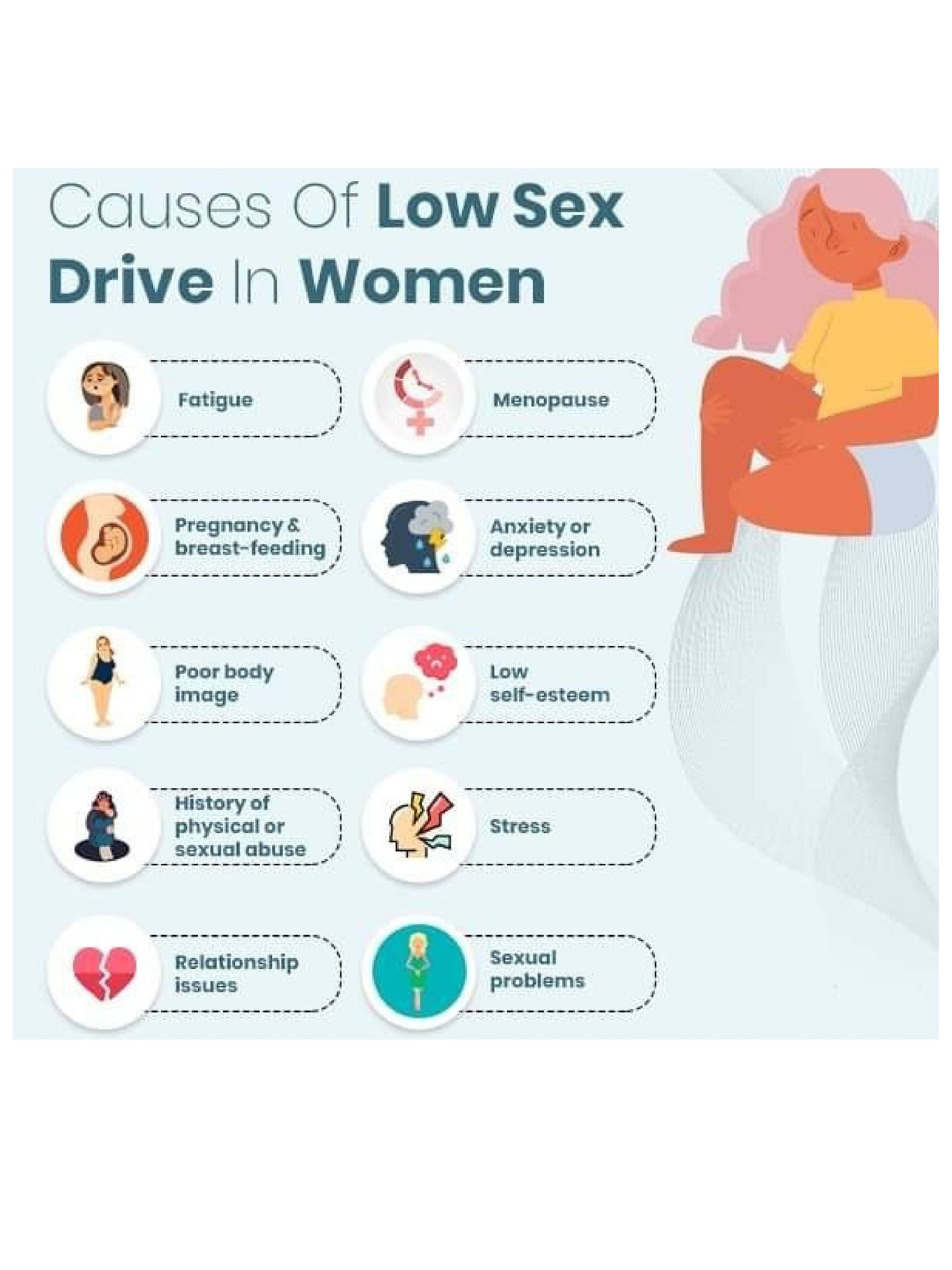
It starts with a subtle shift. Maybe you’re exhausted, or perhaps the thought of intimacy just feels like another chore on an endless to-do list, right next to meal prepping and answering emails. You aren't "broken." Honestly, it’s one of the most common things women bring up in doctors' offices, yet it remains shrouded in a weird kind of shame. We need to talk about low sex drive in women without the clinical coldness or the "just buy some lace lingerie" fluff.
Desire is messy. It’s a literal cocktail of neurochemistry, hormones, and whether or not your partner forgot to take out the trash for the third time this week.
The Biological Reality of the "Big Three"
Most people jump straight to hormones. While they aren't the whole story, they are a massive chunk of the "why."
Testosterone isn't just for the guys. Women produce it in the ovaries and adrenal glands, and it is the primary fuel for the "go" signal in your brain. When it dips—which it does naturally as we age or if you're on certain medications—the engine just won't turn over. Then there’s estrogen. This is the hormone that keeps things comfortable. When estrogen levels crater during menopause or postpartum, the physical act of sex can become genuinely painful due to vaginal atrophy. If it hurts, your brain is going to protect you by making you not want to do it. Simple survival.
Then we have prolactin. This is the "nursing hormone." If you’ve recently had a baby, your body is flooded with prolactin to support breastfeeding, which effectively puts your libido in a deep freeze. It’s nature’s way of saying, "Hey, we’re busy keeping this tiny human alive; we don't need another one yet."
