You just got the call. Or maybe you saw the notification pop up in your patient portal. You see a number—maybe it’s a 5.8 or a 6.2—and next to it, the word "Pre-diabetes" is staring back at you. It feels like a weight. Honestly, it’s a weird middle ground to be in. You aren’t "sick" in the traditional sense, but you aren't exactly in the clear either.
Pre diabetic a1c levels are essentially a warning shot from your pancreas.
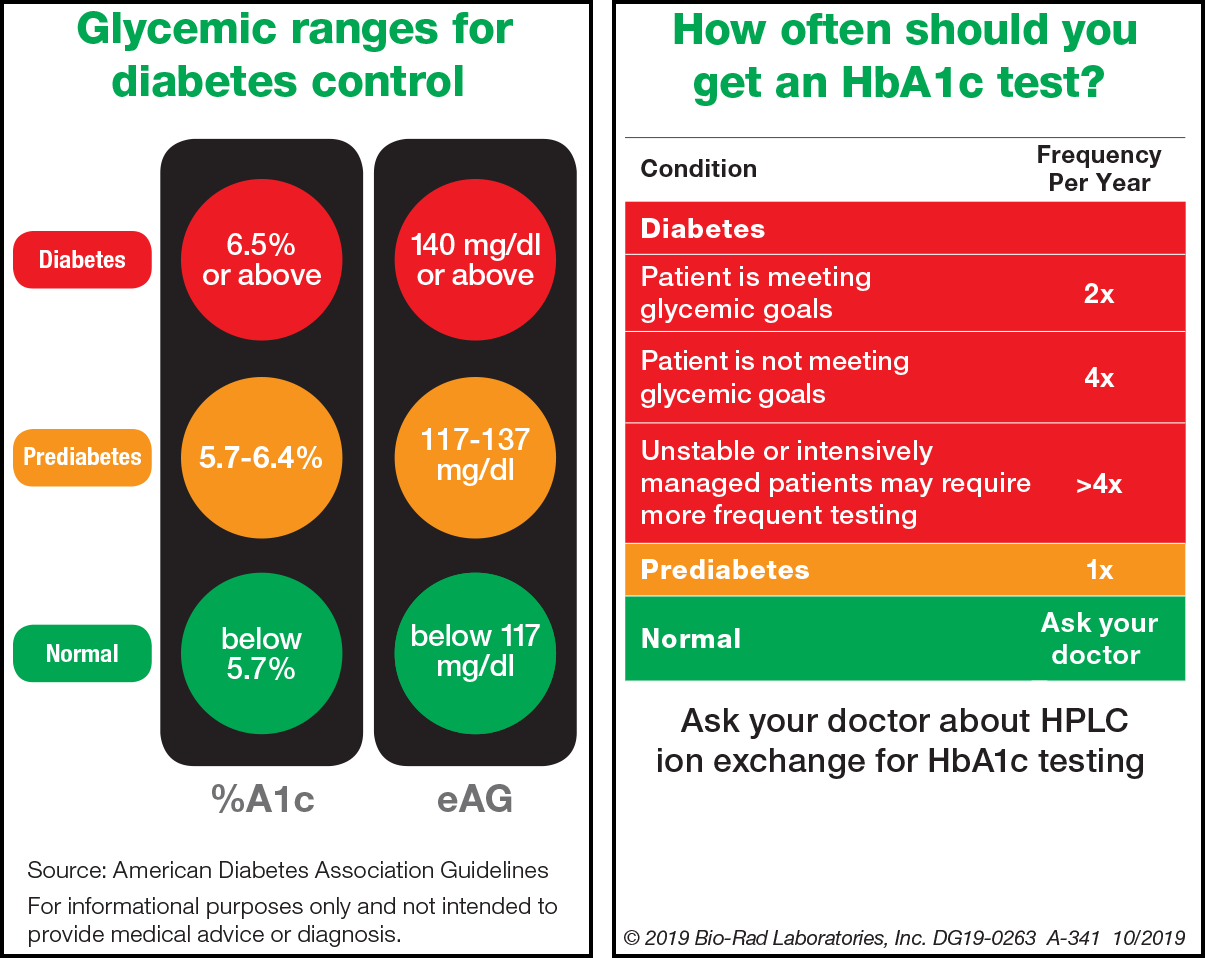
The Hemoglobin A1c test is basically a three-month average of your blood sugar. Think of it like a GPA for your glucose. While a finger-prick test tells you what’s happening right this second, the A1c shows the big picture. When that number hits the 5.7% to 6.4% range, the medical community labels you as pre-diabetic. Anything 6.5% or higher? That’s the threshold for Type 2 diabetes.
