It’s 3:00 AM. You’re staring at the ceiling, wondering why your abdomen feels like it’s hosting a tiny, angry construction crew. Dealing with pain in middle of stomach at night is a uniquely frustrating experience because it steals the one thing you need to recover—sleep. It’s localized, it’s persistent, and honestly, it’s often a bit scary when the rest of the house is silent.
Most people assume it’s just that late-night taco. Sometimes it is. But when the discomfort centers itself right in that "V" where your ribs meet, or just above the belly button, your body is usually signaling something more specific than general indigestion.
The anatomy of that midnight ache
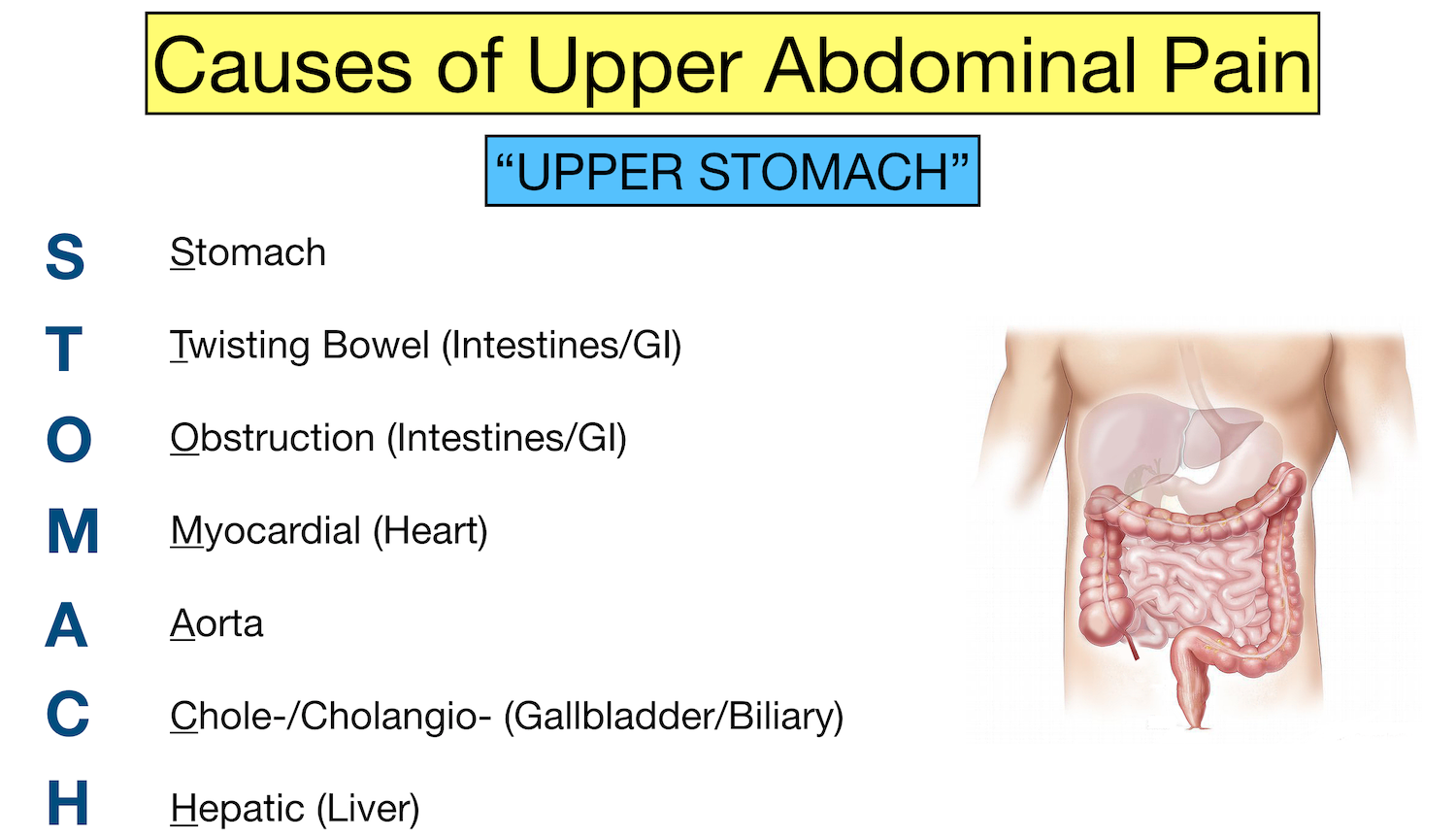
The "middle" of your stomach is prime real estate for several major organs. In medical speak, we call this the epigastric region. It houses the pancreas, the stomach itself, and the beginning of the small intestine (the duodenum). When you lie down, gravity stops helping your digestive system.
Everything flattens out.
