You're sitting on the couch after a long flight or maybe just a marathon session at your desk, and you notice it. A dull ache. You figure it’s just a cramped muscle. Maybe you worked out too hard? But then you look down. One calf looks slightly bigger than the other. It’s a bit red. It feels warm to the touch, almost like it’s glowing from the inside. This is exactly how deep vein thrombosis (DVT) starts, and honestly, the way we talk about a blood clot and leg symptoms is often way too clinical to be helpful when you’re actually panicking at 2:00 AM.
Most people expect a blood clot to feel like a lightning bolt of pain. It usually isn't. It’s sneaky. It’s a slow burn that feels remarkably like a "charley horse" that just won't quit. According to the Centers for Disease Control and Prevention (CDC), up to 900,000 Americans are affected by DVT or pulmonary embolisms every year. That’s not a small number. Yet, because the symptoms are so vague—swelling, redness, and a bit of soreness—nearly half of people with a DVT don't even know they have it until the situation turns into a medical emergency.
If you’ve ever wondered why doctors get so intense about "getting up and stretching" on planes, it’s because of stasis. When your blood isn't moving, it starts to thicken. Think of it like a river that stops flowing; eventually, things start to settle and sludge up. In your veins, that sludge becomes a semi-solid mass. If that mass stays in your leg, it's a DVT. If it breaks loose and travels to your lungs, it’s a pulmonary embolism (PE). That's the part that kills.
The Subtle Signs: More Than Just a Cramp
Let's get into the weeds of what a blood clot and leg symptoms actually look and feel like in the real world. Forget the textbook diagrams for a second.
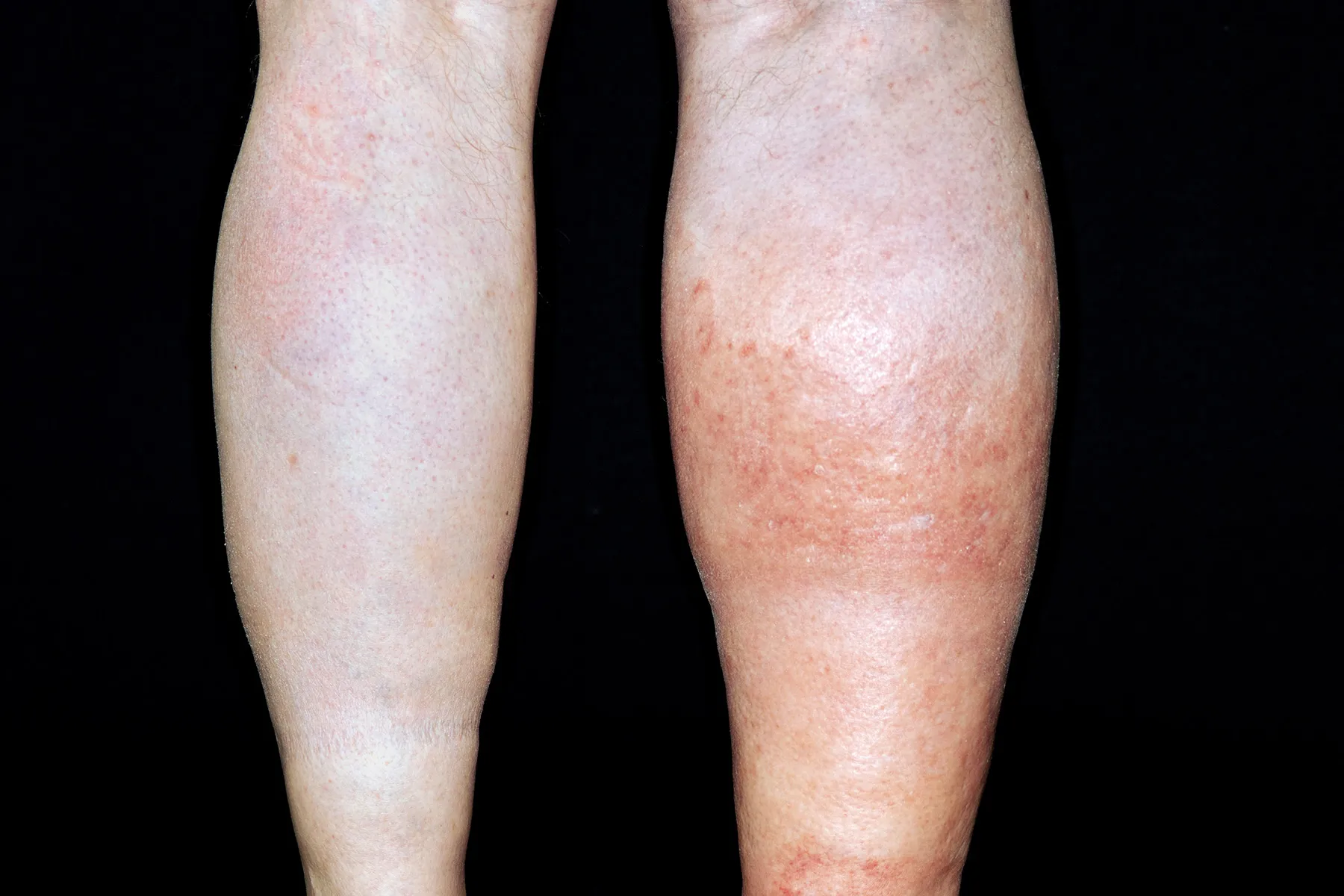
One of the most telling signs is unilateral swelling. That’s just a fancy medical way of saying it happens on only one side. If both your ankles are puffy after eating a bag of salty chips, that’s likely just fluid retention or maybe a heart issue, but it’s rarely a clot. A DVT is a jealous condition; it almost always picks a favorite leg. You might notice your sock leaves a much deeper indentation on your left leg than your right. Or maybe your favorite pair of skinny jeans feels fine on the right side but like a tourniquet on the left.
The pain is different, too. A muscle strain usually hurts more when you move it or touch the specific spot where you tore the fiber. A blood clot feels deeper. It’s an internal pressure. Some patients describe it as a "tightness" in the calf that makes it hard to flex the foot upward. This is sometimes called Homans' sign by old-school doctors, though modern medicine relies way more on ultrasound than just tugging on your toes.
