Ever felt like you're swimming in a sea of confusing medical statistics? You're not alone. One minute a news report says a disease is "on the rise," and the next, they’re throwing around terms like "incidence" and "prevalence" as if we all have PhDs in epidemiology. But honestly, understanding what does prevalence mean is actually the secret to knowing how much a health issue is truly affecting your community right now.
Think of it as a snapshot.
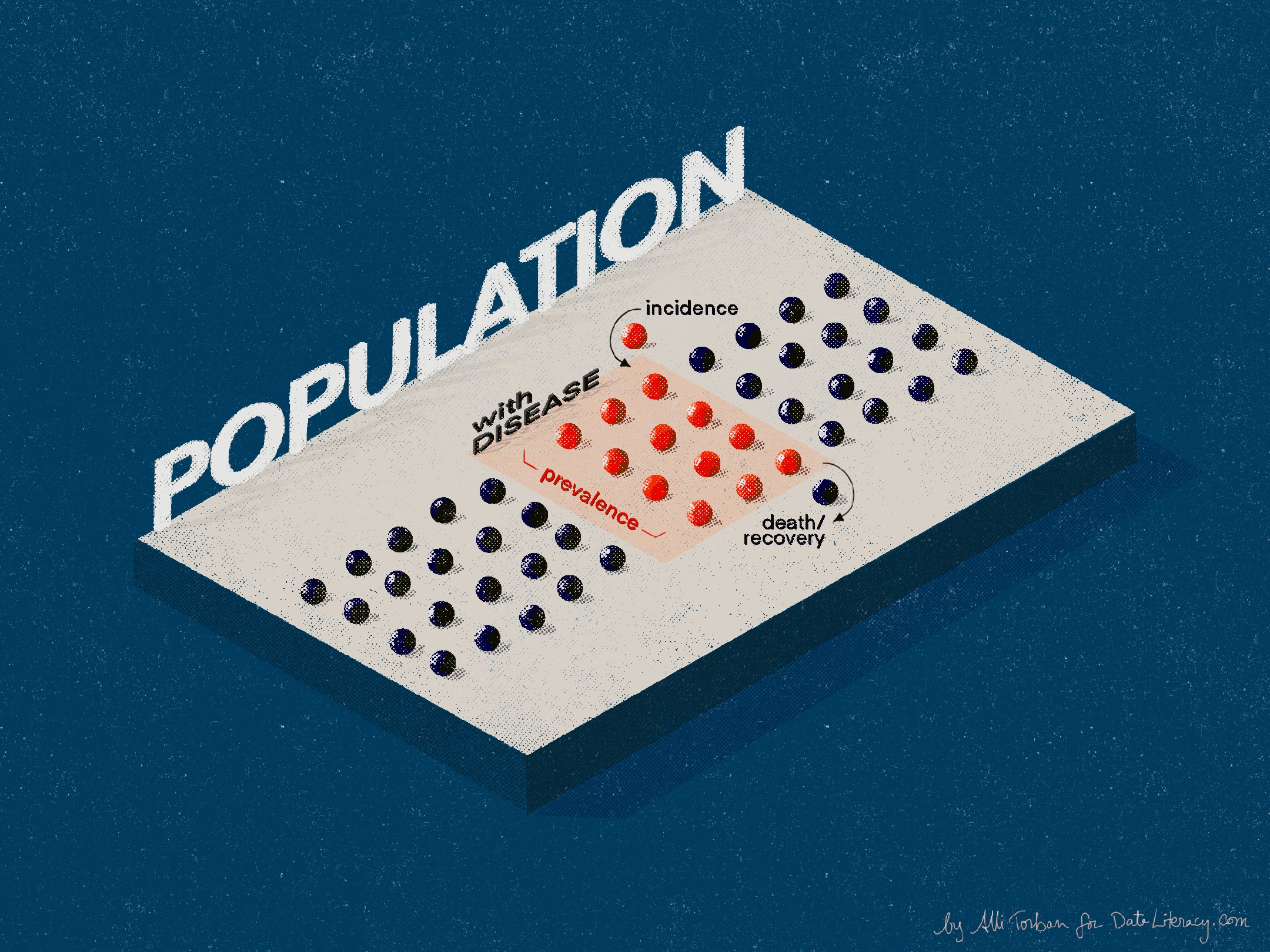
If you take a photo of a crowded stadium, you’re seeing everyone who is there at that exact second. That’s prevalence. It doesn’t matter if they just walked through the gates or if they’ve been sitting in the bleachers for three hours. They are there. They "count." In health terms, prevalence represents the total number of people living with a specific condition in a population at a specific point in time.
