You’re sitting on the couch, maybe scrolling through your phone, when you suddenly feel it. That little thump-thump in your chest. You check your smartwatch. It says 78. Or maybe 54. Or 92. Suddenly, you're spiraling. Is that high? Is it low? Why does your neighbor’s watch say 50 while yours is humming along at 80?
Honestly, the normal resting heartbeat rate is one of those health metrics that seems straightforward until you actually look at the data. Most people think there’s one "perfect" number. There isn't.
If you’ve ever looked at a medical textbook, you've seen the standard range: 60 to 100 beats per minute (bpm). But that range is kind of a massive catch-all. It’s the medical equivalent of saying a "normal" height for an adult is anywhere between 4'10" and 6'8". While technically true for the population, it doesn’t tell you much about your specific health.
Your heart is a pump. It’s a muscle. And like any muscle, its efficiency depends on a hundred different variables ranging from how much coffee you drank at 9:00 AM to whether you’re secretly coming down with a cold you haven't felt yet.
The 60-100 Myth and Why It’s Shifting
For decades, the American Heart Association and the Mayo Clinic have stuck to that 60-100 bpm window. It’s safe. It’s easy to remember. But if you talk to modern cardiologists, many will tell you that the "top end" of that range is actually a bit concerning.
Recent large-scale longitudinal studies have suggested that people consistently at the higher end of "normal"—say, 80 to 100 bpm—actually face higher risks of cardiovascular issues compared to those in the 60s and 70s. A study published in the journal Open Heart tracked men for over a decade and found that those with a resting heart rate of 75 bpm or higher were at a significantly increased risk of premature death compared to those with lower rates.
So, is 90 bpm "normal"? Technically, yes. Is it optimal? Probably not.
Athletes and the Low-End Exception
Then you have the other side of the coin. If your heart rate dips to 48 bpm, a standard hospital monitor might start beeping. But if you’re a marathon runner or a serious cyclist, that 48 bpm is a badge of honor. It’s called athletic bradycardia. When your heart muscle is incredibly strong, it pumps a larger volume of blood with every single squeeze (increased stroke volume), so it doesn't need to beat as often.
👉 See also: How to get more magnesium in my diet: Why most people are still missing the mark
Miguel Induráin, a five-time Tour de France winner, famously had a resting heart rate of 28 bpm. For a "normal" person, that’s a medical emergency. For him, it was peak efficiency.
What Actually Changes Your Number?
It’s not just about "fitness." Your normal resting heartbeat rate is a living, breathing metric.
Temperature is a big one. When it’s sweltering outside, your heart has to work harder to radiate heat away from your core, which can bump your resting rate up by 10 or 15 beats. Dehydration does the same thing. If your blood volume drops because you haven't had enough water, your heart has to beat faster to maintain blood pressure. It's simple physics.
Emotional state is the "silent" variable. You might feel calm, but if you’re stressed about a deadline, your sympathetic nervous system is likely leaking a little adrenaline into your system. That keeps your baseline higher than it would be on a Sunday morning.
The Role of Age and Sex
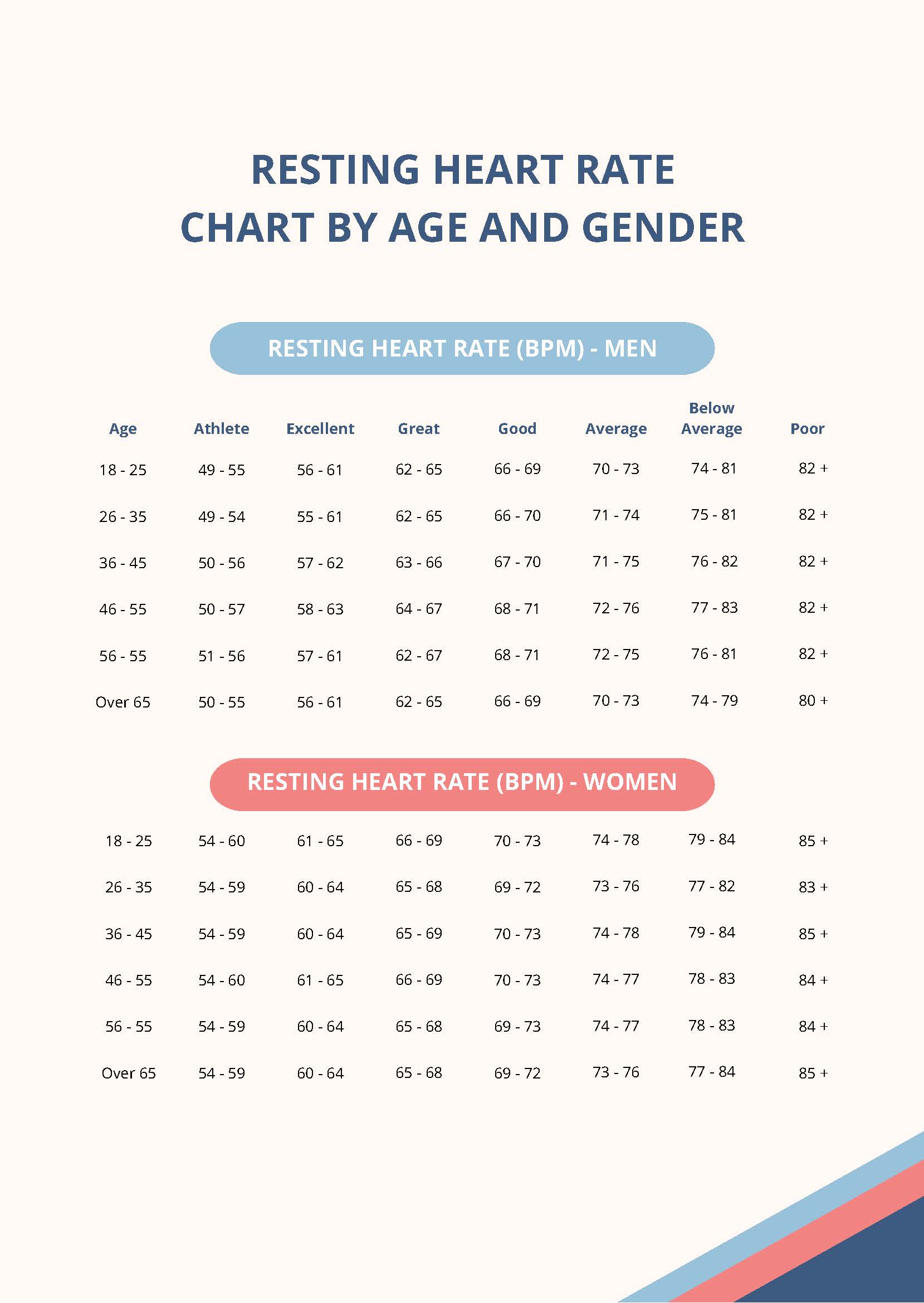
Biologically, women tend to have slightly higher resting heart rates than men. This isn't a sign of being less fit; it’s mostly due to the fact that women generally have smaller hearts, which need to beat a bit more frequently to move the same amount of blood.
