If you live in a town where the nearest Walmart is a forty-minute drive, you already know the vibe. Things are just further away. But there is a massive difference between driving an hour for a flat-screen TV and driving an hour because your chest feels tight and you can't breathe.
Honestly, the number of rural hospitals United States 2024 data paints a picture that's kinda bleak if you just look at the raw totals. We are looking at roughly 1,796 to 1,810 rural community hospitals left standing, depending on which federal ledger you’re checking. That sounds like a lot until you realize that over 600 of them are essentially on life support.
I’ve spent a lot of time looking at these maps. It’s not just a "small town problem." It is a "how do we survive as a country" problem. When a rural hospital vanishes, the pharmacy usually goes next. Then the doctors leave. Then the young families move. Basically, the whole town's pulse slows down.
Why the 2024 Count Feels Different
In 2024, we saw a weird stabilization that isn't actually stable. It’s more like a "pause" button was hit. During the pandemic, the federal government dumped a lot of cash into the system to keep doors open. That money is mostly gone now.
According to the American Hospital Association (AHA), the total count of rural community hospitals hit 1,796 in their latest 2025 report (which covers the 2023-2024 data cycle). This is a slight dip from the 1,810 reported just a year prior. It doesn’t seem like a "collapse" on paper. But numbers are funny. They hide the "conversions."
See, a lot of hospitals didn't technically "close"—they just stopped being hospitals. They became "Rural Emergency Hospitals" (REHs) or clinics. They don't have beds anymore. You can't stay overnight. If you’re really sick, they stabilize you and put you in an ambulance for a two-hour ride to the city. Is it a hospital? Technically, no. Is it better than a locked door? Sorta.
💡 You might also like: Barras de proteina sin azucar: Lo que las etiquetas no te dicen y cómo elegirlas de verdad
The Financial Cliff Nobody is Talking About
The Center for Healthcare Quality and Payment Reform (CHQPR) dropped some heavy data earlier this year. They found that over 700 rural hospitals are at risk of closing soon.
- 300 of those are at "immediate risk."
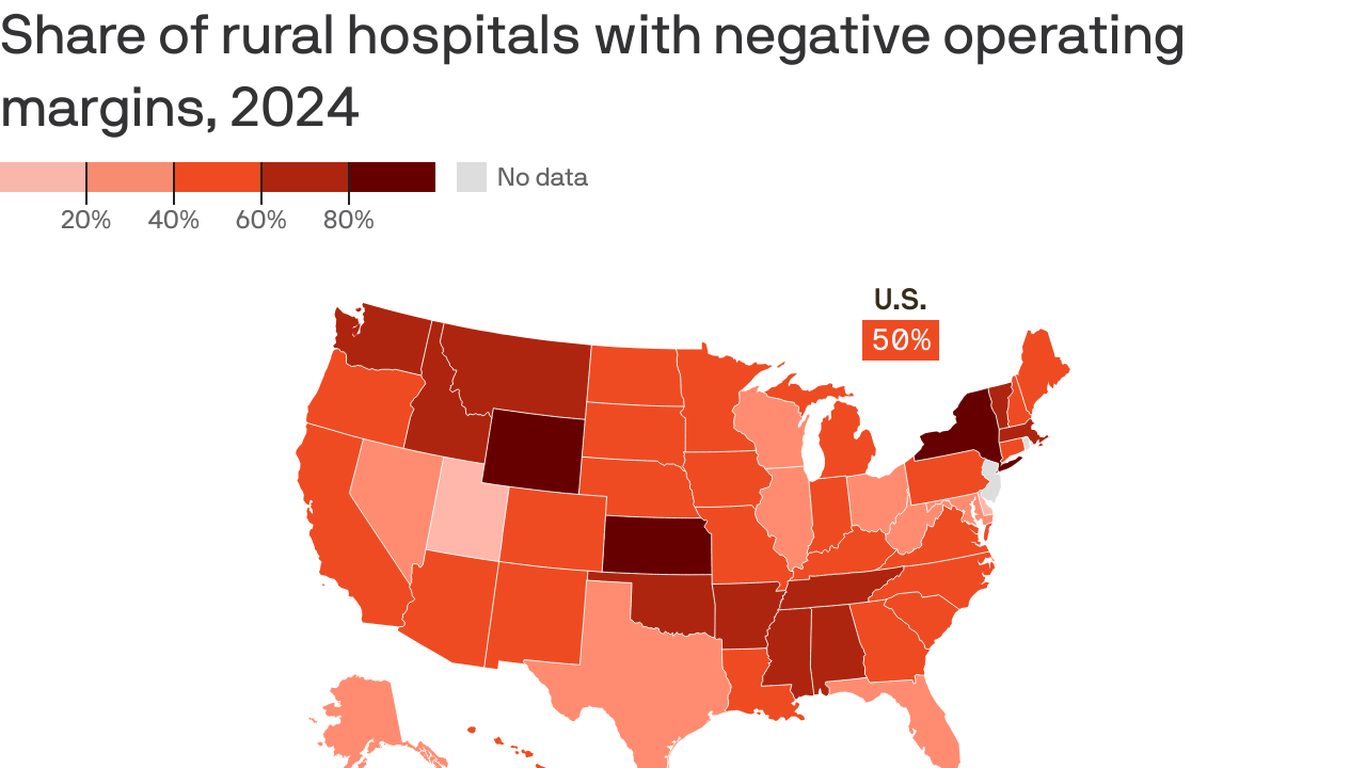
- 50% of rural hospitals in states like Alabama and Mississippi are operating with negative margins.
