You’re staring at a grainy, black-and-white image of your own femur meeting your tibia. Maybe there’s a circle drawn by a radiologist or a jagged line that looks like a lightning bolt. It's scary. When you search for knee pictures knee pain, you’re usually looking for a "smoking gun"—that one specific tear or bone spur that explains why it hurts to walk down the stairs or why your knee makes a sound like gravel in a blender. But here is the weird, honest truth that most surgeons won't lead with: your pictures might not actually be the reason you hurt.
The medical world has a bit of an obsession with "VOMIT." That stands for Victim of Modern Imaging Technology. It’s a real term used by clinicians to describe patients who get an MRI, see a scary-looking report, and suddenly feel ten times worse because they think their knee is "bone on bone."
Honest talk? Your knee might look like a train wreck on a screen but feel totally fine, or it might look pristine while you’re hobbling in agony.
The Disconnect Between the Image and the Ache
If we took 100 people off the street who have zero knee pain and put them through an MRI machine, the results would shock you. A landmark study published in the British Journal of Sports Medicine found that a massive percentage of asymptomatic adults—people living their best lives with no pain—have "abnormal" knee scans. Specifically, about 43% of people over the age of 40 have meniscal tears they don't even know about.
If you’re looking at knee pictures knee pain results and seeing a "frayed meniscus," don't panic. It might just be the "wrinkles of the inside," as many physical therapists call it. Just like we get gray hair and skin folds as we age, our joints change. A scan is just a snapshot in time; it doesn't show how your muscles are firing, how you move, or how sensitive your nervous system has become.
Let's get into the specifics. There are three main types of "knee pictures" you’ll encounter: X-rays, MRIs, and Ultrasounds.
X-rays are the old school standard. They’re great for bones. If you have a fracture or severe osteoarthritis where the space between the bones has basically vanished, an X-ray is your best friend. But it can’t see ligaments. It can’t see the meniscus. If your doctor only orders an X-ray and tells you "everything is fine," but you feel like your knee is giving way, they’re missing half the story.
Then there’s the MRI. This is the gold standard for soft tissue. It’s a giant magnet that captures slices of your anatomy. It’s incredibly detailed—sometimes too detailed. It picks up every tiny cyst, every minor bit of inflammation, and every slight thinning of the cartilage.
👉 See also: Sudafed PE and the Brand Name for Phenylephrine: Why the Name Matters More Than Ever
Why Your MRI Report Sounds Like a Horror Movie
Reading an MRI report is an exercise in anxiety. You’ll see words like "degenerative," "extrusion," "maceration," and "full-thickness tear."
Basically, radiologists are paid to find anything that isn't "perfect." But perfection in a human knee is rare after the age of 25. If you're a runner, an athlete, or just someone who has lived an active life, your knee pictures knee pain results are going to show wear.
Take the ACL, for example. We’ve all seen the dramatic slow-motion replays of athletes tearing their ACL. On a scan, a torn ACL looks like a disorganized mess of gray fibers. It’s clear. But did you know that some people—often called "copers"—have completely torn ACLs and still play high-level sports because their surrounding muscles are so strong? The picture shows a "broken" knee, but the person functions perfectly.
Contrast that with Patellofemoral Pain Syndrome (PFPS), often called "Runner's Knee." You could have excruciating pain right under your kneecap, yet your X-ray and MRI come back looking flawless. Why? Because the pain isn't coming from a structural break; it's coming from how the kneecap tracks in its groove or because the nerves in that area are hypersensitive.
Seeing the Pain: Inflammation and Effusion
Sometimes the "picture" isn't a medical scan at all. It's what you see in the mirror.
"Water on the knee" or joint effusion is a visual cue that something is wrong. When the knee swells, it loses its definition. You lose those little dimples on the sides of the kneecap. This is actually your body’s defense mechanism. The joint produces extra synovial fluid to "cushion" what it perceives as an injury.
If you’re comparing your knee to knee pictures knee pain online to see if your swelling is "normal," look for the "stroke test." You basically try to push the fluid from one side of the kneecap to the other. If a bulge appears on the opposite side, you’ve got a positive effusion.
