You probably know the drill at the doctor’s office. The cuff tightens, your arm pulses, and they shout out two numbers. 120 over 80. That’s the gold standard, right? Everyone obsesses over the top number—the systolic—because that’s the one linked to strokes and heart attacks. But then there’s that bottom number. The diastolic. When it starts dipping into the 50s or 40s, things get weird. You might feel fine. Or you might feel like you’re walking through a fog.
It’s called isolated diastolic hypotension.
Honestly, it’s a bit of a medical underdog. Doctors used to ignore it if the top number looked okay. But we’re finding out that low diastolic blood pressure causes aren’t just random glitches. They tell a story about how your heart is resting—or failing to rest. If that pressure is too low, your heart muscle might not be getting the oxygenated blood it needs during its "off" phase.
What’s actually happening when the bottom number drops?
Think of your heart like a pump. The systolic pressure is the force when the pump pushes blood out. The diastolic is the pressure in your arteries when the heart relaxes between beats. It’s the "refilling" phase. If that pressure is too low, the blood doesn't have enough "push" to get into the coronary arteries.
Your heart eats when it rests.
If the diastolic pressure is garbage, the heart starves a little. That’s why researchers like Dr. J. William McEvoy at Johns Hopkins have pointed out that extremely low diastolic levels can actually be a risk factor for heart damage, even if your systolic pressure is "perfect." It’s a delicate balance.
The big culprits: Why it happens
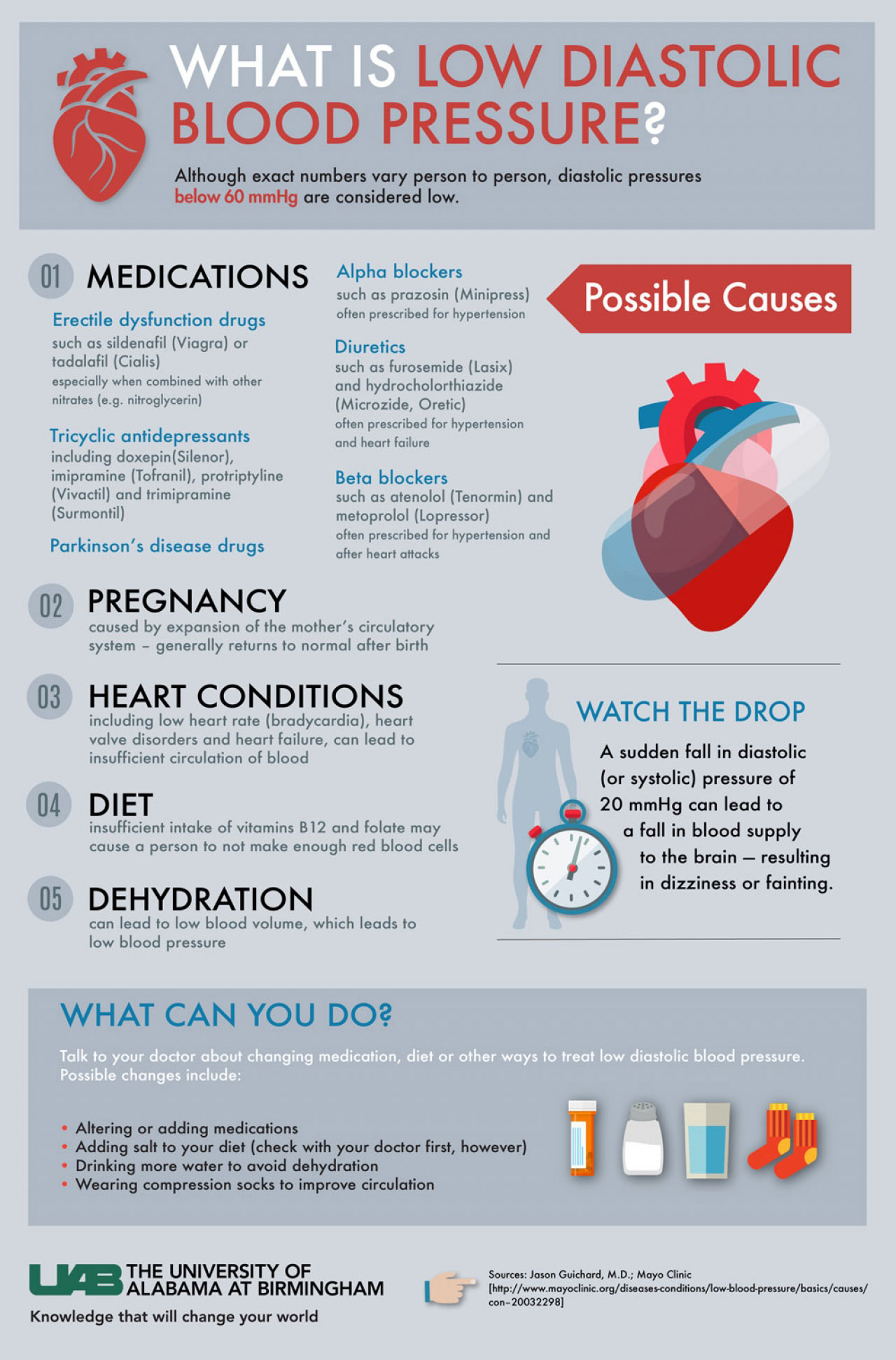
There isn't just one reason your diastolic pressure might be bottoming out. It’s usually a cocktail of biology, age, and maybe the pills you’re taking for something else entirely.
1. The "Stiff Pipe" Problem (Aging)
As we get older, our arteries lose their bounce. They get stiff. In a healthy young person, the aorta acts like a balloon—it expands when the heart pumps and snaps back when the heart rests, keeping the blood moving. This is called the Windkessel effect. But when you’re older and your arteries are stiff like old PVC pipes, they don't snap back. The result? The systolic pressure goes up because the heart has to push harder, and the diastolic pressure craters because there’s no "snap" left in the vessels.
