a targeted probiotic supplement as the "emergency response team." You need the emergency team right now.
Common Mistakes to Avoid
People often mess up the temperature. Many high-quality probiotics are light-sensitive or heat-sensitive. If you leave them on a sunny windowsill next to your antibiotics, the bacteria might be dead before they even hit your stomach acid. Keep them in a cool, dark place, or the fridge if the label says so.
Another big one: taking them on a completely empty stomach. While some brands claim "enteric coating" allows for empty-stomach dosing, most probiotics survive the gauntlet of stomach acid better when there's a little bit of food—specifically a little bit of healthy fat—to buffer the pH levels. A few bites of avocado or a spoonful of almond butter can act as a shield.
Practical Next Steps for Gut Recovery
If you’re currently mid-prescription or about to start one, here is the move:
- Check your strains. Look for S. boulardii or L. rhamnosus GG on the back of the bottle. If it just says "probiotic blend," it’s a gamble.
- Set a phone alarm. Do not rely on your memory. If you take your antibiotic, set a timer for 150 minutes. When it goes off, take your probiotic.
- Stay hydrated. Antibiotics put stress on your kidneys and liver; water helps flush the "debris" of the bacteria the meds are killing off.
- Watch for the "Red Flags." Probiotics help, but they aren't a cure-all. If you develop a fever, severe abdominal pain, or bloody stool, stop the supplements and call your doctor immediately. This could be a sign of a more serious infection that a supplement can't fix.
- Continue for 2 weeks after. The day you finish your antibiotics is not the day you stop the probiotics. Continue the supplements for at least 14 days post-antibiotic to ensure the "regrowth" phase is successful.
The gut is resilient, but it isn't invincible. Managing probiotics and antibiotics timing correctly is probably the simplest way to avoid the "antibiotic hangover" and get your energy back faster. Focus on the gap between doses, prioritize the right strains, and don't stop too early.