Your heart is basically a muscle that never gets a day off. It beats about 100,000 times a day, every single day, until it doesn't. But honestly, most of us only ever think about it when we’re sprinting for a bus or looking at a weirdly high number on a Fitbit. You might see a "72" on your wrist and think you’re the picture of health, or see an "85" and start panicking that you’re about to have a medical emergency.
The truth is that a normal person heart rate is a moving target. It’s not a static number like your height or your social security number. It’s fluid. It reacts to the coffee you drank ten minutes ago, the fact that you’re slightly dehydrated, or that stressful email from your boss that’s currently sitting in your inbox.
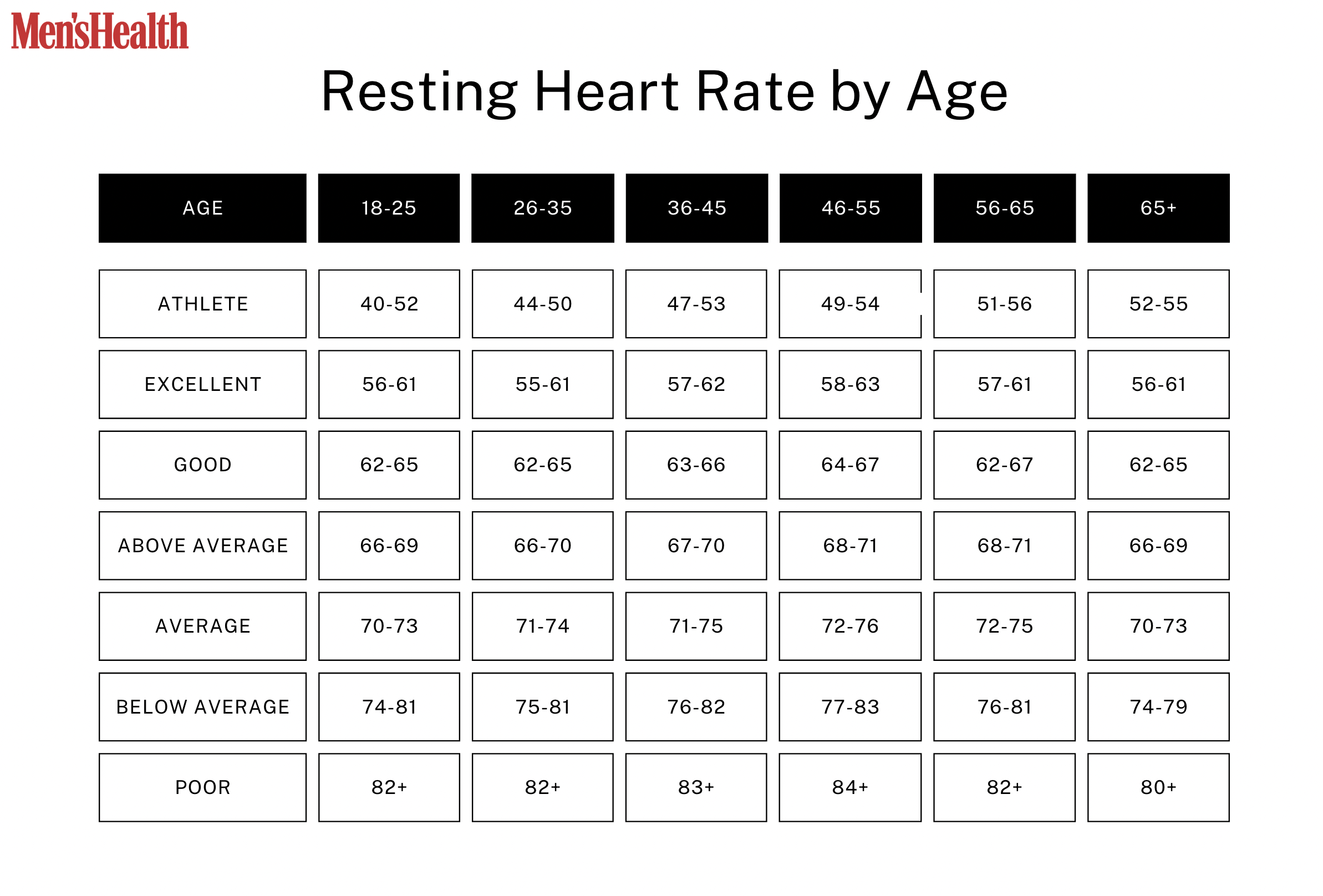
According to the American Heart Association (AHA), the standard "normal" range for an adult's resting heart rate is anywhere between 60 and 100 beats per minute (bpm). But let’s be real—if your heart is consistently hitting 98 while you're just sitting on the couch watching Netflix, most cardiologists are going to want to have a chat with you. There’s "normal" on paper, and then there’s "optimal."
