You’re in the bathroom. The lighting is harsh. Suddenly, you notice a small, brownish-grey smudge on your shoulder that definitely wasn't there last summer. Your first instinct? Grab the phone. You start scrolling through endless pictures of spots on skin online, trying to match your "thing" to a Google Image result. It’s a rabbit hole. Within ten minutes, you’ve convinced yourself it’s either a harmless freckle or a rare, aggressive stage-four melanoma. Honestly, we’ve all been there.
But here is the reality: skin is messy. It’s the body's largest organ, and it doesn't always follow the textbook. A "spot" isn't just a spot; it’s a story written in cells, pigment, and sometimes, sun damage. Doctors call this morphology. To you, it’s just a weird mark that’s making you anxious.
Why matching pictures of spots on skin to your own body is so tricky
Look, the human eye is great, but it’s not a dermatoscope. When you look at high-res medical photos, you're seeing perfect examples. Real life is blurrier. Your skin tone, the lighting in your bedroom, and even your age change how a lesion looks. A seborrheic keratosis—those "barnacles of aging"—can look terrifyingly like a melanoma to the untrained eye. They can be black, crusty, and irregular. But they’re totally benign.
The American Academy of Dermatology (AAD) often talks about the "Ugly Duckling" sign. This is actually more helpful than staring at a thousand clinical photos. Instead of trying to find a twin for your spot online, look at your other spots. Is this one the weirdo? Does it stand out from the rest of your "pattern"? If you have fifty moles and they all look like chocolate chips, but one looks like a squashed raisin, that’s your red flag.
The ABCDEs are just the beginning
Most people know the drill. Asymmetry, Border, Color, Diameter, and Evolving. It’s a solid framework. But it’s not a holy grail.
Let's talk about Color. It’s not just "is it dark?" It’s about variegation. If you see three different shades of brown, a bit of blue-white veil, or a random pinkish hue, that’s when things get interesting for a dermatologist. Dr. Sancy Leachman from the Knight Cancer Institute has often pointed out that melanoma is a master of disguise. It doesn't always look like a scary black spot. Sometimes it’s "amelanotic," meaning it has no pigment at all. It just looks like a persistent pink bump or a scar that won't heal.
✨ Don't miss: How to get over a sore throat fast: What actually works when your neck feels like glass
Actinic Keratosis vs. Basal Cell Carcinoma
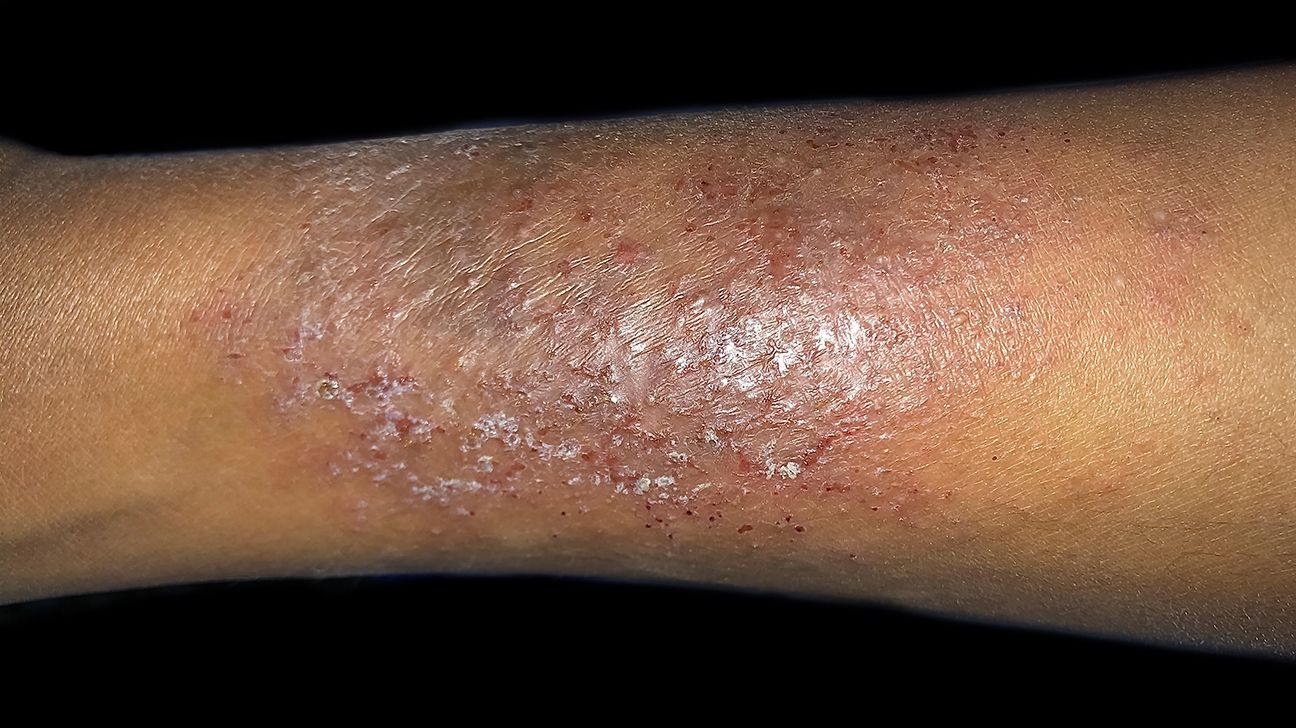
People get these mixed up constantly. Actinic Keratosis (AK) feels like sandpaper. You’ll usually feel it before you see it. It’s precancerous, caused by years of being a "sun worshiper."