It’s about the burden.
The Snapshot vs. The Video: Getting Prevalence Right
People constantly confuse prevalence with incidence. It’s the most common mistake in health reporting. While prevalence is that static snapshot of everyone currently affected, incidence is more like a video of the turnstiles. Incidence only tracks the new cases.
👉 See also: When Does Dick Stop Growing: What the Science Actually Says About Your Timeline
Imagine a bathtub.
The water already in the tub is the prevalence. The water flowing from the faucet represents the incidence—the new cases arriving. The drain? That represents people who either recover or, unfortunately, pass away. If the faucet is leaking fast but the drain is clogged, the water level—the prevalence—is going to skyrocket.
This is why some "scary" prevalence numbers are actually signs of medical progress. Take HIV, for example. In the 1980s, the prevalence was relatively low because people didn't survive very long after a diagnosis. Today, prevalence is much higher. Why? Because people are living long, healthy lives with the virus thanks to antiretroviral therapy. The "tub" is filling up because fewer people are leaving through the "drain."
Why Prevalence Matters More Than You Think
When a local government decides where to build a new dialysis center or how many mental health counselors to hire for a school district, they don't just look at who got sick last week. They look at the total number of people who need help today.
Basically, prevalence dictates resource allocation.
If a city has a high prevalence of Type 2 diabetes, that tells city planners they need more podiatrists, more insulin access, and perhaps better public parks to encourage exercise. It’s a measure of the "load" on the healthcare system. Without these numbers, we’re just guessing.
There are two main ways experts talk about this:
- Point Prevalence: This is the most literal snapshot. How many people have the flu on January 15th?
- Period Prevalence: This looks at a window of time. How many people had the flu at any point during the entire winter season?
The World Health Organization (WHO) uses these metrics to track everything from malaria in sub-Saharan Africa to obesity rates in North America. For instance, the Global Burden of Disease study—a massive, ongoing collaboration involving thousands of researchers—relies heavily on prevalence to rank which diseases are causing the most disability worldwide.
The Nuance: Why the Numbers Can Be Deceptive
It's easy to look at a percentage and think you have the whole story. You don't.
Prevalence can be influenced by how "good" we are at finding a disease. If a new, highly accurate diagnostic test for Alzheimer’s is released tomorrow, the reported prevalence will likely jump. Did more people get the disease overnight? No. We just finally saw the people who were already in the stadium but were hiding in the shadows.
🔗 Read more: How to Cure Headache Quickly: What Actually Works When Your Brain Is Thumping
Context is everything.
Sometimes, a high prevalence is a "good" bad sign. In many developed nations, the prevalence of age-related conditions like osteoarthritis is high because people are actually living long enough to develop it. In countries with lower life expectancies, the prevalence of these conditions is lower—not because the population is "healthier," but because people are dying from other causes before their joints wear out.
We also have to talk about "lifetime prevalence." This is a different beast entirely. It’s the proportion of a population that has ever had a condition at some point in their life. You see this a lot in mental health discussions. You might hear that the lifetime prevalence of depression is around 20%. That doesn't mean one in five people are depressed right now; it means one in five will experience it at some stage.
Breaking Down the Math (The Simple Version)
You don’t need a calculator to get the gist, but the formula is straightforward. You take the number of existing cases and divide it by the total population.
$$Prevalence = \frac{Total\ Cases}{Total\ Population}$$
If you want to express it as a percentage, you multiply by 100. If it’s a rare disease, scientists usually express it as "cases per 10,000" or "cases per 100,000."
