You’ve felt it. That lingering tickle in your throat that turns into a dry, hacking cough. You aren't "bedridden" sick, so you keep going to work, keep hitting the gym, and keep grabbing coffee with friends. Most people call it a "tough cold." Doctors call it mycoplasma pneumoniae, or more colloquially, walking pneumonia. It’s a bit of a medical trickster because it doesn't follow the rules of a standard bacterial infection.
The name alone sounds like something out of a sci-fi novel. Honestly, Mycoplasma is one of the weirdest organisms in the microscopic world. It lacks a cell wall. That sounds like a boring biology fact, but it’s actually a huge deal for your recovery. Most common antibiotics, like penicillin or amoxicillin, work by attacking the cell walls of bacteria. Since Mycoplasma pneumoniae doesn't have one, those "standard" prescriptions are basically useless against it. You could swallow amoxicillin like candy and the bacteria wouldn't even flinch.
What is Mycoplasma Pneumoniae anyway?
It’s small. Really small. In fact, Mycoplasma pneumoniae is one of the smallest free-living organisms discovered to date. Because it's so tiny and lacks a rigid structure, it can wedge itself into places other bacteria can't. It hitches a ride on respiratory droplets. You breathe in a few microscopic particles from someone's sneeze, and suddenly, these little hitchhikers are attaching themselves to the lining of your airways.
They don't just sit there. They actually damage the cilia—those tiny hair-like structures in your lungs that sweep out mucus and debris. When the cilia stop working, the mucus builds up. You start coughing. And coughing. And then you cough some more. This isn't the "productive" cough you get with a chest cold where things are moving; it’s often a dry, persistent rattle that keeps you up at 3:00 AM wondering if you’re ever going to breathe normally again.
🔗 Read more: The Ulas Family: Why Some Humans Still Walk on All Fours
Historically, we see these spikes every few years. The CDC noted a significant uptick in cases throughout 2024 and into 2025, particularly among children. For a long time, we thought of walking pneumonia as a "school-age" disease or something that only happened in military barracks. We were wrong. While it's common in kids aged 5 to 17, it’s making a massive comeback in toddlers and older adults, often appearing in clusters within households or offices.
