You’re sitting on the couch, scrolling through your phone, and suddenly your wrist buzzes. You look down. Your heart rate is 58 beats per minute. Yesterday it was 72. Now you're wondering if you’re dying or if you’ve somehow become an elite marathon runner overnight. Most of us treat the normal pulse rate like a fixed speed limit, but your heart isn't a machine following a manual. It's more like a jazz musician—improvising constantly based on what’s happening in the room.
The truth is, "normal" is a massive, frustratingly vague range. Doctors usually tell you it’s between 60 and 100 beats per minute (bpm). But honestly? That range was established decades ago, and it doesn't account for the fact that a 25-year-old barista and a 70-year-old grandmother have very different biological realities. If your heart is beating at 95 bpm while you're just watching Netflix, you're technically "normal," but you might actually be incredibly stressed or dehydrated.
Context matters more than the number.
The 60-100 Myth and What Science Actually Says
For years, the medical establishment has leaned on the 60 to 100 bpm standard for a resting heart rate. It’s easy to remember. It’s clean. But recent data suggests we should probably be looking at a narrower window for true cardiovascular health. A massive study published in Open Heart tracked middle-aged men for a decade and found that those with a resting heart rate at the higher end of the "normal" spectrum—specifically above 75 bpm—had a higher risk of premature death compared to those in the 50s or 60s.
So, if 100 is the ceiling, why is 76 considered a potential warning sign? It’s because a high resting pulse often means your heart is working harder than it needs to. Imagine a car idling at 3,000 RPMs while parked. It’s going to wear out the engine faster than a car idling at 800 RPMs.
Your heart is a muscle. Like any muscle, efficiency is the goal.
Athletes often have a normal pulse rate that would make a triage nurse panic. Miguel Induráin, the legendary cyclist, reportedly had a resting heart rate of 28 bpm. For a regular person, that's a trip to the emergency room for a pacemaker. For him, it was a sign of a heart so powerful it could move massive amounts of oxygenated blood with a single, lazy thud.
🔗 Read more: How to Puke Quietly Without Everyone Noticing
Why Your Number Jumps Around Like Crazy
It’s almost never static. You take a sip of espresso? Up it goes. You have a stressful thought about your taxes? Spike. You’re slightly dehydrated because you haven't drank water since 10:00 AM? Your heart speeds up to compensate for the lower blood volume.
Temperature plays a huge role too. When you’re hot, your heart pumps blood closer to the skin to help you cool down. This is why your "normal" rate in July might be 10 beats higher than it is in January. Even your posture changes things. There is a specific condition called POTS (Postural Orthostatic Tachycardia Syndrome) where a person’s heart rate skyrockets just by standing up. For most people, a slight rise when standing is expected, but if it jumps by 30 bpm or more, your body is struggling to manage gravity.
The Sleep Factor
While you sleep, your heart rate should dip. This is called "nocturnal dipping," and it's vital for your heart to recover. If your normal pulse rate stays high while you're dreaming, it could be a sign of sleep apnea or chronic overtraining. Dr. Eric Topol, a renowned cardiologist and digital health expert, has often pointed out that wearable tech is actually changing how we see these trends. We used to get a pulse reading once a year at the doctor. Now, we have thousands of data points showing how our hearts react to a bad night’s sleep or a glass of wine.
Alcohol is a silent heart rate killer. Even one drink can keep your resting heart rate elevated for hours after the buzz wears off. Your heart is working overtime to process the toxins, and your nervous system is stuck in a "fight or flight" sympathetic state instead of the "rest and digest" parasympathetic state.
