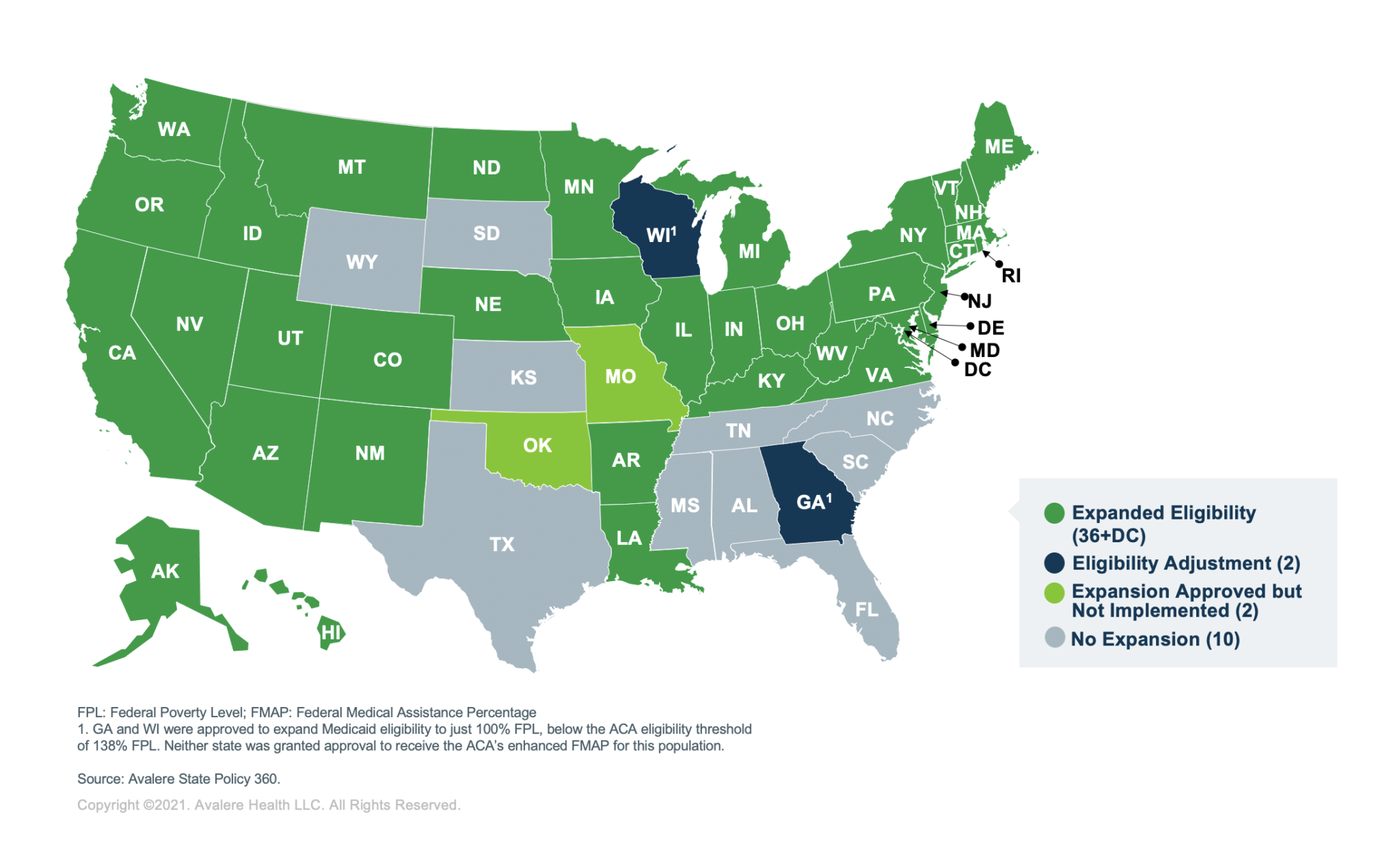
The map showing which states have expanded Medicaid looks a lot different than it did a decade ago. It’s messy. If you've spent any time looking at a Medicaid expansion states map lately, you’ve probably noticed the country is basically split into two worlds. On one side, you have the 41 states (counting DC) that said yes to the federal money. On the other, ten states—mostly in the South—are still holding out.
But here’s the thing: it isn’t just a "yes" or "no" game anymore.
Since the 2012 Supreme Court ruling made this whole thing optional, states have been getting creative. Or difficult. Depending on who you ask. We’re in 2026 now, and the landscape has shifted again thanks to new federal laws like H.R. 1, which some call the "Big Beautiful Bill." It added work requirements into the mix for the first time on a national level. Honestly, if you think you know who’s "in" and who’s "out," you might be looking at an outdated map.
The Current Medicaid Expansion States Map: Who Is Actually In?