The "Walking" Part is a Trap
The term "walking pneumonia" is actually a bit dangerous. It implies it’s "pneumonia-lite."
Because you can still walk around, you don't rest. You keep pushing. This often leads to the infection dragging on for three, four, or even six weeks. It's an "atypical" pneumonia. While "typical" pneumonia (caused by things like Streptococcus pneumoniae) usually hits you like a freight train with high fevers and extreme exhaustion, Mycoplasma is a slow burn.
You might have a low-grade fever of 100.2°F. You might just feel "off." Then the sore throat starts. Then the headache. By the time the cough becomes the primary symptom, the bacteria have already set up shop.
Identifying the Signs You Actually Have It
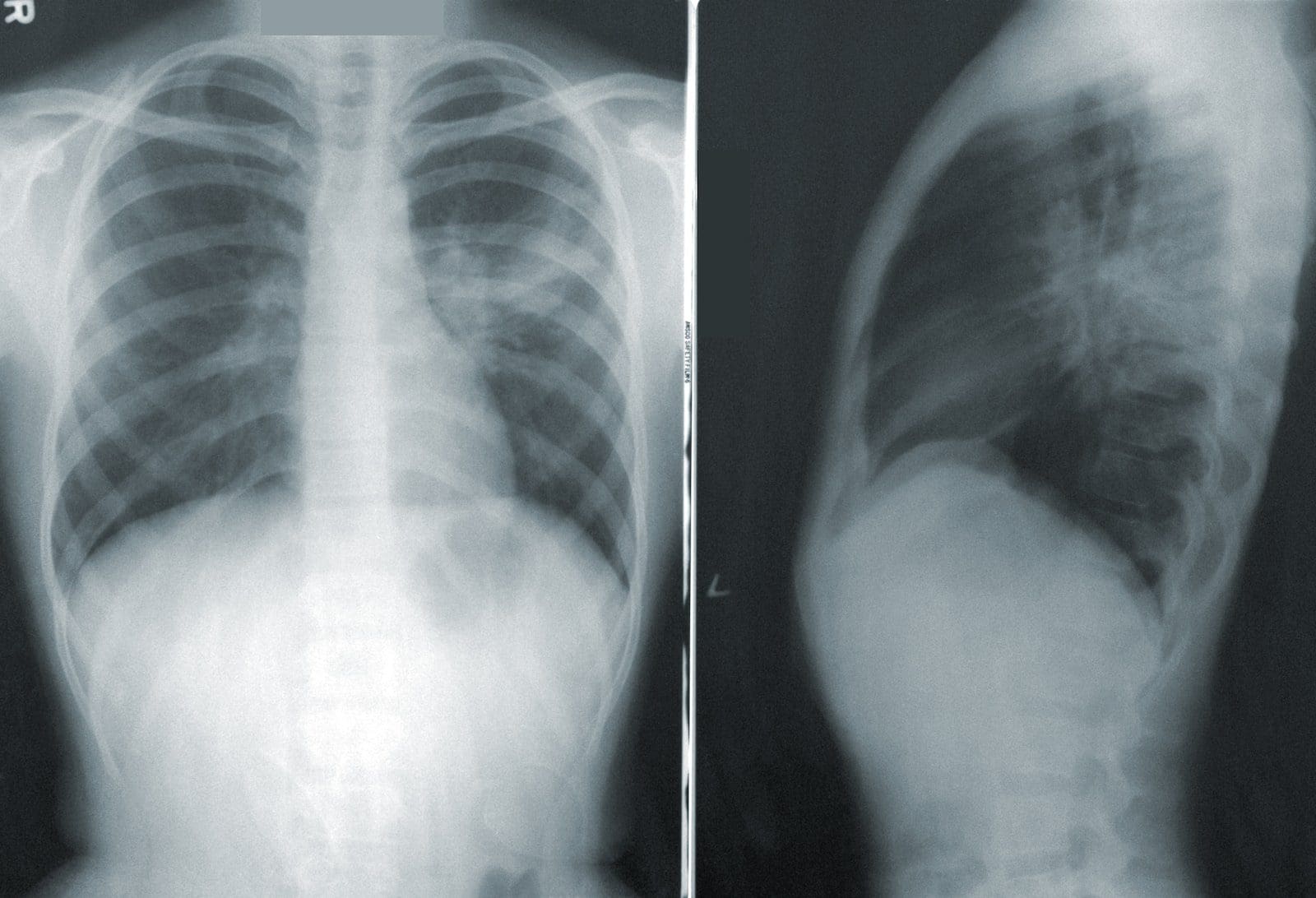
How do you know it's not just a flu or the latest COVID-19 variant? It’s tough. Diagnosis often requires a specific PCR test or a blood test to check for antibodies (IgM and IgG). Most doctors will listen to your lungs with a stethoscope. Interestingly, sometimes the "crackling" sounds of pneumonia are audible even if you feel relatively okay. Other times, the lungs sound totally clear, but a chest X-ray shows "patchy infiltrates"—white cloudy areas that indicate infection.
- The Dry Hack: It rarely starts with phlegm. It’s a tickle that won't go away.
- Chest Soreness: Not from the infection itself, but from the sheer physical labor of coughing for ten days straight.
- Ear Infections: Surprisingly, Mycoplasma can cause bullous myringitis—painful blisters on the eardrum. If your chest hurts and your ears ache, that’s a red flag.
- Skin Rashes: In rare cases, especially in younger patients, it can trigger a rash called Erythema Multiforme.
If you’ve had a "cold" for more than ten days and it’s getting worse instead of better, you aren't dealing with a standard rhinovirus. Viruses usually peak around day five. Mycoplasma pneumoniae is just getting started at day five.
Why Your Usual Meds Aren't Working
Let’s talk about the antibiotic problem again. If you go to an urgent care and they give you a "Z-Pak" (Azithromycin), they are targeting the right thing. Macrolides like Azithromycin or Clarithromycin are the go-to treatments because they inhibit protein synthesis inside the bacteria rather than attacking the non-existent cell wall.