But here’s the thing: these numbers aren't some magic wall. Your body doesn't suddenly break the moment you hit 6.5%. It’s a spectrum. And if you're sitting at a 5.9%, you're already experiencing some of the internal wear and tear that comes with high blood sugar.
✨ Don't miss: Medical Alert Bracelet Tattoo: Why Emergency Doctors Are Torn
The actual math behind pre diabetic a1c levels
Most people don't realize what that percentage actually means in terms of daily sugar. If your A1c is 6.0%, your average blood sugar is sitting around 126 mg/dL. For a "normal" person, that average is closer to 100 mg/dL or less. That extra 26 points might not seem like a lot, but imagine your blood vessels being bathed in that extra syrup every single minute of every single day. It adds up.
According to the American Diabetes Association (ADA), roughly 98 million American adults have pre-diabetes. That’s more than 1 in 3. The scary part? More than 80% of them have no clue. They feel fine. Maybe a little tired after lunch, but who isn't?
The A1c test measures how much sugar is stuck to your red blood cells. Red blood cells live for about 90 to 120 days. So, if your blood sugar has been high, those cells are "glycated"—basically sugar-coated. Once that sugar is stuck, it’s stuck. You can’t "cheat" an A1c test by eating a salad the night before the blood draw. It’s a snitch. It tells the truth about the last three months.
Why doctors sometimes gloss over the 5.7% mark
It's frustrating. You might see your results are 5.7% and your doctor says, "Keep an eye on it," and sends you home. They're busy. They're looking for "fires" to put out, and 5.7% is more like a smoldering ember. But for you, that's the time to act.
Dr. Sarah Hallberg, a renowned expert in reversing Type 2 diabetes, often argued that waiting until someone hits the official "diabetic" mark is a failure of the system. By the time you reach 6.5%, your beta cells—the little factories in your pancreas that make insulin—might already be struggling or dying off.
Does age matter?
Interestingly, the "normal" range is a bit of a debate in the geriatric world. For a 25-year-old, a 5.9% A1c is a loud alarm. For an 85-year-old? Doctors might be okay with that because trying to push blood sugar too low in the elderly can cause "hypoglycemia" (dangerously low sugar), which leads to falls and confusion. Context is everything.
The metabolic "traffic jam"
When you have pre diabetic a1c levels, you likely have insulin resistance.
Imagine your cells have doors. Insulin is the key that unlocks the door to let sugar in for energy. In pre-diabetes, the locks are rusty. Your pancreas has to scream (produce way more insulin) just to get the doors to budge. Eventually, the pancreas gets tired. The sugar stays in the hallway (your bloodstream) because it can't get into the rooms (your cells).
That’s why you might feel hungry or tired even if you just ate. Your cells are literally starving while surrounded by sugar they can't use.
Surprising symptoms you might be ignoring
- Skin tags: Those little bumps on your neck or armpits? They are often linked to high insulin.
- Acanthosis Nigricans: This is a fancy term for dark, velvety patches of skin, usually on the back of the neck or knuckles.
- Brain fog: Feeling like you're walking through a cloud after a high-carb meal.
- The "3 PM Slump": That desperate need for a nap or more caffeine mid-afternoon.
Can you actually "reverse" these numbers?
Yes. 100%. Sorta.
Medical purists hate the word "reverse" because the underlying tendency toward insulin resistance usually stays with you. If you go back to eating a box of donuts every day, the numbers will spike again. But you can absolutely achieve "remission."
💡 You might also like: Converting 5000 i.u to mg: Why the Math Changes Depending on Your Supplement
The Diabetes Prevention Program (DPP), a landmark study, showed that people with pre-diabetes who lost just 5% to 7% of their body weight and added 150 minutes of brisk walking per week reduced their risk of progressing to Type 2 diabetes by 58%. For people over age 60, that risk reduction was 71%.