✨ Don't miss: Silicone Tape for Skin: Why It Actually Works for Scars (and When It Doesn't)
Is swelling bad? Not necessarily. It’s just information. It tells you the joint is "angry." It doesn't tell you why it's angry. You could have swelling from a traumatic ligament tear, or you could have it because you did 500 lunges after not working out for six months.
The Cartilage Myth
We need to talk about the "bone on bone" phrase. It’s perhaps the most damaging phrase in all of orthopedics.
When a doctor looks at knee pictures knee pain and tells a patient they are "bone on bone," the patient often stops moving. They become terrified that every step is grinding their joints into dust.
Here’s the reality: cartilage doesn't have nerves. You can't actually "feel" your cartilage wearing down. The pain comes from the bone underneath (which is highly innervated), the synovium (the lining of the joint), or the surrounding tendons. Furthermore, "bone on bone" is rarely absolute. There is almost always some microscopic layer of protection, and more importantly, movement actually helps lubricate what’s left.
Using Pictures the Right Way
So, should you ignore your scans? No. That would be reckless.
Scans are vital for ruling out the big stuff: tumors, infections, or acute fractures that need immediate surgery. They are also helpful if you’ve tried conservative treatment (like physical therapy) for three months and nothing has changed.
But if you get a scan before you’ve tried moving, you’re setting yourself up for a psychological trap. You’ll start identifying as your MRI report. "I'm the guy with the Grade 3 Meniscal Tear," rather than "I'm the guy whose knee hurts when I squat."
🔗 Read more: Orgain Organic Plant Based Protein: What Most People Get Wrong
Dr. Howard Luks, a renowned orthopedic surgeon and sports medicine expert, often talks about how we treat people, not pictures. He notes that the decision for surgery should be based on your "clinical presentation"—meaning your strength, your range of motion, and your pain levels—rather than just what shows up on the film.
What to Look for in Your Own Knee Photos
If you are taking photos of your own knee to track progress or show a doctor, do these three things:
- Compare sides: Always take a photo of both knees together. Asymmetry is the biggest clue for a clinician.
- Weight-bearing vs. Non-weight-bearing: Take a photo while standing and one while sitting. Does the alignment change? Does a lump appear only when you put weight on it? (This could indicate a Baker's Cyst behind the knee).
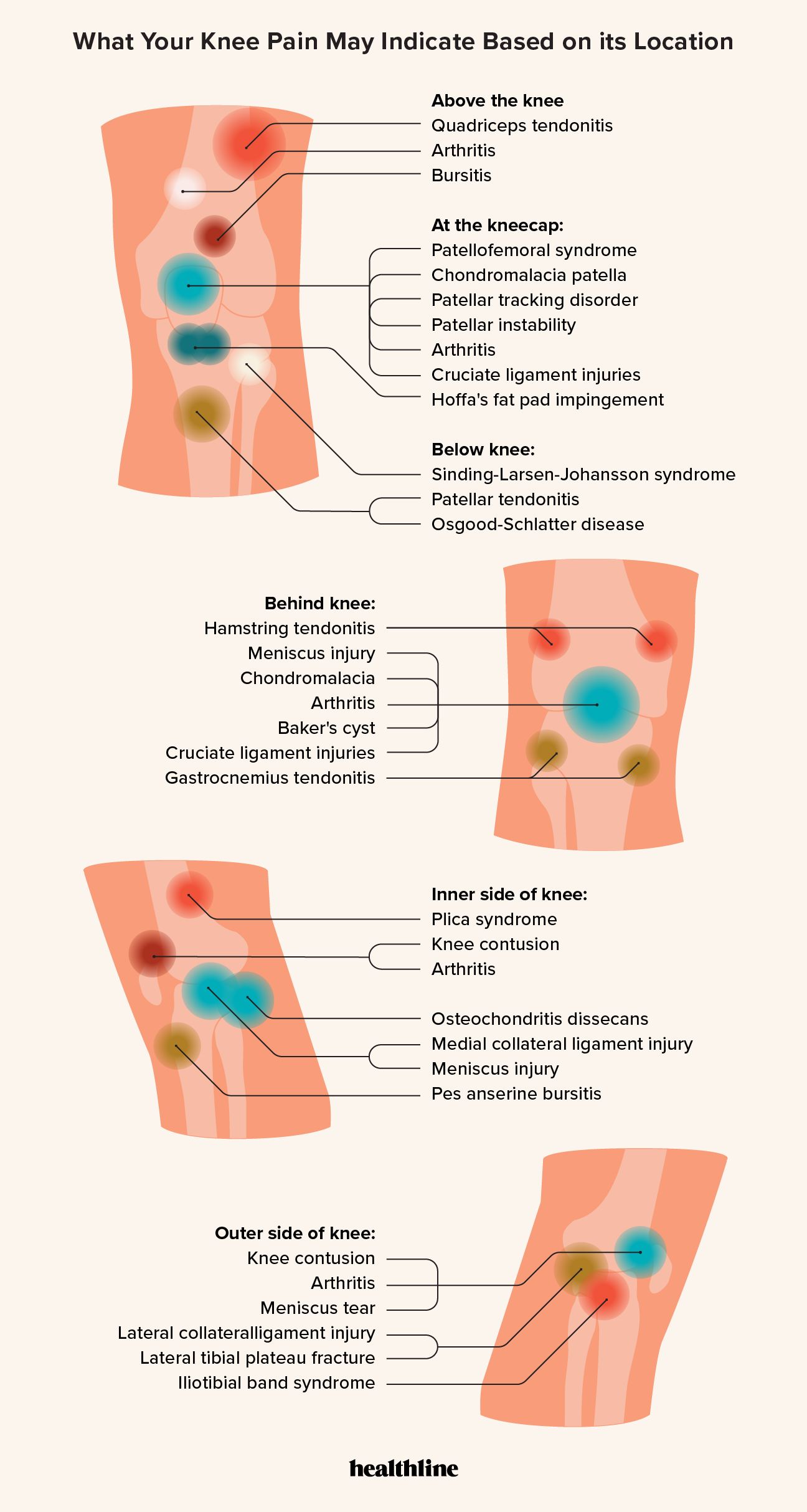
