When you think about "trauma," your brain probably goes straight to a car crash or a war zone. But honestly, that’s such a narrow slice of what human suffering actually looks like. If you've spent any time looking into mental health leadership in the Boston area, you’ve likely bumped into the name Patricia Harney Cambridge Health Alliance.
She isn't just another administrator sitting in a high-backed chair. Dr. Harney is the Director of Psychology Internship Training at CHA and an Assistant Professor at Harvard Medical School. She’s spent decades figuring out how people actually recover from the kind of events that "break" a person. And no, it’s not just about a few weeks of talk therapy.
The Reality of Traumatic Grief
Most of us think grief is a straight line. You’re sad, you cry, you "get over it," right? Wrong.
Dr. Harney’s work—especially her collaboration with the Things They Carry Project—digs into what she calls "traumatic grief." It’s basically grief with a jagged edge. Think about loss that comes from suicide, homicide, or the opioid epidemic. It’s not just blue; it’s a "deeper shade of blue" because it’s mixed with horror and shame.
She often talks about how the "red pigment" of trauma changes the whole palette of the experience. You can’t treat a mother who lost a son to an overdose the same way you treat someone whose elderly grandfather passed away peacefully. The biology of the brain is different. The social stigma is different.
Why Her Work at Cambridge Health Alliance Actually Matters
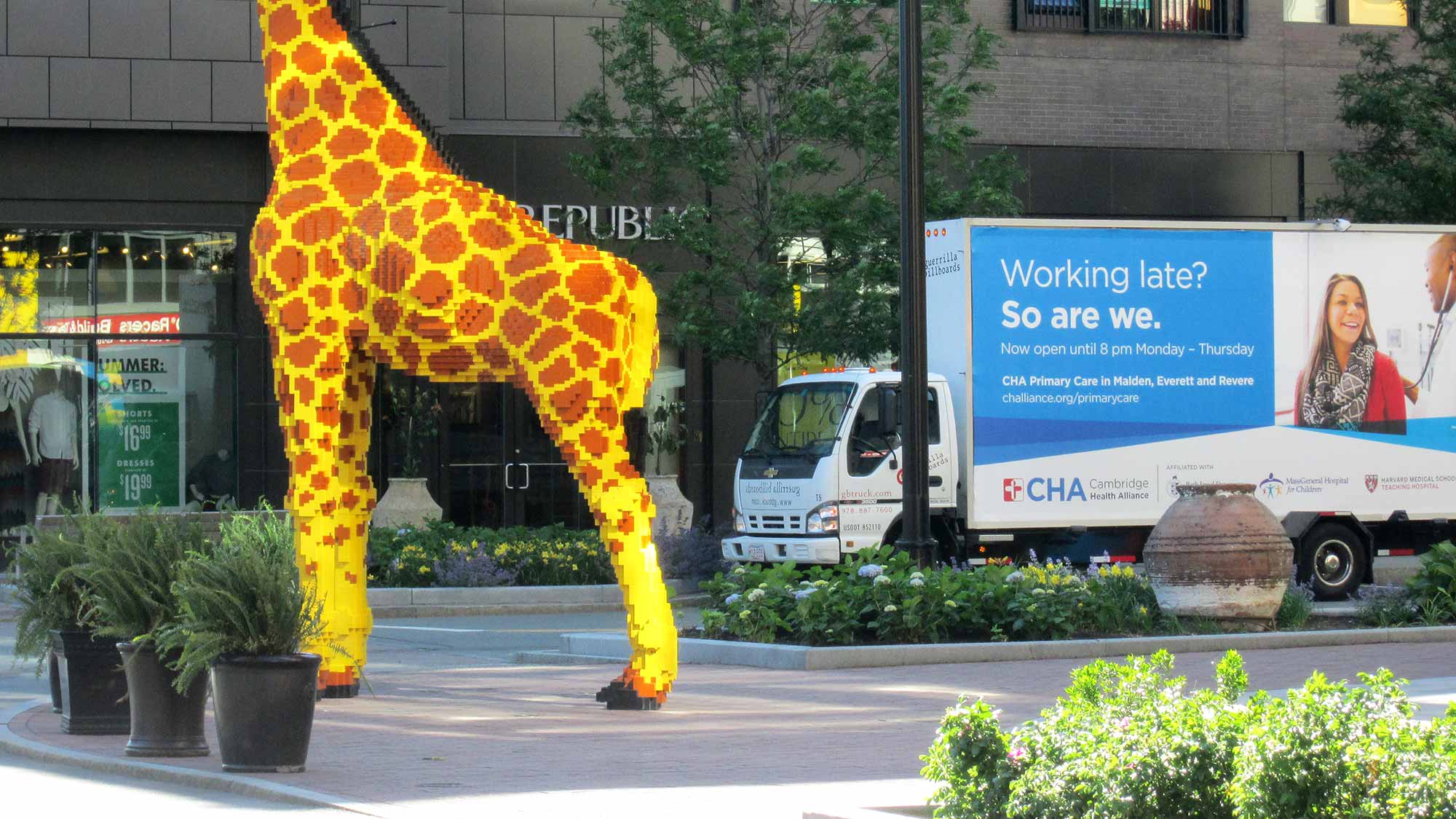
Cambridge Health Alliance (CHA) isn't your typical shiny, corporate hospital. It’s a safety-net system. This means Dr. Harney and her team are working with people from every imaginable background—immigrants, survivors of domestic violence, folks struggling with poverty.