The skin color changes are often overlooked because they can be subtle. It’s not usually "smurf blue" right away. It starts as a slight flush, maybe a dusky or purplish tint that doesn't go away when you elevate the leg. If you press on the red area and the color doesn't "blanch" (turn white) and then snap back to red, or if the area feels significantly warmer than the rest of your skin, your internal alarm bells should be ringing.
💡 You might also like: Is Tap Water Okay to Drink? The Messy Truth About Your Kitchen Faucet
Why Me? The Risk Factors Nobody Mentions
It’s easy to think blood clots only happen to the elderly or people in hospital beds. That's a dangerous myth. Ask any hematologist and they’ll tell you about the 25-year-old marathon runner who ended up in the ER because they had a genetic mutation they didn't know about, like Factor V Leiden.
Genetic predispositions are massive. About 5% to 8% of the U.S. population has one of several genetic risk factors that increase the risk of clotting. Then you have the lifestyle "triad."
- Immobility: This isn't just long-haul flights to Tokyo. It’s the "gamer’s clot." It’s the "coding for 12 hours straight without a bathroom break" clot.
- Hormones: Birth control pills and hormone replacement therapy (HRT) are well-known culprits, especially if you smoke. Estrogen increases the levels of clotting factors in your blood. It’s a known trade-off, but one that requires vigilance.
- Trauma or Surgery: If you’ve recently had knee or hip replacement, you are in the high-risk zone. The body reacts to surgery by revving up its clotting mechanism to stop bleeding—sometimes it just overdoes it.
There is also the "Economy Class Syndrome." When you’re crammed into a middle seat, the edge of the chair can actually compress the veins in your thighs, further slowing down blood flow. It’s a perfect storm. Even being tall—over 6'2"—or being particularly short can change the way blood moves through your extremities.
When the Leg Pain Moves to the Lungs
The absolute scariest part of a blood clot and leg symptoms is the travel. A DVT is a ticking time bomb. If a piece of that clot breaks off, it enters the vena cava, goes through the heart, and gets wedged in the small vessels of the lungs.
This is a Pulmonary Embolism (PE).
Sometimes, the leg symptoms actually disappear or fade just as the lung symptoms start. It’s counterintuitive. You think, "Oh, my leg feels better," and then ten minutes later, you’re gasping for air. If you experience sudden shortness of breath, a sharp chest pain that gets worse when you take a deep breath, or a cough that brings up blood, stop reading this and call 911. Seriously. There is no "waiting it out" with a PE. It is one of the most common causes of preventable hospital deaths worldwide.