- The "Point" Test: Instead of saying "it hurts everywhere," take a photo of yourself pointing with one finger to the exact spot of maximum pain. If it’s right on the joint line, it’s more likely a meniscus issue. If it’s on the bony bump below the kneecap, it’s likely Osgood-Schlatter (in younger people) or patellar tendonitis.
Actionable Steps: Moving Beyond the Image
If you’re currently obsessed with your knee pictures knee pain results, here is how you actually get better.
First, stop Googling "meniscus tear surgery." Instead, Google "knee rehabilitation exercises for [your specific symptom]."
Second, find a physical therapist who doesn't even look at your MRI report until the end of the first session. You want someone who assesses how you move first. If they can get you to do a split squat without pain by slightly adjusting your hip position, then your "torn meniscus" isn't the primary driver of your pain—your mechanics are.
Third, load is medicine. The old advice of "RICE" (Rest, Ice, Compression, Elevation) is largely being phased out in favor of "PEACE & LOVE." The "L" stands for Load. Your cartilage and tendons need gradual, progressive pressure to heal and get stronger. Avoiding movement because of a scary picture actually makes the joint more brittle and sensitive.
Fourth, check your "upstream" and "downstream" joints. Knee pain is rarely just a knee problem. It’s often a "weak hip" problem or a "stiff ankle" problem. The knee is caught in the middle, taking the brunt of the force because the joints above and below aren't doing their jobs.
Summary of Next Steps:
- De-catastrophize: Remind yourself that "abnormal" findings on scans are normal for aging humans.
- Test your function: Can you balance on one leg? Can you heel-walk? If you can, your "structural damage" might not be as severe as the picture looks.
- Focus on the "Big Three": Quad strength, hip stability, and ankle mobility.
- Monitor "The 24-Hour Rule": If an exercise hurts while you're doing it, that's okay (up to a 3/10 pain). If that pain is still worse 24 hours later, you overdid it. Scale back, but don't stop.
- Get a second opinion: If a surgeon looks at a scan and recommends surgery within five minutes without testing your strength or asking about your goals, walk out.
Your knees are incredibly resilient. They are not made of glass. Even if the knee pictures knee pain search results look daunting, remember that the image is just the map—it is not the territory. You can change how your knee feels without ever changing how it looks on an X-ray. Strength, movement, and a bit of patience are usually far more effective than trying to "fix" a picture.