Then there’s Basal Cell Carcinoma (BCC). This is the most common skin cancer. It often looks "pearly." Imagine a tiny, translucent pimple that bleeds when you brush it with a towel and never truly goes away. It grows slowly. It rarely spreads to other organs, but it’s a "rodent ulcer"—it eats the tissue around it. If you see a spot that looks like a tiny waxy crater with blood vessels (telangiectasia) spidering across it, stop looking at pictures and go see a pro.
The rise of AI "Symptom Checkers"
We’re in 2026. AI is everywhere. There are apps now where you snap a photo and a machine-learning algorithm tells you your risk level. Are they good? Sorta. Are they perfect? No way.
A study published in The Lancet Digital Health showed that while AI can be incredibly accurate at identifying malignancies in high-quality datasets, it often struggles with "out-of-distribution" images. That means if your photo is slightly out of focus, or if you have a darker skin tone (Fitzpatrick scales IV through VI), the AI might fail. There is a documented bias in medical photography; for decades, textbooks primarily showed pictures of spots on skin on pale, Caucasian individuals. This makes it harder for people of color to find accurate visual references for how skin cancer manifests on deeper pigment, where it might appear as a dark streak in a nail (subungual melanoma) or a patch on the palm or sole of the foot.
Don't ignore the "boring" spots
Everyone worries about the big, dark moles. But sometimes the most dangerous things are the ones that look like a boring rash.
🔗 Read more: How Much Should a 5 7 Man Weigh? The Honest Truth About BMI and Body Composition
Squamous Cell Carcinoma (SCC) can look like a scaly red patch. You might think it’s just eczema or a bit of dry skin that won't quit. But if that "dry patch" stays for two months, it’s not dry skin. It’s a collection of mutated keratinocytes. SCC is more aggressive than Basal Cell, and it actually has the potential to travel to your lymph nodes.
Then you have Cherry Angiomas. Those bright red, cherry-like dots. People freak out thinking it's a blood disorder. Honestly, they’re just overgrowths of blood vessels. They’re harmless. They’re basically the skin’s way of saying, "Congrats, you’re getting older."
When to actually worry (The nuanced view)
Forget the "perfect" pictures for a second. Think about sensation.
Does the spot itch? Does it hurt? Does it "tingle"? While most skin cancers are painless, a spot that suddenly starts acting up—bleeding spontaneously without being picked at—is a major signal.
Also, consider the "History of the Spot." Dermatologists love a good timeline.
💡 You might also like: How do you play with your boobs? A Guide to Self-Touch and Sensitivity
- Did it appear out of nowhere after age 40? (New moles after 40 are suspicious).
- Has it changed shape in the last six weeks?
- Was there a specific "event," like a blistering sunburn in that exact location ten years ago?
The "Invisible" spots
Some spots aren't even on the skin surface you check. We’re talking about the scalp, behind the ears, and between the toes. This is why looking at pictures of spots on skin online is often a fruitless exercise; you’re usually looking at your forearm or thigh, while the real trouble might be hiding in your hair.
I once talked to a guy who found a melanoma because his barber noticed a "weird freckle" near his crown. You can't DIY a scalp exam.
Actionable Next Steps: Beyond the Screen
Stop the "doom-scrolling" through medical galleries. It’s spiking your cortisol and giving you a false sense of security or a false sense of impending doom. Neither is helpful.
- The Monthly Self-Scan: Use a full-length mirror and a hand mirror. Check your back. Use a blow-dryer to move your hair and check your scalp.
- The Mapping Strategy: Take your own photos. Not to compare to the internet, but to compare to yourself. Put a ruler or a coin next to the spot for scale. Take a photo today, then another in a month. If the pixels don't lie and the borders have shifted, you have documented evidence for your doctor.
- Professional Skin Check: If you have a history of sun exposure, see a dermatologist once a year. They use a dermatoscope—a polarized light tool that sees below the top layer of the skin (the epidermis) into the dermis. No iPhone camera can do that yet.
- Sun Protection is Non-Negotiable: If you’re worried about spots, stop making new ones. Use a broad-spectrum SPF 30 or higher. And remember, "base tans" don't protect you; they're just visible evidence of DNA damage.
If a spot is new, changing, or just feels "off," skip the image search. Get it biopsied. A biopsy is the only way to know for sure what's happening at the cellular level. Everything else is just an educated guess.