It happens in a split second. You’re sitting on the couch, maybe scrolling through your phone, and suddenly there’s this sharp, stabbing sensation or a dull, heavy pressure right there. Your brain immediately goes to the worst-case scenario. You start thinking about emergency rooms and life insurance. Most people assume pain around heart area equals a heart attack. Full stop. But honestly? The human chest is a crowded neighborhood. Between your ribs, your lungs, your esophagus, and your actual heart, there are dozens of things that can go wrong that have absolutely nothing to do with a cardiac event.
I’ve seen people come into clinics white as a sheet, convinced they’re dying, only to find out they just had a particularly nasty case of acid reflux or a pulled muscle from yesterday’s gym session. It’s scary. I get it. The proximity to your literal engine makes every twinge feel like a five-alarm fire. But understanding the nuance of this discomfort is basically the difference between a night of unnecessary panic and knowing when to actually grab your keys and drive to the ER.
The Anxiety-Acid-Ache Triangle
Sometimes, the body plays tricks on you. You've probably heard of "Precordial Catch Syndrome." It’s this weird, sharp pain—usually in younger people—that feels like a needle stabbing you right in the chest when you take a breath. It’s harmless. Totally benign. But if you don’t know that, it feels like your heart is failing.
Then there’s the GI track. Your esophagus sits right behind the heart. When stomach acid creeps up, it causes "heartburn," which is perhaps the most poorly named medical condition in history. It doesn't affect the heart, but the burning sensation can be so intense it mimics stable angina. Dr. Marcelo Vela at the Mayo Clinic has noted that esophageal spasms can be nearly indistinguishable from heart pain because they use the same nerve pathways to signal the brain. Your brain just gets a "pain" signal from "somewhere in the chest" and panics.
Stress makes it worse. High cortisol levels can tighten the intercostal muscles—those tiny muscles between your ribs. When those tighten up, every breath feels restricted. You start shallow breathing, which leads to more anxiety, which leads to more chest tightness. It’s a vicious cycle that lands thousands of people in the hospital every year for what turns out to be a panic attack.
When Pain Around Heart Area is Actually Skeletal
Ever heard of Costochondritis? It sounds like a scary tropical disease, but it’s actually just inflammation of the cartilage that joins your ribs to your breastbone. If you can press on your chest with your finger and the pain gets worse, it’s almost certainly not your heart. Heart pain is visceral; it’s deep. You can't "touch" it from the outside.
📖 Related: The Human Heart: Why We Get So Much Wrong About How It Works
- Muscle Strains: Did you do chest day? Or maybe just move some heavy boxes? The pectoralis major can mimic deep pressure.
- Rib Injury: Even a slight hairline fracture or a bruised rib can cause radiating pain that feels like it's coming from inside the chest cavity.
- Pleurisy: This is when the lining of your lungs gets inflamed. It’s a sharp, knife-like pain that usually gets way worse when you cough or sneeze.
There’s also the "referred pain" factor. Sometimes, problems in your gallbladder or pancreas can radiate upwards. It’s like a short circuit in the body’s wiring.
The "Red Flags" You Can't Ignore
Look, I’m not saying you should blow it off. While most pain around heart area is musculoskeletal or digestive, the stakes are too high to be reckless. There are specific "quality" markers of cardiac pain that should trigger an immediate 911 call.
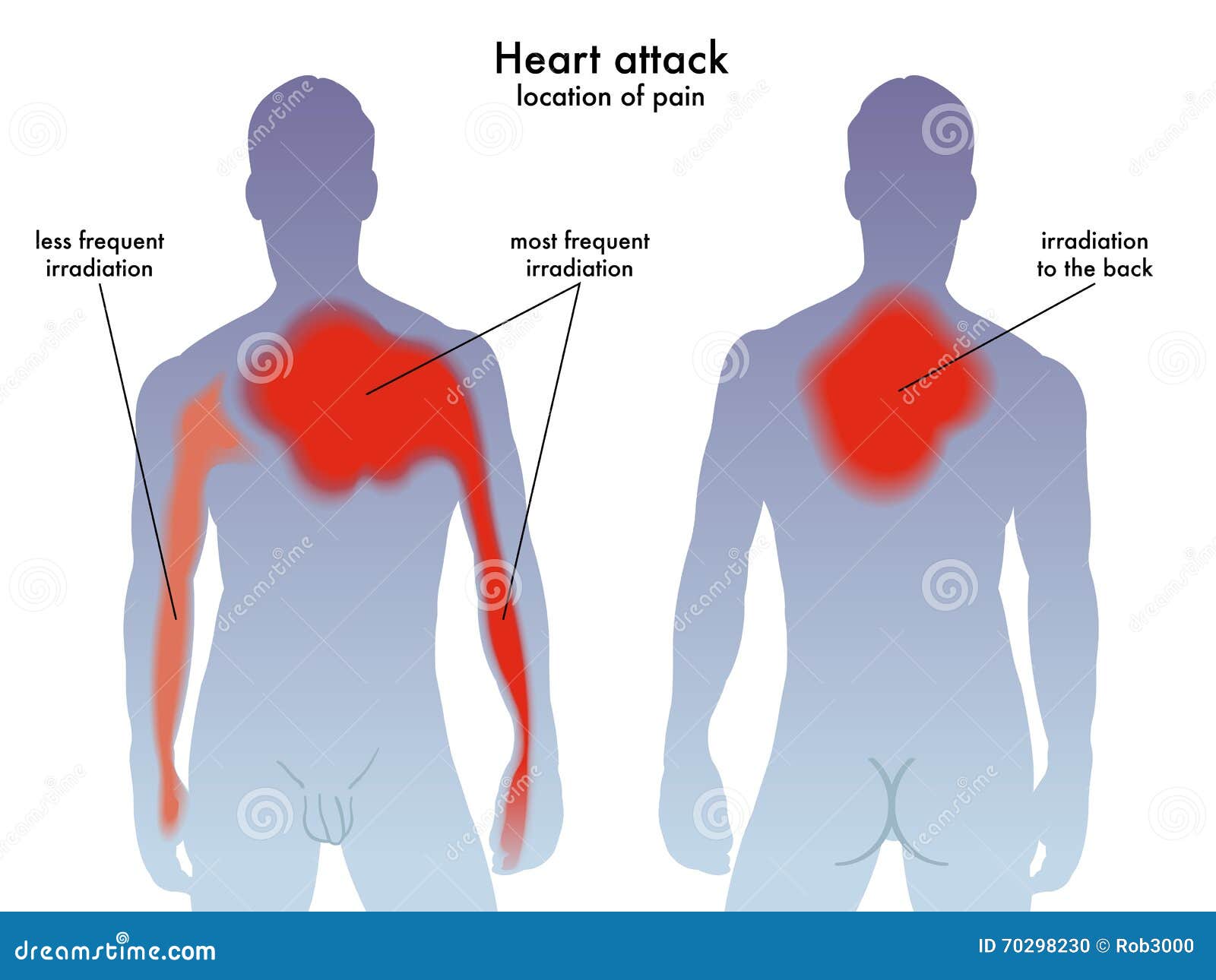
True cardiac distress—specifically a myocardial infarction—often doesn't feel like "pain" in the way a cut or a bruise does. Patients frequently describe it as a "heaviness" or an "elephant sitting on my chest." If the discomfort radiates into your left arm, your jaw, or between your shoulder blades, that’s a massive warning sign. Also, watch for the "silent" symptoms. If you’re sweating profusely (diaphoresis) without exercising, or if you feel a sense of "impending doom," your body is telling you something is critically wrong.