2. Medication Overkill
This is a huge one. Maybe you’re being treated for high blood pressure. Your doctor wants that top number under 130. So, you take your Lisinopril or your Amlodipine. It works! Your systolic drops to 125. But your diastolic, which was already a bit low, slides down to 55. This is "over-treatment." It happens a lot in older patients.
3. Dehydration and the "Empty Tank"
If you don't have enough fluid in your pipes, the pressure drops. Simple physics. This isn't just about not drinking enough water on a Tuesday. It can be chronic. Diuretics (water pills) are notorious for this. They flush out sodium and water to lower your pressure, but sometimes they do the job a little too well.
4. Endocrine and Heart Valve Issues
Sometimes the hardware is the problem. A leaky heart valve—specifically aortic regurgitation—is a classic cause. If the valve doesn't close tightly, blood leaks backward into the heart instead of staying in the arteries to maintain that diastolic pressure. Also, things like an underactive thyroid (hypothyroidism) or Addison’s disease can mess with your vascular tone.
Why doctors are starting to worry about "Too Low"
For a long time, the mantra was "the lower the better." But the J-curve phenomenon changed the conversation.
📖 Related: Average weight of 5'5 female: Why the scale is lying to you
The J-curve suggests that while lowering blood pressure reduces risk, there is a point of diminishing returns where risk starts to climb again. If you push the diastolic pressure below 60 or 70 mmHg, some studies, including data from the ARIC (Atherosclerosis Risk in Communities) study, suggest an increased risk of heart muscle injury.
It’s a bit of a catch-22 for clinicians.
If a patient has a systolic of 150 (dangerous) but a diastolic of 60 (already low), what do you do? If you give them meds to lower the 150, the 60 might drop to 45. That’s a tightrope walk. You’ve got to weigh the risk of a stroke from high systolic pressure against the risk of heart strain from low diastolic pressure.