For example, look at Multiple Sclerosis (MS). According to the National MS Society, nearly 1 million adults in the U.S. are living with the condition. With a population of roughly 330 million, that gives us a prevalence of about 0.3%. That might sound small, but when you realize that's 1 million individuals needing specialized care, the "weight" of that number becomes much heavier.
Common Misconceptions That Mess With Your Head
I’ve seen people argue that because the prevalence of a disease is low, we shouldn't spend money on it. That’s a dangerous way to look at data.
Rare diseases (often defined as affecting fewer than 200,000 people in the U.S.) have low prevalence by definition. But there are over 7,000 different rare diseases. When you add them all up, the combined prevalence is huge. About 1 in 10 Americans lives with a rare disease.
Another huge misconception is that prevalence equals risk.
It doesn't.
Prevalence tells you how widespread a condition is, but it doesn't tell you your personal chance of catching it or developing it. That’s what "risk" (often derived from incidence) is for. If you’re looking at the prevalence of shark attacks, it’s practically zero. But if you’re currently bleeding in the water next to a Great White, your risk is 100%.
The Social Factor: Who Gets Counted?
We have to be honest: prevalence data is only as good as the people collecting it.
Historically, certain populations have been undercounted. If a community lacks health insurance or doesn't trust the medical establishment, their illnesses won't show up in the "official" prevalence numbers. This leads to what's known as "health inequities."
For years, the prevalence of certain heart conditions in women was underestimated because medical research focused primarily on how those conditions appeared in men. We literally didn't know what we were looking for, so we didn't count it.
When you see a prevalence stat, always ask: Who was included in this study? Who was left out?
Real-World Examples to Keep in Your Back Pocket
- Obesity: The CDC reports that the prevalence of obesity in the U.S. is currently over 40%. This is a "high-prevalence" chronic issue that requires long-term public health strategies rather than a quick fix.
- Common Cold: The point prevalence of the cold is massive in January and tiny in July. This is a classic example of how time-sensitive these numbers are.
- Smallpox: The prevalence of smallpox is zero. It’s the gold standard of public health—taking a prevalence number and driving it all the way down through global effort.
How to Use This Information Like an Expert
Next time you see a headline about a "health crisis," don't panic. Check if they are talking about prevalence or incidence.
If a disease has high prevalence but low incidence, it means it’s a chronic condition that people are managing. It's a "maintenance" challenge. If incidence is high, it's an "outbreak" challenge. Knowing the difference changes how you react.
If you’re researching a condition for yourself or a loved one, look for "age-adjusted prevalence." This is a fancy way of making sure the data isn't skewed by a very old or very young population. It gives you a much clearer picture of what the "average" person faces.
Actionable Steps for Navigating Health Data:
- Verify the denominator: When someone says "1,000 people have this," ask "out of how many?" 1,000 out of a million is very different from 1,000 out of a small town.
- Check the date: Prevalence is a snapshot. A 2015 study on the prevalence of vaping is useless in 2026.
- Look for geographic specifics: Prevalence in New York City rarely matches prevalence in rural Wyoming. Environmental factors, lifestyle, and local industry change the numbers completely.
- Distinguish between "self-reported" and "clinically diagnosed": Studies that ask people "do you have back pain?" will always show higher prevalence than studies that look at MRI results.
Understanding prevalence is about seeing the big picture without losing sight of the individuals who make up the statistics. It's the difference between hearing noise and actually hearing the music. By focusing on the total burden of a disease, we can better prepare our hospitals, our schools, and our own medicine cabinets for what’s actually happening on the ground.
✨ Don't miss: Sand, Salt, and Your Vagina on the Beach: How to Actually Stay Comfortable
Keep these distinctions in mind when you're browsing health portals or watching the evening news. The "burden" of a disease is a heavy thing to measure, but it's the only way we can effectively move toward a healthier society.