You’re sitting on the couch, maybe scrolling through your phone, when you suddenly feel it. A little thump in your chest. Or maybe you’re checking your Apple Watch and notice the number is higher than it was yesterday. You start wondering about what should be the normal pulse rate and if yours is actually okay. Most people think there is one "perfect" number.
There isn't.
Your heart isn't a metronome. It’s a living, breathing pump that reacts to everything from that third cup of coffee to the stressful email your boss just sent. Honestly, the range for a "normal" heart rate is much wider than most of the posters in your doctor’s waiting room suggest. While the standard medical textbook answer is 60 to 100 beats per minute (bpm), that’s just the baseline. A lot of nuance lives in the gaps between those numbers.
The 60 to 100 Myth and the Reality of Your Resting Heart Rate
For decades, the American Heart Association (AHA) has hammered home the 60–100 bpm range for adults. It's a safe bet. If you're in that window, you're usually fine. But here’s the kicker: many researchers now believe that the upper end of that range—specifically consistently sitting between 80 and 100 bpm—might actually be a subtle warning sign.
A massive study published in the journal Heart tracked middle-aged men for two decades and found that those with a resting heart rate at the higher end of the "normal" spectrum had a higher risk of cardiovascular issues compared to those in the 50s or 60s. It makes sense, right? If your heart has to beat 100 times every single minute just to keep you alive while you're watching TV, it’s working harder than a heart that only needs to beat 60 times.
But then you have the athletes.
If you’re a long-distance runner or a cyclist, your resting pulse might dip into the 40s or 50s. This is called sinus bradycardia. In a fit person, it's not a bug; it's a feature. Their heart muscle is so efficient and strong that it pumps a larger volume of blood with every single squeeze. They don't need the extra beats.
What changes the rhythm?
It’s not just about fitness.
Age is a huge factor. Newborns have hearts that race at 70 to 190 bpm because their bodies are growing at an astronomical rate. As we get older, that pace slows down. By the time you’re a teenager, you’re basically at the adult range. Then there's the "caffeine effect." If you've ever had an espresso on an empty stomach and felt your chest fluttering, you know exactly how chemical stimulants mess with your electrical system. Stress, dehydration, and even the temperature of the room can shift your pulse by 10 or 15 beats in a matter of minutes.
How to Actually Measure Your Pulse Without Overthinking It
Most people check their pulse when they’re already anxious. That’s the worst time to do it. If you’re worried about your heart, your brain releases adrenaline, which... you guessed it... makes your heart beat faster.
To get a real reading of what should be the normal pulse rate for your specific body, you need to be boring. Sit down. Don’t talk. Don't look at social media. Just sit for five minutes.
- Find your radial artery on the thumb side of your wrist.
- Use your index and middle fingers, not your thumb (your thumb has its own pulse, which gets confusing).
- Count the beats for 30 seconds and double it.
- Or count for 60 seconds if you want to be super precise.
If you’re using a wearable like a Fitbit or a Garmin, take the "resting heart rate" data with a grain of salt. These devices are great at tracking trends over months, but they can be notoriously finicky if the strap is loose or if you’re moving your arm. Use them as a compass, not a GPS.
💡 You might also like: Fear of Letting People Down: Why We’re All So Exhausted and How to Actually Stop
When the Numbers Get Weird: Tachycardia and Bradycardia
Sometimes the pulse goes off the rails.
Tachycardia is the medical term for a heart rate over 100 bpm at rest. Sometimes it’s just because you’re dehydrated or have a fever. When you’re sick, your heart beats faster to move immune cells around and manage your elevated body temp. But if your heart is racing for no reason while you’re just chilling on the sofa, that’s something a doctor needs to look at. It could be an overactive thyroid or an electrical "short circuit" in the heart like SVT (Supraventricular Tachycardia).
On the flip side, bradycardia is when the rate is below 60. As we talked about, it’s fine for athletes. But if you’re 75 years old, not a marathoner, and your pulse is 45, you’re probably going to feel dizzy or tired. Your brain isn't getting enough oxygenated blood.
The Anxiety Loop
We have to talk about the "anxiety-pulse loop." This is huge.
Health anxiety can cause "white coat hypertension" or "white coat tachycardia." You walk into the doctor's office, you see the blood pressure cuff, and your heart starts pounding. The nurse records a pulse of 110. Now you’re worried because 110 is "high." That worry keeps the pulse high for the rest of the day. It’s a vicious cycle. Honestly, sometimes the best thing you can do for your heart rate is to stop checking it for a week and see if your symptoms (like lightheadedness or palpitations) actually persist when you aren't staring at the numbers.