Why Your Brain is the Biggest Mood Killer
Your brain is your largest sexual organ. Period.
✨ Don't miss: How to get over a sore throat fast: What actually works when your neck feels like glass
There is a concept in sex therapy called the Dual Control Model, pioneered by researchers like Dr. Emily Nagoski. Think of it as having an accelerator and a brake. Most of the time, when we talk about low sex drive in women, we focus on pushing the accelerator—trying to find "sparks." But usually, the problem is that the brakes are slammed to the floor. Stress is the biggest brake. When your cortisol is high because of work or family pressure, your nervous system is in "fight or flight" mode. You cannot be in "mate" mode and "survive" mode at the same time.
Mental health plays a huge role here too. Depression is a notorious libido killer, but the kicker is that the most common treatments—SSRIs like Prozac or Zoloft—often make the problem worse by numbing the very receptors needed for arousal. It’s a frustrating Catch-22 that millions of women navigate daily.
The Medication Minefield
Sometimes the thing trying to help you is the thing holding you back.
- Hormonal Birth Control: It’s ironic, isn't it? You take the pill to prevent pregnancy so you can have sex freely, but for many women, the pill shuts down the production of free testosterone, effectively killing the urge to have sex in the first place.
- Blood Pressure Meds: These can change how blood flows throughout the body, including to the pelvic region.
- Antihistamines: If they dry up your sinuses, they’re likely drying up everything else, too.
Relationship Friction and "Responsive Desire"
We have been sold a lie that desire should be "spontaneous"—that you should just be struck by a bolt of lightning while doing the dishes. For many women, desire is actually responsive. You might not feel "horny" out of the blue, but once things start moving, you're into it.
However, if there is simmering resentment in the relationship, the responsive desire never stands a chance. If you feel like your partner is just another person you have to take care of, the "switch" stays off. Research from the Journal of Sex Research consistently shows that egalitarian relationships—where the mental load is shared—report much higher levels of female sexual satisfaction and frequency.
🔗 Read more: How Much Should a 5 7 Man Weigh? The Honest Truth About BMI and Body Composition
Chronic Illness: The Invisible Barrier
We can't ignore the physical toll of chronic conditions. If you're dealing with Fibromyalgia, Endometriosis, or PCOS, your body is essentially in a state of constant inflammation or pain. Fatigue isn't just "being tired"; it's a deep, cellular exhaustion that makes the physical exertion of sex feel like running a marathon with a broken leg.
According to the Mayo Clinic, even conditions like diabetes can cause nerve damage that impacts sensation. When the physical reward for sex diminishes, the psychological drive follows suit. It’s a feedback loop that requires medical intervention, not just "trying harder."
Navigating the Fix: Real Steps Forward
The "fix" for low sex drive in women is rarely a single pill. It’s a multi-pronged approach that addresses the body, the mind, and the room.
1. Get a Full Blood Panel (The Right Way)
Don't just let a doctor tell you your labs are "normal." Ask for specifics. You want to see your Free Testosterone, SHBG (Sex Hormone Binding Globulin), and Thyroid (TSH, T3, and T4) levels. A "normal" range is huge; you want to know if you are at the bottom of that range. If your SHBG is high—common with birth control use—it’s soaking up all your testosterone like a sponge, leaving nothing for your libido.
2. Radical Stress Management
This isn't about a bubble bath. This is about completing the stress response cycle. If you've had a high-stress day, your body needs a physical signal that the "threat" is over. Exercise, a long hug, or even a good cry tells your nervous system it’s safe to move from "survival" back into "connection" mode.
💡 You might also like: How do you play with your boobs? A Guide to Self-Touch and Sensitivity
3. Address the "Brakes" First
Before you try aphrodisiacs or toys, look at what is actively stopping you.
- Is the room messy? Clean it.
- Is the door unlocked? Lock it.
- Are you worried about your body? Dim the lights.
Removing the distractions and inhibitors is often twice as effective as trying to add "stimulants."
4. Consult a Specialist in Female Sexual Medicine
Most GPs get very little training in female sexual dysfunction. Look for a provider certified by ISSWSH (International Society for the Study of Women’s Sexual Health). They understand the nuance of things like HSDD (Hypoactive Sexual Desire Disorder) and can discuss FDA-approved options like Addyi or Vyleesi, which work on brain chemistry, or localized estrogen creams for physical discomfort.
5. Shift the Definition of Intimacy
Sometimes the pressure to "go all the way" is the very thing that prevents anything from happening. Taking the goal of intercourse off the table—often called Sensate Focus exercises—can help rebuild the neural pathways for pleasure without the performance anxiety.
It is vital to remember that your sex drive will ebb and flow throughout your life. It is not a static number or a constant state of being. It’s a reflection of your overall health, your environment, and your relationship. If the "low" has become your "only," it is worth investigating, not because you owe sex to anyone, but because you deserve to feel vibrant and connected to your own body.
Next Steps for You:
- Track Your Cycle and Mood: Spend 30 days noting your energy, stress levels, and libido. Look for patterns—is it always low, or does it tank during your luteal phase?
- Audit Your Medications: List every supplement and prescription you take and bring it to a pharmacist or doctor specifically to ask about sexual side effects.
- The 10-Minute Talk: Sit down with your partner (outside of the bedroom) and identify three "brakes" that make you feel less interested in intimacy. Be honest, even if it feels awkward.