Age also plays a weird role. While you might think your heart slows down as you get older, your resting rate actually stays fairly stable throughout adulthood. What does change is your maximum heart rate. You lose that "top gear" as the electrical pathways in the heart age.
When Should You Actually Worry?
We spend a lot of time obsessing over numbers, but symptoms matter more than the readout on your Fitbit.
💡 You might also like: Cherry Hill Health and Racquet Club: Why This Massive NJ Complex Still Dominates
If your heart rate is 105 but you feel totally fine, you might just be stressed or over-caffeinated. However, if your heart rate is 90 and you feel dizzy, short of breath, or like your heart is "flopping" in your chest (palpitations), that’s when it moves from "variation" to "problem."
Tachycardia is the medical term for a rate over 100. Bradycardia is the term for a rate under 60. Neither is a diagnosis on its own; they are just descriptions of what the heart is doing. The context is everything.
Surprising Things That Spike Your Rate
- Lack of sleep: Even one night of poor sleep can keep your resting rate elevated the next day.
- Alcohol: "Holiday Heart Syndrome" is a real thing where binge drinking triggers irregular rhythms and high rates.
- Thyroid issues: An overactive thyroid (hyperthyroidism) acts like a gas pedal for your heart.
- Medications: Over-the-counter decongestants are notorious for sending heart rates skyrocketing.
How to Get an Accurate Measurement
Most people check their heart rate wrong. They check it after walking from the kitchen, or right after an annoying email. To find your true normal resting heartbeat rate, you need to be "true" resting.
Do it first thing in the morning. Before you get out of bed. Before you check your phone and see the news. Put two fingers (not your thumb, which has its own pulse) on your wrist just below the base of the thumb. Count the beats for 30 seconds and multiply by two.
Do this for three days. The average of those three mornings is your baseline. Everything else throughout the day is just a reaction to your environment.
📖 Related: Philips Sonicare DiamondClean Smart: Why Most People Use This $300 Brush Completely Wrong
The Smartwatch Trap
Technology is a double-edged sword. We have more data than ever, but we aren't always better at interpreting it. Optical heart rate sensors (the green lights on the back of your watch) are generally good at resting rates, but they can be tricked. If the band is loose, or if you have dark tattoos on your wrist, or even if you have cold skin (vasoconstriction), the reading can be off.
Don't let a single weird reading on a watch ruin your day. If the watch says 110 but you feel 60, trust your body, not the sensor.
Actionable Steps for Heart Health
If you’ve found that your resting rate is consistently higher than you'd like (e.g., sticking in the mid-80s or 90s), there are concrete ways to bring it down over time. It’s not about a quick fix; it’s about changing the "setting" of your nervous system.
- Prioritize Zone 2 Cardio: This is low-intensity exercise where you can still hold a conversation. Think brisk walking or light cycling. It strengthens the heart's chambers and increases stroke volume more effectively for resting rate reduction than high-intensity sprinting.
- Magnesium and Potassium: These electrolytes are the "brakes" for your heart's electrical system. Many people are chronically low in magnesium, which can lead to a "touchy" or fast heart rate.
- Vagal Tone Exercises: Your vagus nerve is the primary component of the parasympathetic nervous system (the "rest and digest" system). Deep, diaphragmatic breathing—specifically where the exhale is longer than the inhale—directly signals the heart to slow down.
- Audit Your Stimulants: It sounds obvious, but many people don't realize that the "pre-workout" powder or the third cup of coffee has a half-life. Caffeine can stay in your system for 6-8 hours, keeping your resting rate elevated even while you sleep.
- Consistent Hydration: Aim for half your body weight in ounces of water daily. A hydrated heart is a relaxed heart because the blood is easier to move.
Keep a log of your morning heart rate once a week. If you see a sudden, sustained jump of 10 bpm or more that lasts for several days without an obvious cause (like a hard workout the night before), it’s often the first sign that your body is fighting off an infection or that you are severely overtraining. Use the number as a tool, not a source of anxiety.