She’s currently the Acting Co-Chief of Psychology at CHA. In a world where mental health care is becoming increasingly "McDonaldized" (quick, cheap, and standardized), Harney pushes for something called the collaborative treatment relationship.
- It’s about more than just checking boxes.
- She looks at the "intersectionality" of identity—how being LGBTQ+ or a person of color changes the way you process trauma.
- She advocates for long-term care in an era that wants everything fixed in six sessions.
The Human Behind the Ph.D.
It’s easy to look at a Harvard faculty bio and see a robot. But Patricia Harney is kind of an outlier. She’s a violinist with the Longwood Symphony Orchestra. She’s a writer who’s been published in Slate and WBUR.
She’s currently working on a memoir called Grief in the Margins. That title says a lot. It’s about the people who don't fit into the "normal" boxes of recovery.
I think we often forget that the people teaching the next generation of psychologists are, well, people. During the 2020 lockdowns, she was out there talking about "coffee meditation" and the power of vulnerability. She didn't pretend everything was fine. She talked about the struggle of helping patients through a screen while the world felt like it was ending.
What Most People Miss About Trauma Recovery
People love the word "resilience." It’s a buzzword. But Harney’s research, like her work on the Multidimensional Trauma Recovery and Resiliency Scale, shows that resilience isn't a personality trait you’re born with. It’s a process.
It’s about:
- Connection: Isolation is the enemy of recovery.
- Narrative: Being able to tell your story without it shattering you.
- Safety: Not just physical safety, but the emotional safety of being seen.
She’s been a massive proponent of group therapy. Why? Because trauma makes you feel like you’re the only person on a deserted island. A group proves you aren’t. It acts as an "ecological bridge" back to the community.
Actionable Insights for Your Own Path
If you’re looking into the work of Patricia Harney Cambridge Health Alliance because you’re struggling or you’re a clinician, here’s the "so what" of her philosophy:
🔗 Read more: Caffeine Hair Growth: Why Smearing Coffee on Your Head Actually Works (According to Science)
- Acknowledge the "Shade": If your grief feels heavier than "normal" grief, it probably is. Stop comparing your timeline to others.
- Find Your "Bridge": Don’t try to heal in a vacuum. Whether it’s a support group, a musical ensemble, or a long-term therapist, you need a witness.
- Watch for Shame: Harney’s research highlights how shame acts as a barrier to healing, especially in marginalized communities. If you’re feeling "wrong" for how you feel, that’s the trauma talking, not the truth.
Dr. Harney’s career reminds us that mental health isn't a destination. It’s more like tuning an instrument. It takes practice, it’s often frustrating, and sometimes you need a teacher to show you how to find the right note again.
Practical Next Steps
- Check out the CHA Continuing Education portal: If you're a professional, look for her course on "Traumatic Grief." It covers the specifics of loss via suicide, homicide, and overdose.
- Read her essays on WBUR's Commonhealth: She writes specifically about how to handle difficult family conversations and the intersection of politics and mental health.
- Look into the Things They Carry Project: This is a great resource if you're interested in how writing and creativity can help process professional burnout and personal trauma.