Common symptoms you shouldn't ignore
A lot of people with low diastolic pressure have zero symptoms. They’re the "lucky" ones, sort of. But for others, the lack of pressure means the brain and limbs aren't getting quite enough "oomph."
- Dizziness when you stand up. This is orthostatic hypotension.
- Fatigue. Just a general sense of being "blah."
- Falls. Especially in the elderly, this is the biggest danger.
- Shortness of breath. If the heart isn't getting enough blood through the coronary arteries, it struggles.
The Role of Lifestyle and Diet
Believe it or not, your salt intake matters here, but not in the way you usually hear. Usually, we're told "Salt is evil! It raises blood pressure!" But if your diastolic is tanking and you’re feeling faint, you might actually need more salt.
And water. Tons of it.
Alcohol is another factor. It’s a vasodilator, meaning it relaxes and widens your blood vessels. Great for a Friday night, maybe, but it can cause your diastolic pressure to slump even further, especially if you’re already prone to it.
Real-world nuances: It’s not always a "Disease"
Sometimes, low diastolic pressure is just... you.
✨ Don't miss: How Long Can the Body Survive Without Oxygen: The Brutal Truth About the Four-Minute Rule
Athletes often have very low resting heart rates and lower-than-average blood pressure. Their hearts are so efficient that they don't need a ton of pressure to move things around. If you’re a marathon runner with a diastolic of 58 and you feel like a superhero, it’s probably not an issue. Context is everything in medicine.
But if you’re 75, sedentary, and feeling dizzy, that 58 is a problem.
What can you actually do about it?
If you’ve looked at your monitor and realized you’re dealing with low diastolic pressure, don't panic. But don't ignore it either.
Review the Meds
Take a look at your pill box. Are you on a diuretic? A beta-blocker? Talk to your doctor about whether the dosage is too aggressive. Sometimes shifting the time of day you take your meds can help.
Compression is Key
It sounds old-fashioned, but compression stockings actually work. They help prevent blood from pooling in your legs, which keeps more volume in your central circulation and can help prop up that diastolic number.
The Salt Strategy
Again, talk to a pro before you start dumping salt on everything. But increasing sodium intake (under supervision) is a standard way to boost blood volume.
Check the Valves
If the low pressure is a new development, getting an echocardiogram is a smart move. You want to make sure your aortic valve isn't acting like a swinging door that won't shut.
Moving forward with low diastolic blood pressure causes
Understanding low diastolic blood pressure causes requires looking at the whole person, not just the machine. It’s about the stiffness of your arteries, the volume of your blood, and the way your heart recovers between beats.
👉 See also: How Do You Measure Your Penis? The Science and Mistakes Most Men Make
If you're noticing a trend of low numbers, start a log. Note when you feel dizzy. Is it after a big meal? (That’s postprandial hypotension). Is it right after your morning meds? This data is gold for your doctor.
Actionable Next Steps:
- Track the Trends: Spend one week logging your blood pressure twice a day—once in the morning and once in the evening. Note any symptoms like lightheadedness or "brain fog."
- Hydration Audit: Aim for 2-3 liters of water a day for three days and see if your diastolic numbers stabilize. Often, "low pressure" is just "low water."
- Medication Review: Schedule a specific "medication review" appointment with your GP. Don't wait for your annual physical. Ask specifically: "Is my diastolic pressure too low for my age and heart health?"
- Positional Awareness: If you feel dizzy, practice "slow standing." Move from lying to sitting, wait 30 seconds, then stand. This gives your nervous system time to catch up.
- Check Your Electrolytes: Ask for a blood panel to check your sodium and potassium levels. An imbalance here is a frequent, easily fixable cause of pressure drops.
The bottom number isn't just a passenger. It’s a vital sign that deserves its own spotlight. Keep an eye on it, keep your fluids up, and don't be afraid to ask your doctor to tweak your regimen if things feel off. High pressure gets all the headlines, but low pressure is where the nuance lives.