Women often experience this differently. Instead of the "Hollywood Heart Attack" clutching of the chest, women might just feel incredibly fatigued, nauseated, or have a weird ache in their upper back. According to the American Heart Association, these subtle signs often lead to women waiting longer to seek help, which is dangerous.
The Role of Stable vs. Unstable Angina
If you notice the pain only happens when you’re walking up stairs or exerting yourself, and then it disappears the moment you sit down, that’s often stable angina. It means your heart isn't getting quite enough oxygenated blood during high demand. It’s a "warning light" on the dashboard. Unstable angina is the one that happens while you're resting—that's an emergency.
👉 See also: Ankle Stretches for Runners: What Most People Get Wrong About Mobility
Diagnostic Nuance: What Happens at the Doctor
When you finally go in, they aren't just going to guess. They’ll likely start with an EKG (electrocardiogram). It’s a simple test that looks at the electrical rhythm of your heart. If there’s a blockage or an old scar from a previous "silent" attack, the EKG will usually show it.
They might also run a Troponin test. Troponin is a protein released into the bloodstream when the heart muscle is damaged. If your levels are elevated, it's a definitive sign that the heart is under duress. But even these aren't foolproof. Some people have "false positives" due to kidney issues or extreme endurance exercise (like running a marathon). This is why doctors look at the whole picture—your blood pressure, your history, and how the pain actually feels.
Moving Beyond the Fear
Living in fear of every chest twinge is exhausting. It ruins your quality of life. If you’ve been cleared by a doctor but still feel that pain around heart area, it might be time to look at lifestyle factors that trigger inflammation or esophageal distress.
The "Western Diet" is a major culprit. Highly processed foods lead to systemic inflammation and frequent acid reflux. Switching to an anti-inflammatory protocol—think Mediterranean style with lots of olive oil, leafy greens, and fatty fish—can sometimes "cure" chest pain that was actually just chronic indigestion. Also, check your posture. We spend so much time hunched over laptops that our chest muscles literally shorten, pulling on the rib cage and causing—you guessed it—chest pain.
Real Actions You Can Take Right Now
Stop googling your symptoms for three hours. It only spikes your heart rate and makes the pain worse. If you are currently experiencing discomfort and you're unsure, follow these steps:
✨ Don't miss: Can DayQuil Be Taken At Night: What Happens If You Skip NyQuil
- The "Press Test": Use two fingers to press firmly on the spot where it hurts. If the pain is localized and changes when you press it, it’s likely musculoskeletal.
- The "Breath Test": Take a deep, lung-expanding breath. If the pain is a sharp "catch" that happens only at the peak of the breath, it’s often pleuritic or nerve-related, not a heart attack.
- The "Antacid Trial": If you have a burning sensation, take an over-the-counter antacid. If the pain vanishes in 15 minutes, you’ve found your culprit: the esophagus.
- Check Your Pulse: Is it regular? If your heart is skipping beats or racing at 150 BPM while you're sitting still, that warrants a professional check-up regardless of the pain level.
Schedule a stress test. If you're worried about your heart health, don't wait for an emergency. A proactive stress test can show how your heart handles work in a controlled environment. This provides a baseline of data that can offer immense peace of mind.
Monitor your "Trigger Foods." Keep a simple log for one week. Note when the chest discomfort happens. You might find a direct correlation between that third cup of coffee or that spicy late-night taco and the "heart pain" that’s keeping you up at night.
Improve your thoracic mobility. Incorporate "doorway stretches" to open up your chest. Stand in a doorway, place your forearms on the frame, and lean forward. This releases the pectoralis minor, which, when tight, can cause radiating pain that feels alarmingly like a cardiac issue.
Get a blood panel for inflammation markers. Ask your doctor to check your C-Reactive Protein (CRP) levels. This gives you a snapshot of the general inflammation in your body, which can be a precursor to both joint pain and arterial issues. Knowledge is the best tool against the anxiety of the unknown.