You’re scrolling through your phone, looking at a photo from last weekend’s beach trip, and there it is. A jagged, purple line snaking down your calf that you swear wasn't there last summer. Or maybe you've been obsessively Googling pictures of varicose veins because your shins have started to look like a topographical map of the Amazon River. It’s a weirdly personal thing, seeing your skin change like that. Most people think it’s just a "getting older" thing or a "standing too much at work" thing, but the visual reality of venous insufficiency is actually a pretty complex biological map.
It’s not just about vanity.
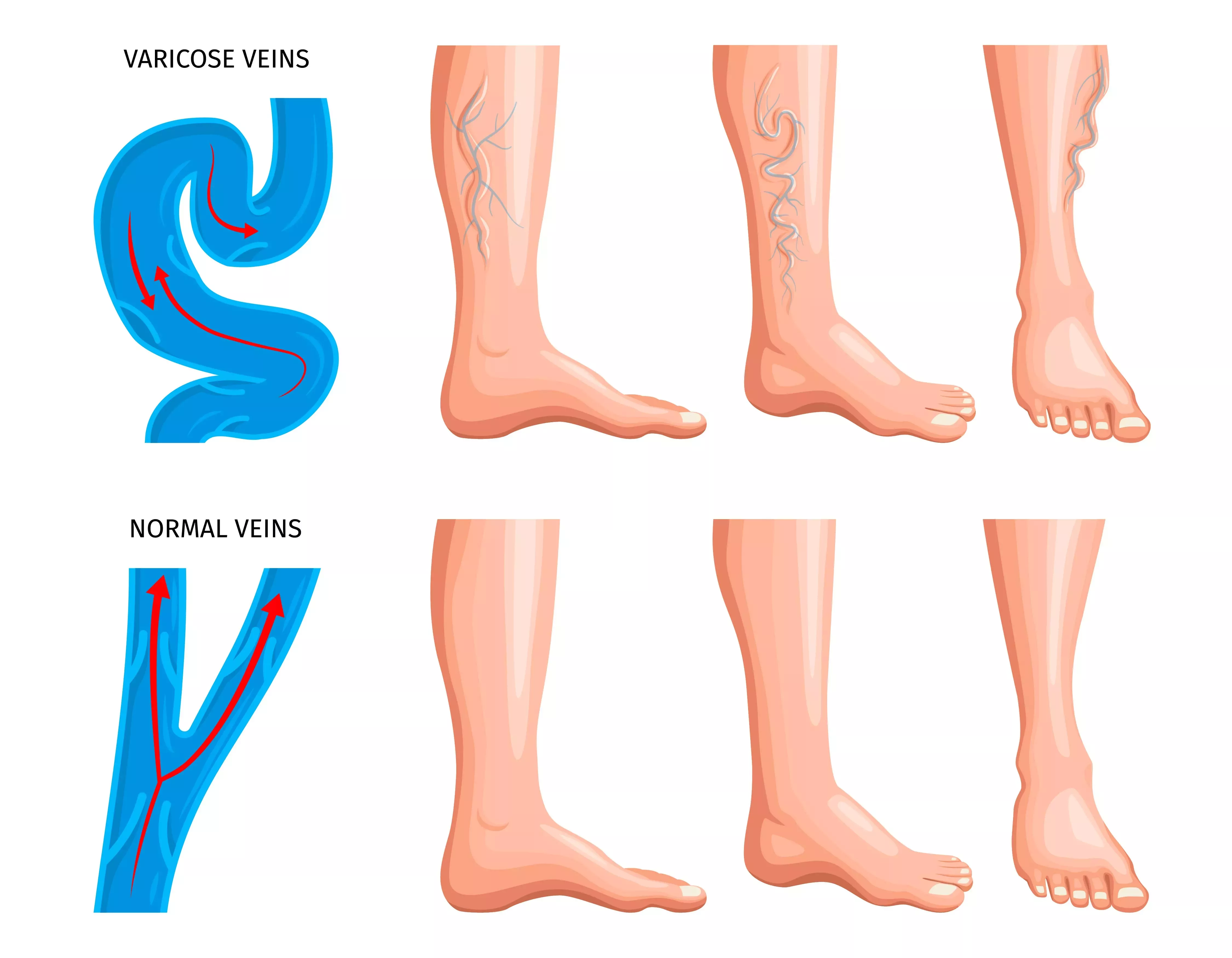
When you look at pictures of varicose veins, you aren't just looking at cosmetic blemishes. You’re looking at a pressurized hydraulic system that’s starting to fail. Your veins have these tiny one-way valves. Their only job is to push blood back up toward your heart, fighting gravity every inch of the way. When those valves get weak or just stop working, the blood pools. It stretches the vein wall. It twists. It turns blue or deep purple because that blood is deoxygenated and just... sitting there.
Honestly, the variety is wild. Some people have those thick, ropey cords that look like they’re about to pop through the skin. Others have what look like fine, sunburst patterns of red and blue, often called spider veins, though doctors technically call them telangiectasias.
Identifying the Stages: Not All Pictures of Varicose Veins Look the Same
If you look at enough medical photography, you’ll notice a pattern. Doctors use something called the CEAP classification to track how bad things are getting. It’s not just a random mess; there’s a progression.
Initially, you might see nothing. Your legs ache, they feel heavy like lead weights by 4:00 PM, but the skin looks fine. This is the "invisible" stage. Then come the spider veins. They’re small. They’re annoying. They usually don't hurt, but they're the first visual cue that the "plumbing" in your legs is under stress.
Then things get real.
🔗 Read more: Ingestion of hydrogen peroxide: Why a common household hack is actually dangerous
True varicose veins are usually 3 millimeters in diameter or larger. In pictures of varicose veins at this stage, you’ll see that classic bulging. This is Stage C2. If you start seeing swelling around the ankles—edema—you've hit Stage C3. This is where the fluid starts leaking out of the veins into the surrounding tissue because the pressure is just too high.