If you have excess acid, it doesn’t just sit in the bottom of your stomach; it creeps up. This is why Gastroesophageal Reflux Disease (GERD) is the most common culprit for nocturnal distress. According to the American College of Gastroenterology, nearly 60 million Americans experience heartburn at least once a month. At night, without the benefit of being upright, that acid irritates the lining of the esophagus, causing a gnawing or burning pain right in the center.
But GERD isn't the only player.
📖 Related: Why the 45 degree angle bench is the missing link for your upper chest
When it’s more than just "heartburn"
Sometimes the pain isn’t a burn; it’s a dull, boring ache that feels like it’s drilling through to your back. This can be a sign of Peptic Ulcer Disease. Interestingly, ulcers often feel worse when the stomach is empty. Nighttime is the longest stretch your stomach goes without food, allowing gastric acid to bathe the open sore in your stomach lining or duodenum.
Dr. Brennan Spiegel, a gastroenterologist at Cedars-Sinai, has noted in his research that the "brain-gut" connection is also hyper-sensitive at night. When external distractions are gone, your brain amplifies the signals coming from your enteric nervous system.
- Gastritis: This is basically an inflamed stomach lining. It can be triggered by NSAIDs (like Ibuprofen or Aspirin) taken on an empty stomach before bed.
- Biliary Colic: While gallbladder pain is often on the right side, it can radiate to the center. It usually hits a few hours after a heavy, fatty meal—right around bedtime.
- Pancreatitis: This is the heavy hitter. If the pain is intense, centered, and feels slightly better when you lean forward in bed, the pancreas might be inflamed. This isn't a "wait and see" situation; it's an ER situation.
The role of the "Sleeping Position" factor
How you sleep actually matters.
If you’re a right-side sleeper, you might be accidentally encouraging that pain in middle of stomach at night. The way the stomach is shaped, sleeping on your right side places the "trap door" of the esophagus (the lower esophageal sphincter) below the level of stomach acid. This makes it incredibly easy for acid to leak out.
Left-side sleeping is the gold standard here. It keeps the junction between the stomach and esophagus above the "acid pool." It sounds like a small tweak. It isn't. It can be the difference between a full REM cycle and a night spent clutching a heating pad.
👉 See also: The Truth Behind RFK Autism Destroys Families Claims and the Science of Neurodiversity
Does it matter what you ate?
Basically, yes. But it’s not just "spicy food."
Chocolate, caffeine, and alcohol all relax that lower esophageal sphincter. You might think a nightcap helps you drift off, but it’s actually a chemical green light for stomach acid to move north. Then there’s the volume of food. A massive meal stretches the stomach, increasing pressure. When you combine high pressure with a horizontal body position, you’re asking for a rough night.
When to actually worry
We all get stomach aches. It's part of being human and occasionally eating things we shouldn't. However, there are "red flag" symptoms that mean your pain in middle of stomach at night isn't just a slow digestion issue.
If the pain is accompanied by unintentional weight loss, difficulty swallowing, or if you’re seeing what looks like coffee grounds in your vomit (that’s old blood), you need a doctor. Yesterday. Also, if the pain is so sharp it takes your breath away, or if your abdomen feels "board-stiff" to the touch, that can indicate a perforation—an actual hole in the digestive tract.
Actionable steps for tonight (and tomorrow)
If you’re reading this while currently hurting, try these immediate adjustments.
✨ Don't miss: Medicine Ball Set With Rack: What Your Home Gym Is Actually Missing
Elevate, don’t just stack.
Don't just put more pillows under your head; that just kinks your neck. You need to elevate your entire torso. Use a wedge pillow or put bricks under the head of your bed frame. You want an incline of at least 6 to 8 inches. Gravity is your only friend here.
The Ginger Trick.
If the pain feels like nausea or "heaviness," real ginger tea (not the sugary soda) can speed up "gastric emptying." The faster your stomach moves its contents into the small intestine, the less pressure there is to cause pain.
Check your meds.
Are you taking Ibuprofen for a headache before bed? Stop. Switch to Acetaminophen (Tylenol) if you have stomach sensitivity, as NSAIDs are notorious for eating away at the stomach's protective mucus layer.
The 3-Hour Rule.
This is the hardest one for most of us. Stop eating three hours before your head hits the pillow. Your stomach needs time to do the heavy lifting of digestion while you’re still vertical.
Track the patterns.
Keep a "pain log" on your nightstand. Does it happen after pasta? After a stressful day? When you’ve skipped lunch? Patterns are the only way a doctor can accurately diagnose things like Gastroparesis or Functional Dyspepsia.
Ultimately, pain in middle of stomach at night is a puzzle. It’s rarely a single "event" and usually a combination of lifestyle, anatomy, and timing. Start with the left-side sleeping and the three-hour fasting rule. If the gnawing persists for more than two weeks, it’s time for an endoscopy to see what’s actually happening under the hood.