As of early 2026, 40 states and the District of Columbia have fully adopted the expansion. North Carolina was one of the last big dominoes to fall back in late 2023. Since then, the momentum has slowed down, but the stakes have gone up.
If you live in an expansion state, the rules are generally simple: if your income is below 138% of the Federal Poverty Level (FPL), you qualify. For a single person in 2025, that was about $21,597. But "qualified" doesn't mean "free and clear" like it used to.
💡 You might also like: What Pictures of Bee Sting Actually Tell You About Your Reaction
The New "Work" Reality
The federal government recently threw a wrench into the works. Starting in late 2026, many expansion states will start enforcing work requirements for adults. This was a massive part of the H.R. 1 legislation. If you’re between 19 and 55, you’ll likely need to prove you’re working, in school, or volunteering for at least 80 hours a month.
States like Arkansas and New Hampshire tried this years ago and it was a bit of a disaster—thousands of people lost coverage just because they couldn’t figure out the reporting website. Now, it's becoming the law of the land for almost everyone.
The Ten States Still Holding Out
The "Non-Expansion" list is shrinking, but the remaining holdouts are dug in deep. These states haven't adopted the 138% FPL threshold:
- Alabama
- Florida
- Georgia (the weird exception)
- Kansas
- Mississippi
- South Carolina
- Tennessee
- Texas
- Wisconsin (another weird exception)
- Wyoming
Texas and Florida are the big ones. Combined, they account for over 60% of the people stuck in the "coverage gap." That gap is a weird, frustrating place to be. You make too much for traditional Medicaid (which usually only covers parents or people with disabilities), but you make too little to get subsidies for a private plan on the Marketplace.
Why Georgia and Wisconsin Are "Different"
You’ll often see Georgia and Wisconsin colored differently on a Medicaid expansion states map.
Georgia has a program called "Pathways to Coverage." It’s a partial expansion. They cover people up to 100% of the poverty line, but only if they meet strict work requirements. The enrollment has been tiny—only about 11,000 people as of late last year, compared to the nearly half a million who would be covered under a full expansion.
Wisconsin is even stranger. They haven't "officially" expanded under the ACA rules, but they already cover everyone up to 100% of the FPL. Because they don't go up to 138%, they don't get the 90% federal "bonus" money. It's basically a political statement that costs the state millions of dollars every year.
The Ballot Box Battle
When legislatures say no, voters sometimes say yes. We saw this in South Dakota and Missouri. People literally bypassed their governors to get expansion into the state constitution.
But the "trigger law" trend is the new thing to watch. In 2025, South Dakota passed a measure that effectively says: "If the federal government ever drops their 90% funding share, we’re out." This will be on the November 2026 ballot. It's a safety valve for conservative states that are worried the federal government will eventually leave them holding the bill.
What Most People Get Wrong About the Map
One huge misconception is that expansion is "free" for the states. It’s not. While the feds pay 90%, the states have to find that last 10%. Some states, like North Carolina, use "provider taxes" on hospitals to cover their share.
However, the new H.R. 1 law put a moratorium on new provider taxes. This makes it way harder for the remaining 10 states to join the club. If a state like Mississippi wanted to expand today, they can’t just tax the hospitals to pay for it anymore. They have to find the money in their actual budget, which is a much tougher sell.
Another myth? That expansion kills the private insurance market. Actually, research from the Urban Institute shows that in expansion states, the uninsured rate halved. People are getting more preventive care, which generally keeps premiums from skyrocketing for everyone else because hospitals aren't eating as much "uncompensated care" cost.
Actionable Insights for 2026
If you are looking at the map because you need coverage, don't just give up if your state is "red" (non-expansion).
- Check the "Gap" anyway: Even in Texas or Alabama, you might qualify if you are pregnant, have a disability, or are a primary caretaker.
- The 100% FPL Trick: If you live in a non-expansion state and your income is above 100% of the poverty line, you can actually get very cheap (sometimes $0) private plans on Healthcare.gov. The "gap" only hurts you if you make less than that.
- Community Health Centers: If you're truly stuck in the gap, these centers use a sliding scale. They are the backbone of care in the South right now.
- Watch the 2026 Ballots: If you’re in Florida or Wyoming, there are active pushes to get expansion on your ballot. Your vote actually determines the map.
The map isn't static. It's a living document of political bickering and fiscal math. By the end of 2026, with the new work requirements kicking in and the South Dakota "trigger" vote, the colors on that map are probably going to shift again.
Stay informed on your local state's Department of Health and Human Services (DHHS) website. They are the only ones who can tell you exactly where you stand with the new 2026 reporting rules. Check your mail for "redetermination" packets; if you ignore them, you'll lose coverage even in a state that fully expanded.
The "Big Beautiful Bill" changes mean the 90/10 split is staying for now, but the hoops you have to jump through to keep that coverage are getting higher. Keep your paystubs and volunteer logs ready. The era of "simple" Medicaid expansion is officially over.