The Warning Signs You Can’t Ignore
There’s a specific look that should actually scare you a little bit. It’s a brownish or rusty discoloration around the ankles. It looks like a permanent tan or maybe a bruise that never heals. This is called hemosiderin staining. It happens because red blood cells are literally being forced out of the capillaries and dying in your skin, leaving iron deposits behind.
If you see this in your own photos or in the mirror, it’s a massive red flag.
It means the skin is becoming "starved" of fresh blood and nutrients. Left alone, this leads to lipodermatosclerosis—where the skin gets hard and woody—and eventually, venous ulcers. Those are open sores that are notoriously difficult to heal. According to the Society for Vascular Surgery, about 1% of Americans will deal with these ulcers at some point, and they almost always start with those "harmless" looking bulges.
Why Do My Veins Look Different Than Yours?
Genetics is the big one. If your mom had "bad legs," you're likely headed down the same path. But it’s also about lifestyle.
Think about a cashier or a surgeon. They stand still for hours. Without the calf muscles contracting to "pump" the blood upward, the pressure builds. On the flip side, someone who sits at a desk all day has the same problem; the pump isn't working because the legs aren't moving.
💡 You might also like: Why the EMS 20/20 Podcast is the Best Training You’re Not Getting in School
Pregnancy is another massive factor. You've got increased blood volume and a whole human pressing down on the pelvic veins. It's a recipe for sudden, dramatic changes in how your legs look. The good news? Sometimes those pregnancy-related veins shrink back after delivery, but they often leave the valves permanently weakened.
Real Examples and Misconceptions
People often see pictures of varicose veins and assume it's an "old person" problem. That's a total myth. I’ve seen athletes in their 20s with significant varicosities because of high-impact strain or genetic predisposition.
Another big mistake? Thinking that because a vein is small, it isn't "bad." Sometimes those tiny surface veins are actually "feeders" coming from a much larger, deeper vein that has completely failed. You could zap the surface vein with a laser a hundred times, and it would keep coming back until you fix the source deeper underground.
The Tech Behind the Diagnosis
When you go to a specialist like a vascular surgeon or a phlebologist, they aren't just looking at the surface. They use Duplex Ultrasound.
This is essentially "live-action" pictures of varicose veins from the inside. They can actually see the blood flowing backward—this is called reflux. If the blood flows backward for more than 0.5 seconds, that valve is clinically "leaking." It’s fascinating and a bit gross to see it on the screen, but it’s the only way to know what’s actually happening under the skin.
Treatment Isn't What It Used To Be
Forget what you heard about "vein stripping." That was a brutal, bloody surgery from the 1980s that involved literally pulling veins out with hooks. Nobody does that anymore unless it’s an extreme case.
📖 Related: High Protein in a Blood Test: What Most People Get Wrong
Today, it’s mostly "fire and glue."
- Endovenous Laser Ablation (EVLA): They slide a tiny fiber into the vein and use heat to cauterize it shut. Your body just reroutes the blood to healthy veins.
- Sclerotherapy: They inject a foam that irritates the vein lining, causing it to collapse and fade away. Great for those spider veins you see in pictures of varicose veins.
- VenaSeal: This is literally medical-grade superglue. They glue the vein shut. No heat, no tumescent anesthesia (which involves a lot of numbing pokes), and you can usually go back to the gym the next day.
How to Manage the Visuals at Home
Look, you can't "cure" a varicose vein with a cream. Any "miracle vein eraser" cream you see advertised on social media is basically just a heavy-duty concealer or a moisturizer with some caffeine to temporarily tighten the skin. It won’t fix a broken valve.
But you can stop things from getting worse.
Compression stockings are your best friend, even if they're a pain to put on. They provide external pressure that helps those failing valves close more effectively. It’s like giving your veins a supportive hug. Also, elevation is key. Not just putting your feet on a footstool—you need your ankles above your heart.
And move.
Flexing your ankles while sitting, taking a walk every hour, or even just shifting your weight from side to side can drastically reduce the "heavy leg" feeling that usually precedes the visible bulging.
Practical Steps to Take Right Now
If you're worried about what you see in pictures of varicose veins on your own body, don't just wait for it to go away. It won't. Venous disease is progressive.
- Perform a self-check. Use a hand mirror to look at the back of your calves and the inside of your ankles. Check for any skin color changes, specifically browning or redness that doesn't go away.
- Document the changes. Take your own photos every three months. Use the same lighting and the same time of day (evening is best because veins are more prominent after a long day). This gives your doctor a timeline.
- The "Press Test." If you have a bulge, press on it. Does it flatten out easily and then refill when you let go? That's a classic varicose vein. Is the area around it hard or tender? That might indicate a superficial blood clot (phlebitis), which needs medical attention sooner rather than later.
- Evaluate your symptoms. Is it just the look, or do your legs throb? Do you get restless legs at night? Often, treating the underlying vein issues can magically "cure" that annoying "jimmy leg" feeling that keeps you awake.
- Consult a Professional. Find a board-certified vascular specialist. Ask specifically for a "standing ultrasound." If they try to do the ultrasound while you're lying down, find a different doctor—gravity is essential to seeing how the valves actually fail.
Dealing with the reality of pictures of varicose veins on your own legs can be a bit of a wake-up call. It's easy to ignore a dull ache, but it's harder to ignore a physical change in your body. While the aesthetics are what usually drive people into the office, the long-term health of your skin and your circulation is what really matters. Modern treatments are fast, relatively painless, and covered by most insurance if you have symptoms like pain or swelling. There's no reason to just "live with it" anymore.