Beyond the Beats: Heart Rate Variability (HRV)
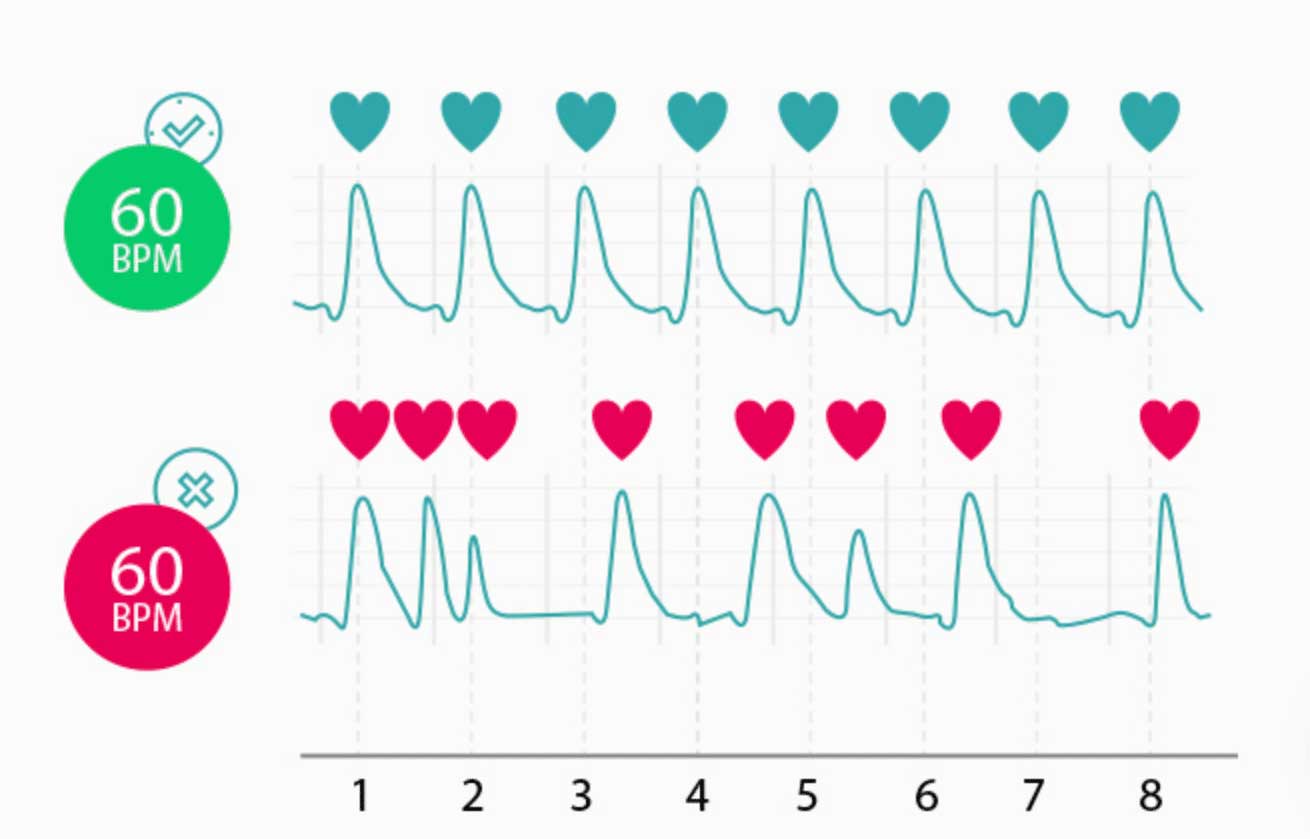
If you want to go deeper than just the pulse rate, look at HRV.
This is the newest darling of the health tech world. HRV isn't about how many times your heart beats per minute; it’s about the variation in time between each beat. Surprisingly, you want a "messy" heart. You want the intervals between beats to vary slightly. A high HRV means your nervous system is flexible and can switch between "fight or flight" and "rest and digest" easily. If your heart is beating like a perfect, rigid clock (low HRV), it often means you’re overstressed or overtrained.
Practical Steps for a Healthier Pulse
So, you want to improve your numbers? You can't just wish your pulse lower. It takes a bit of work, but it’s mostly lifestyle maintenance.
💡 You might also like: Lower Abdominal Pain ICD 10 Code: What Your Doctor Is Actually Looking For
First, focus on cardiovascular "base training." You don't need to sprint. Long, slow walks or easy bike rides—where you can still hold a conversation—strengthen the heart muscle over time. This is the most effective way to lower your resting heart rate naturally.
Second, watch the "hidden" stimulants. It’s not just coffee. Some over-the-counter cold medicines and even certain herbal supplements can kick your heart into overdrive.
Third, hydration is king. When you’re dehydrated, your total blood volume drops. To make up for the lack of fluid, your heart has to beat faster to maintain blood pressure. Drink a glass of water, wait twenty minutes, and check your pulse again. You might be surprised.
When to See a Doctor
Don't ignore the "tags" that come with a fast or slow pulse. If your pulse is outside the 60-100 range AND you feel:
- Chest pain (even "minor" pressure)
- Shortness of breath while doing nothing
- Fainting spells or near-fainting
- A "flopping" sensation in your chest that won't stop
Go get an EKG. It’s a simple, non-invasive test that shows the electrical map of your heart. It can rule out things like Atrial Fibrillation (Afib), which is a common rhythm issue where the top chambers of the heart quiver instead of pumping correctly.
Summary of Actionable Insights
To keep your pulse in a healthy zone, start by tracking your resting rate immediately upon waking up, before you even get out of bed. This is your "true" baseline. If you notice a steady creep upward over several weeks, check your stress levels and sleep quality first.
Prioritize magnesium-rich foods like spinach and almonds, which support electrical signaling in the heart, and aim for at least 150 minutes of moderate activity per week. Most importantly, stop comparing your pulse to your friend’s or a celebrity’s. Your "normal" is a moving target influenced by your genetics and your daily habits. Keep an eye on the trends rather than the individual blips, and always trust your physical symptoms over a flickering number on a digital screen.