📖 Related: The Stanford Prison Experiment Unlocking the Truth: What Most People Get Wrong
Dr. Samuel Goldhaber, a leading expert at Brigham and Women's Hospital, has spent decades trying to increase awareness that PE is often "the great masquerader." It can look like a panic attack, pneumonia, or even a heart attack. The common denominator? That underlying, often ignored leg clot.
Diagnostics: What Happens at the Hospital
If you show up at the ER with a swollen leg, they aren't just going to guess. The process is actually pretty streamlined now.
First, they’ll likely do a D-dimer test. This is a blood test that looks for a specific protein fragment that appears when a blood clot dissolves in the body. If the D-dimer is negative, there’s a very high chance you don't have a clot. It’s a great "rule-out" tool. However, a positive D-dimer doesn't always mean you have a DVT—it just means they need to look closer because things like recent surgery, pregnancy, or even a bad bruise can set it off.
The "gold standard" is the venous ultrasound (duplex ultrasonography). It’s non-invasive. The technician uses a probe to see if the veins in your leg compress when pressure is applied. A healthy vein squishes flat. A vein with a clot stays open like a stiff pipe.
In some cases, if the ultrasound is inconclusive but the suspicion is high, they might go for a CT Venogram or an MRI. But usually, the ultrasound tells the story.
Treatment and Living with a Clot
The word "blood thinner" is a bit of a misnomer. Anticoagulants like Heparin, Warfarin (Coumadin), or the newer Direct Oral Anticoagulants (DOACs) like Eliquis or Xarelto don't actually thin your blood like water. They just change the chemical signaling to prevent new clots from forming and keep the current clot from getting bigger.
👉 See also: In the Veins of the Drowning: The Dark Reality of Saltwater vs Freshwater
Your body actually has to do the hard work of dissolving the clot itself. It's a slow process. It can take months.
During this time, you might be told to wear compression stockings. These aren't the ones your grandma wears; medical-grade graduated compression stockings apply specific pressure at the ankle to shove blood back up toward the heart. They are vital for preventing post-thrombotic syndrome—a chronic condition where the leg stays swollen and painful forever because the valves in the veins were damaged by the clot.
Misconceptions That Can Be Dangerous
There’s a lot of bad advice on the internet. "Just massage the cramp!" No. Absolutely do not do that. If you have a DVT, massaging the area is the fastest way to break a piece of that clot loose and send it straight to your heart. If you have unexplained leg swelling and pain, keep the leg still until you see a professional.
Another myth? "I’m too fit to get a clot." Actually, athletes can be at higher risk due to dehydration (which thickens the blood) and repeated trauma to vessels. Dehydration is a massive, often ignored factor. When you’re dehydrated, your blood volume drops, making what’s left "stickier."
Also, don't assume aspirin is enough. While aspirin has anti-platelet properties, it is generally not considered strong enough to treat an active DVT. You need proper anticoagulation managed by a doctor.
Actionable Steps for Prevention and Safety
If you're worried about blood clot and leg symptoms, there are immediate things you can do to lower your risk profile and stay safe.
- The 2-Hour Rule: Never stay seated for more than two hours. Even if you just stand up and do ten calf raises, you're "pumping" the blood out of those lower extremities.
- Hydrate Like It's Your Job: Keep your blood viscosity low by drinking water consistently. If your urine isn't pale yellow, you’re likely too dry.
- Know Your Family History: Ask your parents or siblings if anyone has ever had a "clot in the leg" or a "lung issue" after surgery. If the answer is yes, tell your doctor. You might need a simple blood test to check for genetic markers.
- Watch the "Big Three": If you see swelling, feel heat, or experience unexplained pain in one leg, get it checked. It’s better to have a "wasted" ER visit for a muscle strain than to ignore a DVT.
- Post-Surgery Movement: If you have surgery, follow the physical therapy plan. They make you walk the same day for a reason. Movement is the best medicine for your veins.
If you are currently experiencing one-sided leg swelling that is accompanied by a "tight" feeling or redness, you should seek medical attention within the next few hours. While it might be a simple strain, the risk of a pulmonary embolism makes this one of the few medical scenarios where "better safe than sorry" is a literal life-saving mantra. Tell the triage nurse specifically that you are concerned about a deep vein thrombosis; this often triggers a faster diagnostic path than simply saying "my leg hurts."