However, there is a growing concern about antibiotic resistance. In parts of Asia, resistance to macrolides in Mycoplasma cases has been reported as high as 80% or 90% in some studies. In the U.S., it's lower, but it’s rising. If Azithromycin fails, doctors might move to Doxycycline (a tetracycline) or Levofloxacin (a fluoroquinolone).
✨ Don't miss: Finding a Medical Power of Attorney Form Free: What Most People Get Wrong About Making Their Own
But here’s the kicker: Doxycycline can stain the teeth of very young children if used repeatedly, and fluoroquinolones have their own set of heavy side effects. It’s a balancing act. This is why doctors don't just hand out these meds for every sniffle. They want to be sure it’s bacterial.
The Timeline: What to Expect
Recovery isn't a straight line. It’s more of a jagged path.
Week 1: The incubation period is long—sometimes up to three weeks after exposure. You might feel a scratchy throat and a general sense of fatigue. You assume it’s stress.
Week 2: The cough arrives. It’s annoying. You’re taking over-the-counter suppressants, but they aren't doing much. This is usually when the low-grade fever kicks in. You’re still "walking," but you’re tired.
Week 3: This is the "make or break" week. If your immune system is winning, the cough starts to subside. If the bacteria are winning, you might start feeling short of breath. This is when most people finally cave and go to the doctor.
Week 4 and Beyond: Even with the right antibiotics, the "post-infectious" cough can linger. Your airways are sensitive. A gust of cold air or a bit of dust can trigger a coughing fit that lasts five minutes. This isn't because you’re still "infected," but because your lungs are healing from the microscopic carnage.
💡 You might also like: How Do You Get Rid Of Puffy Eyes Fast? What Actually Works When You Wake Up Swollen
Beyond the Lungs: Rare Complications
It’s rare, but Mycoplasma pneumoniae can go systemic. It has been linked to neurological issues like encephalitis (brain swelling) or Guillain-Barré syndrome. Some people develop joint pain or even heart palpitations (pericarditis).
This is why we shouldn't dismiss walking pneumonia as a joke. While most people recover perfectly fine with some rest and maybe a round of Doxycycline, for the immunocompromised or those with underlying asthma, it can trigger severe respiratory distress. If you have asthma, Mycoplasma is like pouring gasoline on a fire. It triggers inflammation that can lead to a massive flare-up or even a secondary bacterial infection like Staph or Strep.
Practical Steps for Recovery and Prevention
Since there is no vaccine for mycoplasma pneumoniae, you have to rely on old-school hygiene and smart recovery.
- Stop "Walking": If you are diagnosed, actually lie down. Your body needs ATP (energy) to fight the infection. If you're using that energy to run errands, you're extending your illness by weeks.
- Hydration is Literal Medicine: Thicker mucus is harder to cough up. Water thins it out. Skip the soda; stick to water or broth.
- Humidifiers are Your Best Friend: Dry air irritates the already damaged cilia in your lungs. A cool-mist humidifier can take the edge off the nighttime coughing fits.
- Check Your Contacts: Because the incubation period is so long, you likely caught it from someone 2-3 weeks ago. Likewise, you’ve probably been shedding the bacteria for a while. Tell your close contacts to watch for a lingering cough.
- Probiotics: If you’re put on Doxycycline or Azithromycin, your gut microbiome is going to take a hit. Eat fermented foods or take a high-quality probiotic to avoid the "second wave" of stomach issues.
The reality of walking pneumonia is that it's a test of patience. It’s a slow-moving, stubborn infection that preys on our tendency to "power through." Honestly, the best thing you can do is listen to that nagging cough earlier rather than later. If you've been hacking for a week and you're feeling more tired than usual, stop guessing. Get a proper test.
Don't wait until you're struggling to catch your breath to take it seriously. Early intervention with the right kind of antibiotic—the kind that doesn't care about cell walls—can turn a month-long ordeal into a one-week recovery. Take the rest. Drink the water. Let your lungs heal.