The "Normal" Range vs. The "Healthy" Reality
If you ask a doctor what a normal person heart rate should look like, they’ll give you that 60-100 bpm window. It’s the gold standard. However, recent research published in The Lancet and various studies from the Harvard Medical School suggest that being at the higher end of that "normal" range might actually be a bit of a red flag.
Think about it this way.
If your heart has to beat 90 times every single minute just to keep you alive while you’re resting, it’s working significantly harder than a heart that only needs to beat 60 times. Over a decade, that’s millions of extra contractions. It’s wear and tear. Many experts now argue that a truly healthy resting heart rate for most non-athletes should probably sit between 50 and 70 bpm.
But don't freak out if you're an 80. Some people just have naturally smaller hearts or different autonomic nervous system wiring. If you’ve always been an 80, that might be your normal. The problem usually arises when your "normal" starts creeping up over time without a clear reason.
👉 See also: Nuts Are Keto Friendly (Usually), But These 3 Mistakes Will Kick You Out Of Ketosis
Why athletes have "weird" numbers
You’ve probably heard stories about elite marathon runners like Eliud Kipchoge or Tour de France cyclists having resting heart rates in the 30s. To a normal person, that sounds like a literal coma. But for an athlete, it’s just efficiency. Their heart muscle is so thick and powerful that it pumps a massive volume of blood with a single squeeze. They don't need to beat often because each beat is high-quality.
For the rest of us? If your heart rate drops to 38 while you’re awake and you aren't training for an Ironman, you’d probably feel dizzy, tired, and generally like garbage. This is called bradycardia. It's only "good" if it's earned through cardiovascular conditioning.
What Actually Changes Your Pulse?
Everything. Literally everything.
Temperature is a big one. If it’s a sweltering July afternoon, your body has to work harder to radiate heat away from your skin. Your heart rate will climb. Same goes for emotions. Anxiety isn't just "in your head"—it’s a physiological cascade. Your adrenal glands dump cortisol and adrenaline into your system, telling your heart to prep for a fight, even if you’re just worried about a dental appointment.
Then there’s the stuff we put in our bodies.
- Caffeine: A classic. It blocks adenosine receptors, which usually help you relax, leading to a spiked pulse.
- Nicotine: A potent stimulant that narrows blood vessels and forces the heart to pump faster against more resistance.
- Alcohol: This is a tricky one. While a glass of wine might make you feel relaxed, alcohol is actually a cardiac irritant. Many people experience "holiday heart syndrome" where their heart rate jumps or becomes irregular after a night of drinking.
- Dehydration: When you’re low on fluids, your blood volume actually drops. To keep your blood pressure stable, your heart has to beat faster to move what little fluid is left.
Medications also play a massive role. Beta-blockers, often prescribed for high blood pressure, are designed specifically to slow the heart down. On the flip side, some asthma inhalers or OTC cold medicines containing pseudoephedrine can make your chest feel like a drum kit.
✨ Don't miss: That Time a Doctor With Measles Treating Kids Sparked a Massive Health Crisis
How to Actually Measure Your Normal Person Heart Rate
Most people check their heart rate wrong. They check it after walking up the stairs, or right after a meal, or while they're annoyed. To get a true reading of your normal person heart rate, you need to find your "basal" rate.