- 120 hospitals have stopped delivering babies since 2020 because they can't afford the liability insurance or the staff.
It’s expensive to keep a light on in a building where only five people might walk in during a Tuesday afternoon. But those five people still deserve to live.
Where Have All the Hospitals Gone?
If you look at the Sheps Center data from UNC, you’ll see the "Closing Belt." It’s mostly the South and the lower Midwest. Texas, Tennessee, Georgia—these states have been hit the hardest.
Why? It’s a mix of things. Medicaid expansion (or the lack of it) is a huge factor. In states that didn't expand Medicaid, hospitals end up eating the cost of "uncompensated care." Basically, people show up, get treated, can't pay, and the hospital just takes the loss. You can only do that for so many years before the bank comes for the keys.
The "System" Solution (That Might Not Work)
Lately, big health systems have been gobbling up small rural spots. On the surface, it’s a win. The big guys bring money, better tech, and more doctors. But honestly, it can feel like a corporate takeover. Suddenly, the local board is replaced by executives three states away. If the "satellite" hospital isn't profitable, they cut the most expensive services—like labor and delivery or oncology.
📖 Related: Cleveland clinic abu dhabi photos: Why This Hospital Looks More Like a Museum
A report from the Coalition to Strengthen America’s Healthcare found that 2 in 3 hospitals at high risk of closing were saved by joining a system. That’s a great stat. But for the person in labor who now has to drive 80 miles to a "sister facility," it doesn't feel like a win.
The Human Cost of a Number
Let's get real for a second. We talk about the number of rural hospitals United States 2024 like it's a math problem. It's not.
When a hospital closes, the travel time for emergency care increases by an average of 20 to 30 minutes. In a stroke or a heart attack, that is the difference between going home or going to a funeral. Rural residents are already older, sicker, and poorer than their urban counterparts. They have higher rates of diabetes and heart disease. They literally need more care, yet they have the least access to it.
What's Actually Being Done?
There are some glimmers of hope.
- Rural Emergency Hospital (REH) Designation: This is a new federal category that gives small facilities more money if they give up their inpatient beds but keep their ER open.
- Telehealth: It’s not a replacement for a surgeon, but it helps. You can see a specialist in Chicago from a clinic in rural Nebraska.
- The Rural Hospital Support Act: There is constant pressure in D.C. to make some of the pandemic-era payment bumps permanent.
But these are bandages on a pretty deep wound.
👉 See also: Baldwin Building Rochester Minnesota: What Most People Get Wrong
Actionable Steps for Rural Residents
If you’re worried about your local hospital, you aren't powerless.
First, check the status. Visit the Sheps Center website or CHQPR to see the financial "risk rating" of your local facility. Knowledge is power.
Second, use the services. It sounds simple, but hospitals need "volume." If you go to the city for every blood test or X-ray because it feels "fancier," you’re taking revenue away from the place that will have to save your life during a midnight car accident.
Third, get loud. Hospital boards and state legislators respond to pressure. If they know the community is watching the "conversion" or "merger" talks, they are less likely to let the facility just fade away.
The number of rural hospitals United States 2024 is more than just a statistic. It’s a map of where we value human life and where we don't. We have the 1,796 facilities left—the goal now is making sure that number doesn't hit zero for the towns that need them most.