Age, Gender, and the Biological Curve
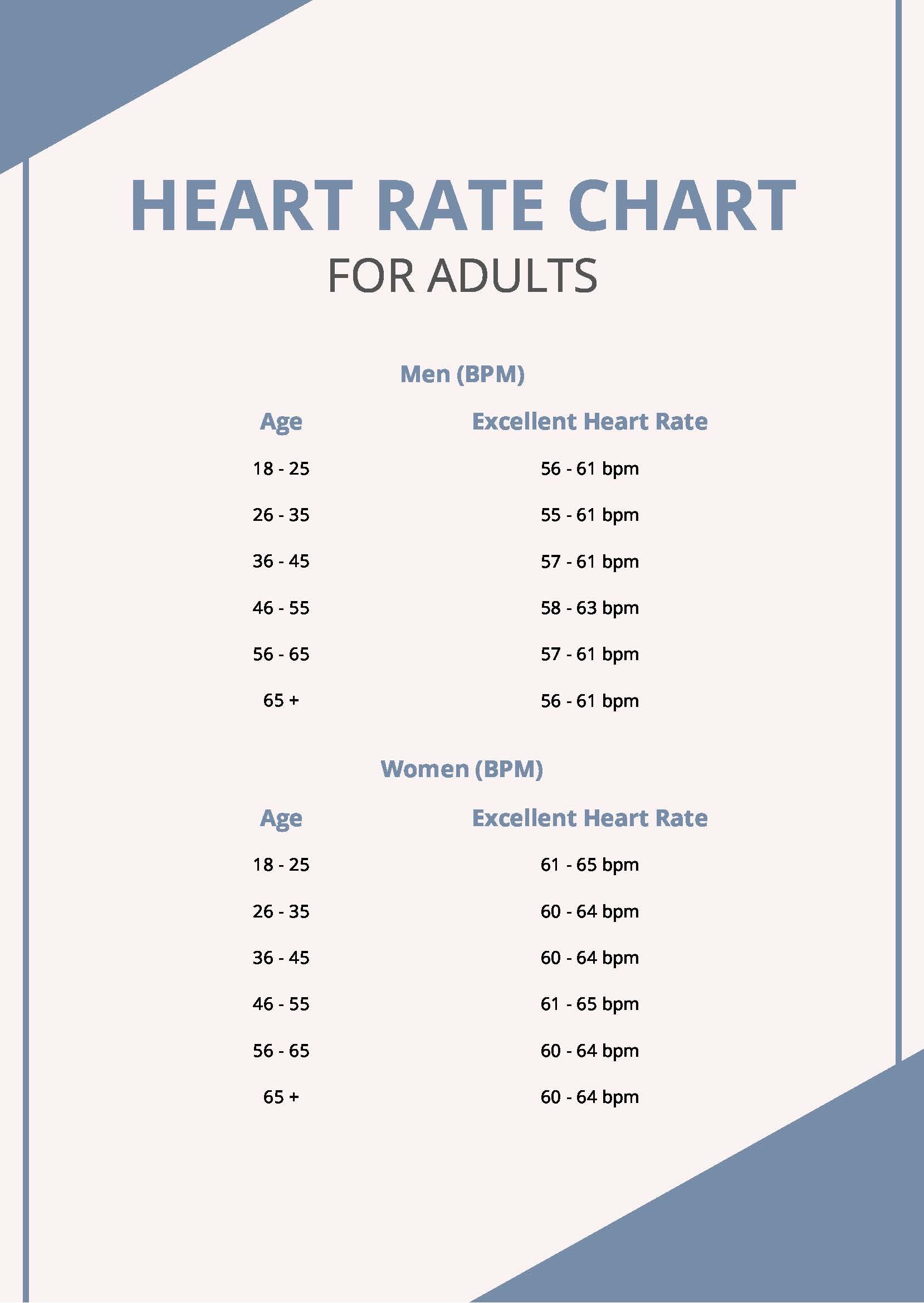
Women generally have higher resting heart rates than men. This isn't a sign of poor fitness; it's mostly due to smaller heart size. A smaller heart has to beat more frequently to move the same amount of blood.
Age is the other big variable. You’ve probably heard of the "220 minus your age" formula for calculating your maximum heart rate. It’s a bit of a blunt instrument, honestly. It was never intended to be a hard rule, yet it’s programmed into every treadmill at the gym. As you get older, your heart's maximum capacity naturally declines, but your resting normal pulse rate doesn't necessarily have to climb. In fact, many seniors who stay active maintain resting pulses in the 60s, which is a fantastic indicator of longevity.
When Should You Actually Be Worried?
I’m not a doctor, but cardiologists generally look for patterns rather than single data points. One high reading doesn't mean much. However, there are two terms you should know: Tachycardia and Bradycardia.
📖 Related: Healthy Fizzy Drinks: Why Most Of What You're Buying Is Kind Of A Lie
Tachycardia is when your resting heart rate is consistently over 100 bpm. This can be caused by anything from anemia to thyroid issues. If your heart is racing while you're just sitting there, it’s a signal that something is taxing your system.