The best time to do this is the very second you wake up. Before you get out of bed. Before you check your phone and see a stressful news headline. Before that first hit of caffeine.
- Find your pulse on your wrist (radial) or neck (carotid).
- Use your index and middle fingers—never your thumb, because your thumb has its own pulse that will confuse you.
- Count the beats for a full 60 seconds. Sure, you can do 15 seconds and multiply by four, but a full minute is way more accurate for catching slight irregularities.
If you’re using a wearable like an Apple Watch or a Garmin, don't just look at the "Current HR" screen. Look at the "Resting Heart Rate" trend over a week. Wearables use algorithms to filter out the noise of your daily movement, providing a much clearer picture of what your heart is doing when you aren't looking.
When Should You Actually Be Worried?
Medical anxiety is real, and the "worried well" population is growing thanks to all the data we have on our wrists. But there are specific times when a normal person heart rate becomes a medical issue.
Tachycardia is the medical term for a resting heart rate over 100 bpm. If you’re just sitting there and your heart is racing like you’re on a treadmill, that’s a problem. It could be anemia, it could be a thyroid issue (hyperthyroidism is a huge culprit for high HR), or it could be an arrhythmia like SVT (Supraventricular Tachycardia).
The "danger zone" isn't just about the number, though. It's about the symptoms.
🔗 Read more: Dr. Sharon Vila Wright: What You Should Know About the Houston OB-GYN
If you have a high or low heart rate plus chest pain, shortness of breath, or fainting spells (syncope), that is a non-negotiable trip to the doctor. A pulse of 110 while you’re nervous for a speech is one thing. A pulse of 110 while you’re lying in a dark room feeling like you can't catch your breath is another entirely.
The Myth of the "Fat Burning Zone"
Since we’re talking about heart rates, we have to mention the gym. You’ve seen those colorful charts on the elliptical machines. They tell you that if you stay in a lower heart rate zone, you’ll burn more fat.
It’s kinda true, but also mostly a misunderstanding.
Yes, at lower intensities, your body uses a higher percentage of fat for fuel. But at higher intensities, you burn way more total calories. If you’re trying to improve your heart health, don't get too bogged down in the "fat-burning" zone. Focus on your recovery heart rate—how fast your heart returns to normal after you stop moving. That is a much better indicator of your actual cardiovascular age than your resting pulse alone.
Improving Your Numbers Without Medication
If you’ve realized your resting heart rate is a bit higher than you’d like, you aren't stuck with it. The heart is a muscle. You can train it.
Consistent aerobic exercise is the most obvious path. You don't need to run marathons. Even a brisk 30-minute walk five days a week can lower your resting heart rate by several beats over a few months. It makes the heart more efficient.
Sleep is the "hidden" factor. Sleep deprivation puts your body in a state of chronic stress, which keeps your sympathetic nervous system (fight or flight) in the driver's seat. Better sleep equals a lower resting pulse. Period.
Lastly, check your magnesium levels. Magnesium is crucial for the electrical signaling in your heart. Many people are subclinically deficient, and simply getting enough of it (through spinach, almonds, or supplements) can sometimes "quiet" a jumpy heart.
Actionable Steps for Heart Health
- Audit your data: Instead of checking your pulse daily, look at your weekly average. Ignore the outliers caused by a bad night's sleep or a heavy workout.
- The "Morning Minute": For the next three days, take your manual pulse the moment you wake up. Average those three numbers to find your true baseline.
- Check your meds: Read the labels on any stimulants or decongestants you take regularly. They might be artificially inflating your numbers.
- Hydrate aggressively: Try drinking an extra liter of water tomorrow and see if your resting heart rate drops by 3-5 bpm. You'd be surprised how often "high heart rate" is just "thirst."
- Talk to a pro: If your resting heart rate is consistently over 100 or under 50 (and you aren't an athlete), book an appointment for an EKG just to get a baseline of your heart's electrical rhythm.