That’s huge. It’s more effective than many medications.
Real talk about the "Pre-diabetes Diet"
Forget the "everything in moderation" advice for a second. If your A1c is creeping up, your body is telling you it can’t handle the current load of carbohydrates you're feeding it.
You don't have to go full Keto if you don't want to. But you do need to understand the "Glycemic Load." A bowl of oatmeal and a bowl of sugary cereal might look different, but to a body with pre-diabetes, they can both send blood sugar soaring.
The "Starch Trick"
Researchers like Jessie Inchauspé (The Glucose Goddess) have shown that the order in which you eat food matters. If you eat fiber (greens) first, then proteins and fats, and save the starches for the end of the meal, you can flatten the glucose spike significantly. It’s the same amount of food, but a totally different hormonal response.
Why the A1c test isn't perfect
We rely on it heavily, but it has flaws.
If you have anemia, or if your red blood cells live longer or shorter lives than average, your A1c might be "falsely" high or low. For example, if you have iron-deficiency anemia, your red cells stay in circulation longer. That gives them more time to collect sugar, which can artificially inflate your A1c.
Some people use a Continuous Glucose Monitor (CGM) to get the "ground truth." It’s a little sensor you wear on your arm. It shows you exactly what happens to your sugar when you eat a banana versus an apple. For many, seeing that spike on a graph is the "aha!" moment that a lab report never provides.
Moving the needle: Actionable steps
If you're staring at a lab report with pre diabetic a1c levels, don't panic. Panic raises cortisol. Cortisol raises blood sugar. It’s a vicious cycle.
Instead, do this:
- Walk after you eat. Even 10 minutes. Muscle contractions are the most efficient way to "sponge up" excess sugar from your blood without needing extra insulin.
- Prioritize protein at breakfast. Ditch the toast or cereal. Go for eggs, Greek yogurt (unsweetened), or a protein shake. Starting the day with a sugar spike sets you on a roller coaster you can't get off until you sleep.
- Strength training. You don't need to be a bodybuilder. But muscle is "metabolically expensive" tissue. The more muscle you have, the more places your body has to store glucose.
- Sleep is non-negotiable. One night of poor sleep (less than 6 hours) can make you as insulin resistant as a diabetic the next morning. It sounds like an exaggeration, but the data from the National Institutes of Health (NIH) is pretty clear on this.
- Check your meds. Some drugs, like statins or certain diuretics, can slightly nudge your blood sugar up. Don't stop taking them, but ask your doctor if your medication could be contributing to the climb.
Understanding the "Dawn Phenomenon"
You might notice that if you check your sugar first thing in the morning, it's high—even if you haven't eaten in 10 hours. This drives people crazy.
It’s called the Dawn Phenomenon. Your liver dumps a bunch of sugar into your blood to give you energy to wake up and start your day. In a healthy metabolism, insulin handles this easily. In pre-diabetes, that sugar just sits there. If your morning numbers are high, it’s a sign that your liver is a bit "fatty" or overworked.
Focusing on a lower-carb dinner and avoiding late-night snacking can often help settle that morning spike over time.
The big picture
A1c levels in the pre-diabetic range are not a sentence. They are data.
It’s your body’s way of saying, "Hey, the current system is overloaded. We need a change." Whether that's through more movement, different food choices, or better stress management, the power is actually in your hands. Most chronic conditions aren't this "fixable." This one is.
Take the 5.8% or the 6.1% for what it is: an opportunity to pivot before the damage becomes permanent.
Immediate Next Steps:
- Review your lab work: Look for your Triglyceride to HDL ratio. If it’s over 2.0, you likely have insulin resistance, regardless of what the A1c says.
- The 10-minute rule: Commit to walking for 10 minutes after your largest meal of the day starting today.
- Fiber first: At your next meal, eat your vegetables before you touch the bread or potatoes.
- Retest: Don't wait a year. Request a follow-up A1c in 3 to 6 months to see if your lifestyle shifts are hitting the mark.