Bradycardia is the opposite—under 60 bpm. As we discussed, this is great if you’re a runner. But if you aren't an athlete and your pulse is 45 bpm, and you feel dizzy, tired, or faint? That’s a problem. It means your brain isn't getting enough oxygen.
Then there’s the "skipped beat." Most people feel a palpitation at some point—that weird thud or flip-flop in the chest. Usually, it's a PVC (Premature Ventricular Contraction). They are almost always harmless, triggered by caffeine, stress, or lack of magnesium. But if they happen constantly, it’s worth getting an EKG just to rule out an underlying arrhythmia like Atrial Fibrillation (Afib).
The Influence of Modern Anxiety
We live in a state of "micro-stress." Every notification on your phone is a tiny hit of adrenaline. Over time, this constant stimulation can shift your baseline normal pulse rate higher. We are essentially training our hearts to stay on high alert.
Breathwork isn't just "woo-woo" wellness talk; it’s a mechanical override for your heart. When you exhale longer than you inhale, you stimulate the vagus nerve. This sends a chemical signal (acetylcholine) to your heart to slow down. You can literally drop your pulse by 10 beats in two minutes just by changing how you breathe.
What to Look for in Your Data
If you wear a smartwatch, don't obsess over the minute-by-minute changes. Look at the Weekly Average Resting Heart Rate. This is the most "honest" number.
- A sudden trend upward: You might be getting sick. Often, your resting heart rate will spike 24-48 hours before you even feel a scratchy throat. It's your immune system revving up the engine.
- A trend downward: Your fitness is likely improving, or you're finally getting enough recovery.
- High variability: This is actually a good thing. Heart Rate Variability (HRV) is the measure of the time difference between beats. You want a high HRV. A "perfect" metronome heart is actually a sign of extreme stress. You want a heart that can adapt and change its rhythm instantly.
Actionable Steps to Optimize Your Pulse
Forget just hitting a "normal" number. Aim for an optimal one.
First, get a baseline. Measure your pulse manually first thing in the morning before you get out of bed. Put two fingers on your wrist (the radial artery) and count for 60 seconds. Don't do the "count for 15 and multiply by 4" trick—it's less accurate for catching subtle irregularities.
Hydrate like it's your job. Blood is about 90% water. When you're dehydrated, your blood gets thicker (more viscous), and your heart has to pump harder to move that sludge through your veins. Drinking a glass of water can sometimes drop a high resting pulse almost immediately.
Magnesium and potassium are the electrolytes that run your heart's electrical system. Most modern diets are chronically low in magnesium. If you’re prone to palpitations or a slightly "bouncy" pulse, check your mineral intake. Spinach, almonds, and avocados are your heart's best friends here.
Move, but don't just do "cardio." Zone 2 training—which is exercise where you can still hold a conversation—is the sweet spot for strengthening the heart muscle without overtaxing the nervous system. It builds the size of the left ventricle, allowing it to pump more blood per beat.
Check your medications. Everything from decongestants to asthma inhalers and ADHD meds can send your normal pulse rate into the triple digits. If you started a new med and your heart is suddenly hammering, that’s a conversation for your doctor.
💡 You might also like: Exactly How Much is 20 Grams of Sugar? A Reality Check for Your Pantry
Finally, stop checking it every five minutes. Health anxiety is a real thing. If you stare at your heart rate monitor all day, the anxiety of seeing a high number will cause a high number. It's a feedback loop that serves no one. Put the watch on "theatre mode" for a day and just live. Your heart knows what to do.
Next Steps for Your Health
- Conduct a Morning Baseline Test: For the next three days, measure your pulse manually for 60 seconds before leaving bed. Average these three numbers to find your true resting heart rate.
- The Hydration Experiment: If you notice your pulse is above 80 bpm while resting, drink 16 ounces of water and re-test in 30 minutes to see if dehydration was the culprit.
- Audit Your Stimulants: Track your caffeine and nicotine intake for 48 hours and note any correlation with "racing heart" sensations or palpitations.
- Consult a Professional: Schedule an appointment if your resting heart rate is consistently above 100 bpm or below 50 bpm (without athletic training), or if you experience shortness of breath and chest pain regardless of the number.